Anorexia Nervosa: Difference between revisions
No edit summary |
No edit summary |
||
| Line 85: | Line 85: | ||
*'''Athletics''': Individuals who participate in any sport that emphasizes a thin build or has weight classifications is more likely to develop an eating disorder. Again those sports that show higher rates of anorexia nervosa include ballet, gymnastics, long-distance running, figure skating, wrestling, body-building, and diving. <ref name="Goodman">Goodman, Catherine C. and Fuller, Kenda S. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.</ref> | *'''Athletics''': Individuals who participate in any sport that emphasizes a thin build or has weight classifications is more likely to develop an eating disorder. Again those sports that show higher rates of anorexia nervosa include ballet, gymnastics, long-distance running, figure skating, wrestling, body-building, and diving. <ref name="Goodman">Goodman, Catherine C. and Fuller, Kenda S. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.</ref> | ||
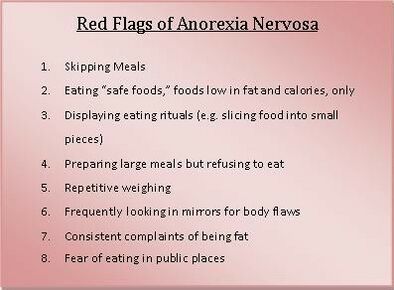
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
*<br> | |||
[[Image:Hospitalization.jpg|center|Hospitalization.jpg]] | [[Image:Hospitalization.jpg|center|Hospitalization.jpg]] | ||
. | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
Revision as of 12:38, 9 August 2021
Original Editors - Brittney Kerchief from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Brittney Kerchief, Lucinda hampton, Admin, Simisola Ajeyalemi, Laura Ritchie, Kim Jackson, Tony Lowe, Elaine Lonnemann, Wendy Walker, George Prudden, WikiSysop and Vidya Acharya
Introduction[edit | edit source]
Anorexia nervosa is an eating disorder defined by restriction of energy intake relative to requirements, leading to a significantly low body weight. Patients will have an intense fear of gaining weight and distorted body image with the inability to recognize the seriousness of their significantly low body weight.[1]
The long‐term prognosis is often poor, with severe developmental, medical and psychosocial complications, high rates of relapse and mortality.[2]
Epidemiology[edit | edit source]
The lifetime prevalence of anorexia nervosa is 0.66-1.9% based on geographical location, with a higher prevalence in developed countries.
Females are ten times more likely to be diagnosed with anorexia nervosa compared to men.
The lifetime incidence of anorexia nervosa has increased from 0.1 to 5.4 per 100,000 over the last fifty years. In females aged 15-19 years, the incidence has increased from 56.4 to 109 per 100,000 person-years.[3]
Pathophysiology[edit | edit source]
Studies demonstrate biologic factors play a role in the development of anorexia nervosa in addition to environmental factors. Genetic correlations exist between educational attainment, neuroticism, and schizophrenia. Patients with anorexia nervosa have altered brain function and structure there are deficits in neurotransmitters dopamine (eating behavior and reward) and serotonin (impulse control and neuroticism), differential activation of the corticolimbic system (appetite and fear), and diminished activity among the frontostriatal circuits (habitual behaviors). Patients have co-morbid psychiatric disorders such as major depressive disorder and generalized anxiety disorder.[1]
Clinical Presentation[edit | edit source]
The Diagnostic and Statistical Manual of mental disorders (DSM-5) recognises the following criteria for the diagnosis of anorexia nervosa
- a restriction of caloric intake
- low body weight relative to age, sex and health
- unjustified fear of weight gain
- body dysmorphia
Along with these, numerous signs may be observed and they include - but are not limited to - the following:
- lanugo hair and/or alopecia
- amenorrhoea (from suppression of the gonadal axis)
- dental caries (from purging)
- orthostatic hypotension or tachycardia
- resting bradycardia
- halitosis
- lagophthalmos
- purpurae[3]
Two sub-types of anorexia nervosa have been recognized by the Diagnostic and Statistical Manual of Mental Disorders. These sub-types include:
- Restricting subtype is characterized by an individual with anorexia nervosa who has not regularly taken part in bingeing or purging behaviors during the current episode.
- Bingeing and purging behaviors include the use of laxatives, diuretics, enemas, and self-induced vomiting to restrict weight gain. Binge-eating-purging subtype is characterized by an individual who has regularly taken part in binge-eating or purging behaviors in the current episode of anorexia nervosa. [4][5]
Associated Co-morbidities[edit | edit source]
Death is the most devastating co-morbidity present with this eating disorder and most commonly occurs due to symptoms of starvation or suicide. Medical conditions typically causing death consist of abnormal heart rhythms and imbalances of electrolytes. Mortality rates are as high as 5.9% in anorexia nervosa diagnoses.
Co-morbid conditions present in individuals with anorexia nervosa may also include "major depressive disorder (50-75% of cases), sexual abuse (20-50% of cases), obsessive compulsive disorder (25% of cases), substance abuse (12-18% of cases), and bipolar disorder (4-13% of cases)". [4]
Anemia, mitral valve prolapse, osteoporosis, and stress fractures are examples of co-morbidities that may be present with any eating disorders. Many individuals with anorexia nervosa often develop other types of eating disorders as well. Up to 50% of individuals with anorexia nervosa develop characteristics of bulimia nervosa over the span of their lifetime.
Treatment[edit | edit source]
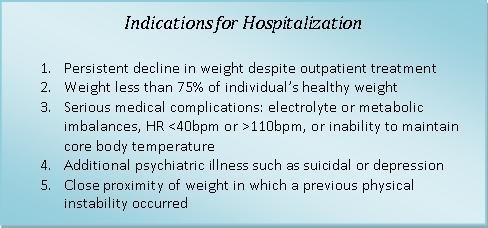
Treatment for anorexia nervosa is centered on nutrition rehabilitation and psychotherapy. Patients who need inpatient treatment have the following characteristics:
- Existing psychiatric disorders requiring hospitalization
- High risk for suicide (intent with highly lethal plan or failed attempt)
- Lack of support system (severe family conflict or homelessness)
- Limited access (lives too far away to participate in a daily treatment program)
- Medically unstable (bradycardia, dehydration, hypoglycemia or poorly controlled diabetes, hypokalemia or other electrolyte imbalances indicative of refeeding syndrome, hypothermia, hypotension,, organ compromise requiring acute treatment)
- Poorly motivated to recover (uncooperative, preoccupied with intrusive thoughts)
- Purging behaviors that are persistent, severe, and occur multiple times a day
- Severe anorexia nervosa (less than 70% of ideal body weight or acute weight loss with food refusal)
- Supervised feeding and/or specialized feeding (nasogastric tube) required
- Unable to stop compulsively exercising (not a sole indication for hospitalization).
Outpatient treatment includes intensive therapy (2 to 3 hours per weekday) and partial hospitalization (6 hours per day). Pediatric patients benefit from family-based psychotherapy to explore underlying dynamics and restructure the home environment.
Refeeding syndrome can occur following prolonged starvation. As the body utilizes glucose to produce molecules of adenosine triphosphate (ATP), it depletes the remaining stores of phosphor.
Also, glucose entry into cells is mediated by insulin and occurs rapidly following long periods without food. Both cause electrolyte abnormalities such as hypophosphatemia and hypokalemia, triggering cardiac and respiratory compromise. Patients should be followed carefully for signs of refeeding syndrome and electrolytes closely monitored.
Pharmacotherapy is not used initially. For acutely ill patients who do not respond to initial treatment, olanzapine is a first-line medication. Other antipsychotics have not demonstrated similar effects on weight gain. For patients who are not acutely ill but have co-morbid psychiatric conditions such as generalized anxiety disorder or major depressive disorder, combination therapy with selective serotonin reuptake inhibitors (SSRIs) and therapy is best. Patients who do not respond to SSRIs may need a second-generation antipsychotic. Tricyclic antidepressants (TCAs) are less-preferred due to concerns about cardiotoxicity, especially in malnourished patients. Bupropion is contraindicated in patients with eating disorders due to the increased risk of seizures[1]
Nutritional therapy guidelines include weight gain of .9 - 1.4 kg per week for inpatient treatment and .22 - .45 kg per week for outpatient treatment. Initially daily caloric goals should reach 1000-1600 kcal in divided meals and bathroom use should be restricted for two hours following each meal. Once a healthy weight is maintained stretching can be reintroduced followed by aerobic exercise with supervision and counselling on proper exercise guidelines. Cite error: The opening <ref> tag is malformed or has a bad name
Cause / Risk Factors[edit | edit source]
- Biological: Young women and men are at an increased risk to develop anorexia nervosa if the individual has a biological sibling or mother with anorexia nervosa. According to current research, children of patients with anorexia nervosa have a tenfold increased risk for developing the eating disorder. [6][4] An area on chromosome one has also been associated with increased risk for development of anorexia nervosa. [6] Varying amounts of the chemical serotonin have shown evidence in playing a role in anorexia nervosa. All of the above show a definite genetic involvement in patients with anorexia nervosa.
- Genetics: 50-80% of the risk for anorexia and bulimia is genetic.[7] According to research, families in which the condition is reported in more than one member, a genetic predisposition to AN may be a factor for the development of anorexia. Although the gene(s) responsible for the disorder have not yet been identified, research has shown that certain loci on chromosomes 1, 2, and 13 may be involved in the development of Anorexia. Recently, a study using targeted sequencing implicated the gene epoxide hydrolase 2 as increasing the risk of developing anorexia.[8]
- Psychological: Individuals with anorexia nervosa often portray low self-esteem, low self-confidence, extreme perfectionist qualities, and obsessive-compulsive behaviors. Higher rates of eating disorders are also found in individuals who were teased about their weight at a younger age. Strict weight control can be used as a means to combat feelings of inadequacy or identity confusion.
- Sociocultural: A correlation between prevalence rates of anorexia nervosa and modern western cultures have been evidenced in research today. Modern western cultures are theorized to emphasize importance of thin appearance and associate power or wealth with thinness. [4][6] Adolescents who feel pressure from families or peers to appear unrealistically thin are at an increased risk for developing anorexia nervosa.
- Familial: Families who struggle with resolving internal conflicts, constantly overprotecting their children, limit the autonomy of their children, or expect extraordinarily high achievements place the children at a higher risk for developing anorexia nervosa as shown in research trends. [5]
- Athletics: Individuals who participate in any sport that emphasizes a thin build or has weight classifications is more likely to develop an eating disorder. Again those sports that show higher rates of anorexia nervosa include ballet, gymnastics, long-distance running, figure skating, wrestling, body-building, and diving. [9]
.
Physical Therapy Management[edit | edit source]
Physical Therapy is an integral part in rehabilitation of patients with anorexia nervosa once stretching and exercise is reintroduced. A health care provider who has extensive knowledge of proper exercise guidelines and how to monitor physical signs of fatigue and vitals is needed to treat these patients. These skills are important to help the patient learn to monitor levels of fatigue and heart rate in order to prevent them from over exercising or exercising to the point of exhaustion. Patients with anorexia nervosa are also more susceptible to orthostatic hypotension, bradycardia, and muscle cramping due to malnutrition and low level caloric diets. A health care provider, such as a physical therapist, is the best trained professional to monitor and respond to these medical conditions.
A physical therapist can also be beneficial during the screening process because they are educated in their professional programs on how to recognize the signs and symptoms of this disorder. A therapist may be the first provider to notice signs and symptoms present with this disorder. For example, during a cervical exam the therapist may note edema in the face or salivary glands or overuse injuries like stress fractures from excessively exercising.
When creating exercise programs for these individuals, physical therapists must take into account bone density levels, orthostatic hypotension, cardiac status, and lab values. The program must be adjusted in order to protect the individual from physical harm or becoming medically unstable. Exercise is not recommended if the patients body mass index is less than 18 kg/m2, and therefore is not introduced until the individual can maintain a healthy weight and is medically stable. The ideal exercise program should include elements of stretching, light upper body weights, breathing exercises, and aerobic exercise. It is very important for the physical therapist to set upper limits on repetitions, sets, or minutes in order to prevent the individual from over exercising. Encouraging the individual to focus on the positive effects of exercise on overall health and not weight is equally important for the physical therapist. [9]
Other Management[edit | edit source]
- Electroconvulsive therapy has been used in severe cases of anorexia nervosa with positive effects in weight gain and improving affect. [10]
- Yoga has been proven to be effective as an adjunct to treatment for anorexia nervosa to increase self-awareness and self-reflection. [11]
Differential Diagnosis [4][edit | edit source]
Eating Disorders:
- Bulimia Nervosa
- Food Avoidance Emotional Disorder
- Pervasive Refusal Syndrome
- Functional Dysphagia
Medical Illnesses:
- Brain tumors or malignancies
- Gastrointestinal Disease
- Acquired Immunodeficiency Syndrome (AIDS)
Psychiatric Disorders:
- Depression
- Schizophrenia
- Somatization Disorder
Case Reports[edit | edit source]
- Strategies used by physical therapists in the U.S. for treatment and prevention of the female athlete triad.
- Prevalence of the Female Athlete Triad Syndrome Among High School Athletes
- Mitsuaki Tokumura, Shigeki Yoshiba, Tetsuya Tanaka, Seiichiro Nanri, Hisako Watanabe. Prescribed exercise training improves exercise capacity of convalescent children and adolescents with anorexia nervosa. European Journal of Pediatrics [serial online]. 2003;162:430-1. Available from: ProQuest Health and Medical Complete. Accessed April 8, 2010, Document ID: 1322842551.
- The female athlete triad: an emerging role for physical therapy
- Severe Anorexia Nervosa, Co-occurring Major Depressive Disorder and Electroconvulsive Therapy as Maintenance Treatment: A Case Report
- Unique challenges for appropriate management of a 16-year-old girl with superior mesenteric artery syndrome as a result of anorexia nervosa: a case report
- Family-Based Treatment of a 17-Year-Old Twin Presenting with Emerging Anorexia Nervosa: A Case Study Using the “Maudsley Method”
Resources[edit | edit source]
- National Association of Anorexia Nervosa and Associated Disorders
- The Alliance for Eating Disorders Awareness
- Eating Disorders Anonymous (EDA)
- Eating Disorder Referral and Information Center
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Moore CA, Bokor BR. Anorexia Nervosa. [Updated 2021 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available:https://www.ncbi.nlm.nih.gov/books/NBK459148/ (accessed 9.8.2021)
- ↑ Fisher CA, Skocic S, Rutherford KA, Hetrick SE. Family therapy approaches for anorexia nervosa. Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No.: CD004780. DOI: 10.1002/14651858.CD004780.pub4. Available: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004780.pub4/full Accessed 09 August 2021.
- ↑ 3.0 3.1 Radiopedia Anorexia Nervosa Available:https://radiopaedia.org/articles/anorexia-nervosa (accessed 9.8.2021)
- ↑ 4.0 4.1 4.2 4.3 4.4 Franco, Kathleen N. Eating Disorders. Cleveland Clinic Center for Continuing Education Website. 2009. Available at: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/psychiatry-psychology/eating-disorders/. Accessed February 20, 2010.
- ↑ 5.0 5.1 Mitchell, James E. Outpatient Treatment of Eating Disorders: A Guide for Therapists, Dietitians, and Physicians. Minneapolis, MN, USA: University of Minnesota Press. 2001. p 14-27.
- ↑ 6.0 6.1 6.2 Mayo Clinic Staff. Anorexia Nervosa. Mayo Clinic Website. 2010. Available at: http://www.mayoclinic.com/health/anorexia/DS00606. Accessed February 20, 2010.
- ↑ Trace, S. E., Baker, J. H., Peñas-Lledó, E., & Bulik, C. M. (2013). The genetics of eating disorders. Annual Review of Clinical Psychology, 9, 589-620.
- ↑ Scott-Van Zeeland AA, Bloss CS, Tewhey R, Bansal V, Torkamani A, et al. (2014) Evidence for the role of EPHX2 gene variants in anorexia nervosa. Mol Psychiatry 19: 724–732. pmid:23999524
- ↑ 9.0 9.1 Goodman, Catherine C. and Fuller, Kenda S. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.
- ↑ Poutanen O., et al. Severe anorexia nervosa, co-occurring major depressive disorder and electroconvulsive therapy as maintenance treatment: a case report. Cases Journal [serial online]. 2009;2:9362. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2804009/?tool=pubmed.
- ↑ Douglass L. Yoga as an intervention in the treatment of eating disorders: does it help. Eat Disord. 2009 Mar-Apr;17(2):126-39.