Anatomy of the Human Heart
Original Editor - Uchechukwu Chukwuemeka
Top Contributors - Uchechukwu Chukwuemeka, Lucinda hampton, Kim Jackson, Joao Costa, George Prudden, Sai Kripa, Adam Vallely Farrell and Admin
Introduction[edit | edit source]
The heart is a muscular pump that serves two functions; to collect oxygen-poor blood from the tissues of the body and pump this blood to the lungs to pick up oxygen and release carbon dioxide and to collect oxygen-rich blood from the lungs and pump this blood to all of the tissues of the body[1].
It is important to note that, the blood pumped by the heart also circulates many other important substances[1][2] such as:
1. Nutrients from digestion are collected from the small intestine and pumped through the circulatory system to be delivered to all cells of the body.
2. Hormones are produced from one type of tissues and distributed to all cells of the body. The circulatory system carries waste materials (salts, nitrogenous wastes, and excess water) from cells to the kidneys, where they are extracted and passed to the bladder.
3. The pumping of interstitial fluid from the blood into the extracellular space is an important function of the heart. Excess interstitial fluid is then returned to the circulatory system via the lymphatic system.
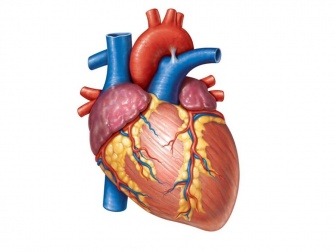
Anatomy[edit | edit source]
The general shape and orientation of the heart are that of a pyramid that has fallen over and is resting on one of its sides. Placed in the thoracic cavity, the apex of this pyramid projects forward, downward, and to the left, whereas the base is opposite the apex and faces in a posterior direction[3][2][4].
The average adult’s heart is about 5.5 inches (14 centimeters) long and 3.5 inches (9 centimeters) wide, or approximately the size of one’s fist and also varies with body size. In an infant, the heart is about a thirtieth of total body weight. In an average adult, the heart is about one three-hundredth of total body weight; this equals about 11 ounces (310 grams) in males and 8 ounces (225 grams) in females[5].
Location of the Heart[edit | edit source]
The heart is roughly in a plane that runs from the right shoulder to the left nipple. It lies in the protective thorax, posterior to the sternum and costal cartilages, and rests on the superior surface of the diaphragm. The heart is located between the two lungs in the space referred to as the mediastinum ("that which stands in the middle"). The human heart assumes an oblique position in the thorax, one-third of the heart is located on the right side, while two thirds is located on the left side of midline. The base is located below the third rib as it approaches the sternum (note that the sternal angle occurs at the level of the second rib). The base is directed superiorly to the right of midline and posterior. The pointed apex projects to the left of midline and anterior. Thus, the heartbeat can be most easily palpated at the left fifth intercostal space, 8-9 cm from the midsternal line (just inferior to the left nipple).[6][4]
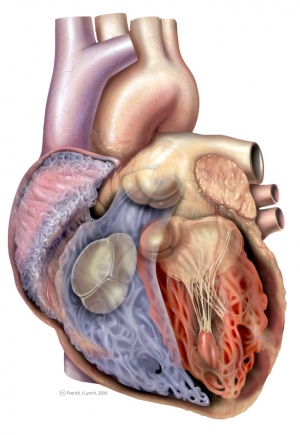
Layers of the Heart Walls[edit | edit source]
The heart wall consists of three layers[1][2][4]:
Epicardium - the outer layer of the wall of the heart and is formed by the visceral layer of the serous pericardium.
Myocardium - the muscular middle layer of the wall of the heart and is composed of three discernable layers of muscle that are seen predominantly in the left ventricle and inter-ventricular septum alone. It includes
· a subepicardial layer,
· a middle concentric layer
· a subendocardial layer.
The rest of the heart is composed mainly of the subepicardial and subendocardial layers. The myocardium also contains important structures such as excitable nodal tissue and the conducting system.
Endocardium - the innermost layer of the heart is formed of the endothelium and subendothelial connective tissue
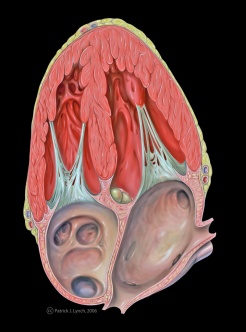
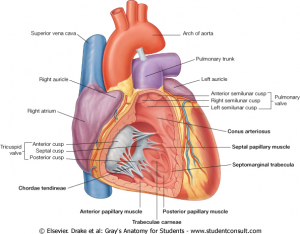
Chambers of the Heart[edit | edit source]
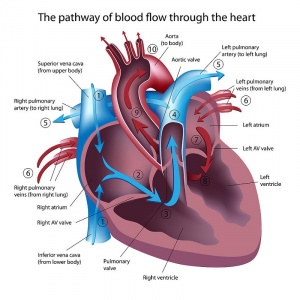
The heart functionally consists of two pumps separated by a partition. The right pump receives deoxygenated blood from the body and sends it to the lungs. The left pump receives oxygenated blood from the lungs and sends it to the body. Each pump consists of an atrium and a ventricle separated by a valve.The heart is divided into four distinct chambers with muscular walls of different thickness
The left atrium (LA) and right atrium (RA) are small, thin walled chambers located just above the left ventricle (LV) and right ventricle (RV), respectively. The ventricles are larger thick-walled chambers that perform most of the work. The atria receive blood from the venous system and lungs and then contract and eject the blood into the ventricles.
The left Atrium[edit | edit source]
The left atrium receives oxygenated blood from the lungs via the left and right pulmonary veins. The pulmonary veins enter the heart as two pairs of veins inserting posteriorly and laterally into the left atrium. In addition, the smallest (Thebesian) veins drain deoxygenated blood from the atrial myocardium directly into the atrium. The left atrium is found midline, posterior to the right atrium and superior to the left ventricle. Anteriorly, a left atrial appendage (auricle) extends over the atrioventricular (coronary) sulcus. The walls of the atrial appendage are pectinate, and the walls of the left atrium are smooth. It discharges into the left ventricle through the mitral valve[7][8]
The right Atrium[edit | edit source]
The interior of the right atrium has three anatomically distinct regions. First, the posterior portion of the right atrium has a smooth wall and is referred to as the sinus venarum.; Secondly, the wall of the anterior portion of the right atrium is lined by horizontal, parallel ridges of muscle bundles that resemble the teeth of a comb, hence the name pectinate muscle (pectin = "a comb,"); and thirdly, the atrial septum . It receives both the superior and inferior venae cavae and the coronary sinus. It also contains the fossa ovalis, the sinoatrial node, and the atrioventricular node. The inferior border of the right atrium contains the opening or ostium of the inferior vena cava and the os or ostium of the coronary sinus. On the medial side of the right atrium, the interatrial septum (atrial septum) has interatrial and atrioventricular parts.
On the "floor" of the right atrium is the atrioventricular portion of the atrial septum, which has muscular and membranous components. At the anterior and inferior aspect of the atrial septum, the tricuspid valve annulus (annulus = "ring") is attached to the membranous septum.
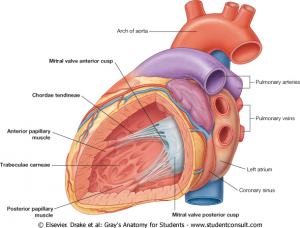
The left ventricle
It pumps blood throughout the body via the aorta. Most of the left lateral surface of the heart is formed by the left ventricle, also forming part of the inferior and posterior surface. Abundant trabeculae carneae characterize the walls of the left relatively; LV apex is less trabeculated than the RV apex.However, in contrast to the right ventricle, the muscular ridges tend to be relatively fine and the myocardium in the wall of the left ventricle is three times thicker; thickest towards the base and thinnest towards the apex. The interventricular septum appears from within the left ventricle to bulge into the right ventricle; this creates a barrel-shaped left ventricle. It is made of an inlet portion comprised of mitral valve apparatus, subaortic outflow portion and a trabeculated apical zone[7][9].
The right ventricle
It pumps blood to the lungs through the pulmonary trunk and arteries. It comprises of an inlet and outflow segments. The Inlet extends from tricuspid annulus to the insertions of the papillary muscles. Abundant, coarse trabeculae carneae ("beams of meat") characterize the walls of the right ventricle.
Trabeculae carneae are analogous to pectinate muscle of the right atrium (as bundles of myocardium) . The outflow tract, conus arteriosus ("arterial cone") or infundibulum ("funnel"), carries blood out of the ventricle in an anterior-superior direction and is relatively smooth walled. A component of the conus arteriosus forms part of the interventricular septum. This small septum, the infundibular (conal) septum, separates the left and right ventricular outflow tracts and is located just inferior to both semilunar valves[7].
Heart Valves[6][4][edit | edit source]
The heart has the Four valves.
Pulmonary Valve - At the apex of the infundibulum, the outflow tract of the right ventricle, the opening into the pulmonary trunk is closed by the pulmonary valve, which consists of three semilunar cusps with free edges projecting upward into the lumen of the pulmonary trunk thus prevents the back flow of blood as it is pumped from the right ventricle to the pulmonary artery. The cusps are named the left, right and anterior semilunar cusps, relative to their fetal position before rotation of the outflow tracks from the ventricles is complete. Each cusp forms a pocket-like sinus; a dilation in the wall of the initial portion of the pulmonary trunk.[4]
Tricuspid Valve - The right atrioventricular orifice is closed during ventricular contraction by the tricuspid valve (right atrioventricular valve) thus prevents the back flow of blood as it is pumped from the right atrium to the right ventricle. It’s named tricuspid valve because it made up of three cusps or leaflets. The base of each cusp is secured to the fibrous ring that surrounds the atrioventricular orifice. The naming of the three cusps, the anterior, septal, and posterior cusps, is based on their relative position in the right ventricle.
Aortic Valve - The opening from the left ventricle into the aorta is closed by the aortic valve thus prevents the back flow of blood as it is pumped from the left ventricle to the aorta. The aortic vestibule is continuous superiorly with the ascending aorta. It consists of three semilunar cusps with the free edge of each projecting upward into the lumen of the ascending aorta. Between the semilunar cusps and the wall of the ascending aorta are pocket-like sinuses-the right, left, and posterior aortic sinuses. The right and left coronary arteries originate from the right and left aortic sinuses. Because of this, the posterior aortic sinus and cusp are sometimes referred to as the noncoronary sinus and cusp.
Mitral Valve - The left atrioventricular orifice opens into the posterior right side of the superior part of the left ventricle. It is closed during ventricular contraction by the mitral valve (left atrioventricular valve), which is also referred to as the bicuspid valve as it has two cusps; the anterior and posterior cusps. It prevents the back flow of blood as it is pumped from the left atrium to the left ventricle and are continuous with each other at the commissures.
Blood Supply[6][4][edit | edit source]
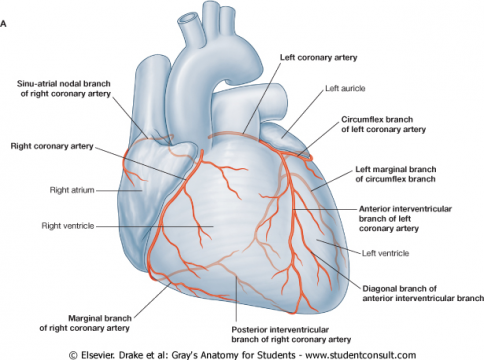
Arterial blood supply to the heart[edit | edit source]
The heart has 2 main arteries that supply it and the are namely
- right coronary artery (RCA)
- left coronary artery (LCA)
The RCA supplies
- The right atrium via the atrial branch
- Most of right ventricle.
- Part of the left ventricle (the diaphragmatic surface) via the posterior interventricular branch
- Part (usually the posterior third) of the IV septum via the right marginal branch
- The SA node (in approximately 60% of people) via the sino-nodal branch
- The AV node (in approximately 80% of people) via the atrioventricular branch
The LCA supplies
- The left atrium via the anterior interventricular branch (left anterior descending artery-LAD)
- Most of the left ventricle via the diagonal, circumflex and left marginal artery branches
- Part of the right ventricle.
- Most of the IVS (usually its anterior two thirds), including the AV bundle of the conducting system of the heart, through its perforating IV septal branches.
- The SA node (in approximately 40% of people).
Venous Drainage of the heart
The heart is drained mainly by veins that empty into the coronary sinus and partly by small veins that empty into the right atrium.
- The coronary sinus is a wide venous channel that runs from left to right in the posterior part of the coronary groove. It receives the great cardiac vein at its left end and the middle cardiac vein and small cardiac veins at its right end.The left posterior ventricular vein which drains the posterior surface of the left ventricule and left marginal vein also open into the coronary sinus.
- The great cardiac vein is the main tributary of the coronary sinus and it drains the areas of the heart supplied by the LCA. The middle cardiac vein (posterior IV vein) accompanies the posterior interventricular branch (usually arising from the RCA) and a small cardiac vein accompanies the right marginal branch of the RCA. Thus these two veins drain most of the areas commonly supplied by the RCA.
- The anterior cardiac veins begin over the anterior surface of the right ventricle, cross over the coronary groove, and usually end directly in the right atrium; sometimes they enter the small cardiac vein
Lymphatic drainage of the Heart[edit | edit source]
The lymphatic vessels of the heart follow the coronary arteries and drain mainly into:
- brachiocephalic nodes, anterior to the brachiocephalic veins
- tracheobronchial nodes, at the inferior end of the trachea.
Nerve Supply[edit | edit source]
The nerve supply to the heart is from two sets of nerves originating in the medulla of the brain. The nerves are part of the involuntary (autonomic) nervous system. One set, the branches from the vagus nerve, keeps the heart beating at a slow, regular rate. The other set, the cardiac accelerator nerves, speeds up the heart. The heart muscle has a special ability; it contracts automatically, but the nerve supply is needed to provide an effective contraction for blood circulation.
Branches from both the parasympathetic and sympathetic systems contribute to the formation of the cardiac plexus[4]. Branches from the cardiac plexus affect nodal tissue and other components of the conduction system, coronary blood vessels, and atrial and ventricular musculature.
Parasympathetic preganglionic fibers reach the heart as cardiac branches from the right and left vagus nerves. Stimulation of the parasympathetic system decreases heart rate, reduces force of contraction and constricts the coronary arteries.
Sympathetic fibers (from the upper four or five segments of the thoracic spinal cord ) reach the heart through the cardiac nerves from the sympathetic trunk. Stimulation of the sympathetic system increases heart rate and increases the force of contraction. From the cardiac plexus small branches, which are mixed nerves containing both sympathetic and parasympathetic fibers, supply the heart.
Visceral afferents fibers from the heart, a component of the cardiac plexus pass through the cardiac plexus and return to the central nervous system in the cardiac nerves from the sympathetic trunk and in the vagal cardiac branches.
The afferents associated with the vagal cardiac nerves return to the vagus nerve [X] and mainly concerned with cardiac reflexes.
The afferents associated with the cardiac nerves from the sympathetic trunks return to either the cervical or the thoracic portions of the sympathetic trunk and conduct pain sensation from the heart, which is detected at the cellular level as tissue-damaging events (i.e. cardiac ischemia).
Within the heart muscle itself, there are special groups of nerve fibers that conduct impulses for contraction. These groups make up the conduction system of the heart[1][4][6]. When the conduction system does not operate properly, the heart muscle contractions are uncoordinated and ineffective. The impulses within the heart muscle are tiny electric currents, which can be picked up and recorded by the electrocardiogram.
Embroyology[edit | edit source]
Developmental Timeline of Human Heart Embryology[10][9][edit | edit source] | |
| Days of human Developmental | Development process |
| 0 | Fertilization. |
| 1–4 | Cleavage and movement down the oviduct to the uterus. |
| 5–12 | Implantation of the embryo into the uterus. |
| 13–14 | Primitive streak formation (midstreak level contains precardiac cells). |
| 15–17 | Formation of the three primary germ layers (gastrulation): ectoderm, mesoderm, and endoderm. Midlevel primitive streak cells that migrate to an anterior and lateral position form the bilateral primary heart field. |
| 17–18 | Lateral plate mesoderm splits into the somatopleuric mesoderm and splanchnopleuric mesoderm. Splanchnopleuric mesoderm contains the myocardial and endocardial cardiogenic precursors in the region of the primary heart field. |
| 18–26 | Neurulation (formation of the neural tube) |
| 20 | Cephalocaudal and lateral folding brings the bilateral endocardial tubes into the ventral midline of the embryo. |
| 21–22 | Heart tube fusion. |
| 22 | Heart tube begins to beat. |
| 22–28 (3–4 wk) | Heart looping and the accretion of cells from the primary and secondary heart fields. |
| 22–28 (3–4 wk) | Proepicardial cells invest the outer layer of the heart tube and eventually form the epicardium and coronary vasculature. |
| 22–28 (3–4 wk). | Neural crest migration starts |
| 32–37 (5–6 wk) | Cardiac neural crest migrates through the aortic arches and enters the outflow tract of the heart. |
| 57+ (9 wk) | Outflow tract and ventricular septation complete. |
| Birth | Functional septation of the atrial chambers as well as the pulmonary and systemic circulatory systems. |
Histology of the Heart[11][edit | edit source]
Resources[edit | edit source]
- https://www.ncbi.nlm.nih.gov/pubmed/3642647
- https://www.ncbi.nlm.nih.gov/pubmed/21477775
- https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0025455/
- https://www.physio-pedia.com/Cranial_Nerves
- https://www.ncbi.nlm.nih.gov/pubmed/21357845
- https://www.ncbi.nlm.nih.gov/books/NBK354/
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Kenny, WL,Wilmore, JH, Costill, DL. Cardiovascular System and its Control. In Physiology of Sport and Exercise, 5rdedn. Human Kinetics, 2011. 140-150.
- ↑ 2.0 2.1 2.2 Malouf, JF, Edwards, WD, Tajil, AJ, Seward, JB. Functional anatomy of the heart. In: Fuster, F, Alexander, RW, O’Rourke, RA editors. Hurst’s: The Heart. 10th edn. McGraw-Hill Inc., 2001. p19–62.
- ↑ Ganong, WF. Lange Review of Medical Physiology, 22nd ed. McGraw-Hill. 2005
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Drake, RL, Vogl, W, Mitchell, AW, Gray, H. Gray's anatomy for Students 2nd ed. Philadelphia : Churchill Livingstone/Elsevier, 2010.
- ↑ Balaban, NE, Bobick, J, Cardiovascular system.The Handy Anatomy Answer Book. Detroit:Visible Ink Press, 2008. P197.
- ↑ 6.0 6.1 6.2 6.3 Moore, KL, Dalley, AF. Clinically oriented anatomy. 6th ed. Philadelphia: Lippincott Williams & Wilkins. 2009
- ↑ 7.0 7.1 7.2 Boulpaep, EL, Boron WF. Organisation of Cardiovascular System. Elsevier Saunders, 2005. p423–507
- ↑ Shah, S, Gnanasegaran, G, Sundberg-Cohon, J, Buscombe, JR. The Heart: Anatomy, Physiology and Exercise Physiology. 2009. DOI: 10.1007/978-3-540-78674-0_1
- ↑ 9.0 9.1 Weinhaus, AJ, Roberts, KP. Anatomy of the Human Heart. In: Iaizzo, PA. Hand book of Cardiac Anatomy, physiology and Devices. Humana press Inc.Totowa, New Jersey, 2005, P51-79
- ↑ Sherman, LS, Potter, SS, Scott, WJ, editors. Human Embryology, 3rd Ed. Churchill Livingstone, New York, NY.2001
- ↑ https://www.kenhub.com/en/library/anatomy/histology-of-the-heart