Alzheimer's Disease: Difference between revisions
Josie Little (talk | contribs) No edit summary |
Josie Little (talk | contribs) No edit summary |
||
| Line 28: | Line 28: | ||
== Prevalence == | == Prevalence == | ||
As of 2017, approximately 5.5 million people have Alzheimer's Disease in the United States and about 8 million are affected around the world.<ref>Latest Alzheimer's Facts and Figures [Internet]. Latest Facts; Figures Report | Alzheimer's Association. 2016 [cited 2017Apr1]. Available from: http://www.alz.org/facts/</ref> It is expected that by 2050 that number will have increased almost three fold to around 115.4 million. The known prevalence is 6% in people over the age of 65, 20% in people over the age of 80, and more than 95% in those 95 years of age. Alzheimer's disease is the sixth leading cause of death in adults. The period from onset to death is usually 7 to 11 years <ref>" / | As of 2017, approximately 5.5 million people have Alzheimer's Disease in the United States and about 8 million are affected around the world.<ref name="Facts">Latest Alzheimer's Facts and Figures [Internet]. Latest Facts; Figures Report | Alzheimer's Association. 2016 [cited 2017Apr1]. Available from: http://www.alz.org/facts/</ref> It is expected that by 2050 that number will have increased almost three fold to around 115.4 million. The known prevalence is 6% in people over the age of 65, 20% in people over the age of 80, and more than 95% in those 95 years of age. Alzheimer's disease is the sixth leading cause of death in adults. The period from onset to death is usually 7 to 11 years. <ref name="<ref name="Goodman">" />While death from other top 10 diseases have been observed to decline, from 2000-2014 Alzheimer’s disease as the primary cause of death has increased by 89%. <ref name="<ref name="Facts">" /><br>Early onset AD manifests between the ages of 30 and 60 years. This occurs in 1-6%of all cases.<br>Late onset AD manifests after the age of 60 years. This occurs in around 90% of cases.<br>● ⅔ of Americans with Alzheimer’s are women<br>● Older African Americans and Hispanics have an increased likelihood of developing Alzheimer’s or dementia than older white adults<ref name="<ref name="Facts">" /><br> | ||
<br> | <br> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Revision as of 21:09, 2 April 2017
Original Editors - Stephanie Schwebler from Pathophysiology of Complex Patient Problems Bellarmine University's Pathophysiology of Complex Patient Problems project and Irene Leahy
Top Contributors - <img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="24" _fck_mw_template="true">
Definition/Description
[edit | edit source]
Dementia is a general term for memory loss and other cognitive abilities that are required for activities of daily living [1]. Alzheimer's Disease (AD) is the most common cause of dementia worldwide. [2]The primary known risk factor for the disease is aging, but AD is not a normal part of aging. Alzheimer’s Disease is progressive so symptoms will worsen with time. There is currently no cure for the disease, but treatments are available to slow down the progression.[3] The understanding of the pathophysiology of this condition is constantly changing . There is a complex intertwining of mechanisms that manifest as AD.
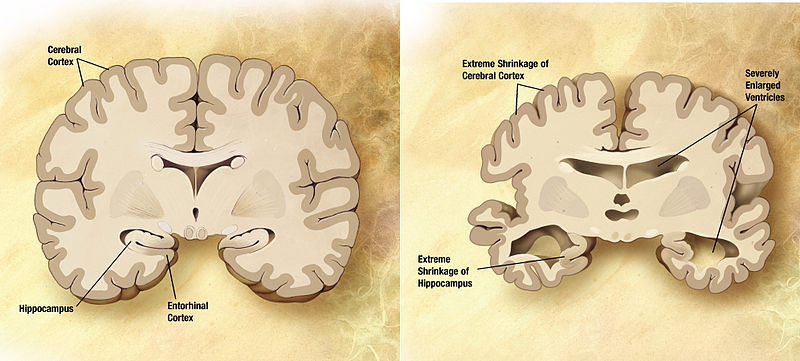
Alzheimer's Disease is characterized by cortical atrophy and loss of neurons, particularly in the parietal and temporal lobes. Also with loss of brain mass there is an enlargement of the ventricals of the brain.
[4] The changes in the brain tissue slowly cause changes in the person. These changes result in dementia, one form can be Alzheimer’s Disease.
Senile plaques which consist of extracellular amyloid are found in high concentrations in patients with Alzheimer's when compared with normal aging brains. [5] Neurofibrillary tangles in the neo cortex, amygdala, hippocampus and basal nucleus of Meynert can also occur. [6] In a normal functioning brain, B-amaloid dissolves and the brain reabsorbs it. When it is not reabsorbed, the B-amaloid protein can fold in on itself. The proteins then connect with one another and form a plaque. These plaques cause an inflammatory response that results in the damage of more neural tissue. Cite error: Closing </ref> missing for <ref> tag
| [7] | [8] |
Prevalence[edit | edit source]
As of 2017, approximately 5.5 million people have Alzheimer's Disease in the United States and about 8 million are affected around the world.[9] It is expected that by 2050 that number will have increased almost three fold to around 115.4 million. The known prevalence is 6% in people over the age of 65, 20% in people over the age of 80, and more than 95% in those 95 years of age. Alzheimer's disease is the sixth leading cause of death in adults. The period from onset to death is usually 7 to 11 years. Cite error: Closing </ref> missing for <ref> tag There are some key risk factors that need to be considered with Alzheimer's Disease.
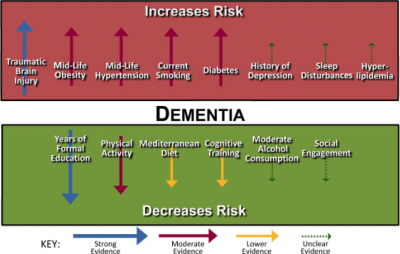
The Primary Risk Factors:
- Advancing age, > 85 y/o risk increases by nearly 50% [10]
- Direct family member with the disease (mother, father, brother or sister) Risk genes that increase the likelihood of developing the disease
- Apolipoprotein E-e4 (APOE4) carries the strongest risk of developing Alzheimer’s Disease, this is a genetic mutation of APOE [11]
- Risk believed to increase if carriers of the gene also have a traumatic brain injury
- See http://www.alz.org/research/video/video_pages/genetics_in_alz.html - for a video on how genetics effect alzheimers
- Deterministic genes have a direct cause of early onset AD, however they only account for less than 5% of cases: amyloid precursor protein (APP), presenilin-1 (PS-1), presenilin (PS-2) [12]
- Trisomy 21
- Cardiovascular risk factors: mid-life obesity, mid-life hypertension, hyperlipidemia, diabetes mellitus[13]
Possible Risk Factors:
- Head trauma - older adults with moderate traumatic brain injury (TBI) risk increases by 2.3x, severe TBI increases risk of AD by 4.3x. Believes to increase risk by increasing beta-amyloid and tau proteins. e.g. falls, MVA, sports injuries [14]
- History of Depression
- Progression of Parkinson-like signs in older adults
- Hyperhomocysteinemia
- Folate deficiency
- Hyperinsulinemia[15]
- Lower educational attainment
- Sleep Disturbances
- High Blood Pressure in midlife
- Hyper/Hypothyroidism [16]
Cite error: Closing </ref> missing for <ref> tag http://www.alz.org/living_with_alzheimers_behaviors.asp?cons_id=4488668
Stages of Alzheimer's Disease[edit | edit source]
Mild Alzheimer’s Disease (early stage)[17]
- May Function Independently: may drive, work or may be apart of social activities
- Memory Lapses: familiar words, location of objects, names of new people, recently read material
- Difficulties noticed by family, friends and doctors: challenges performing activities at home or work, difficulty planning
- Lack of spontaneity
- Subtle personality changes
- Disorientation to time and date
Moderate Alzheimer’s Disease (middle-stage)
- Longest stage, may last for years
- Personality changes: moody or withdrawn, suspiciousness, delusions, compulsive, repetitive behavior
- Increased memory loss: forgetfulness regarding personal history, unable to recall address, phone number, or high school they graduated from
- Decreased independence: trouble controlling bowel and bladder, increased risk of wandering or becoming lost, dependence with choosing appropriate clothes for event or season, increased Confusion
- Impaired cognition and abstract thinking
- Restlessness and agitation
- Wandering, "sundown syndrome"
- Inability to carry out activities of daily living
- Impaired judgment
- Inappropriate social behavior
- Lack of insight, abstract thinking
- Repetitive behavior
- Voracious appetite
Severe Alzheimer’s Disease (late stage)
- Decreased response to the environment: decreased ability to communicate and may speak in small phrases, decreased awareness of experiences & surroundings
- Dependence on caregiver: decreased physical functioning: walking, sitting & swallowing; increased vulnerability to infections, incontinence
- Emaciation, indifference to food
- Inability to communicate
- Urinary and fecal incontinence
- Seizures
| [18] | [19] |
Associated Co-morbidities[edit | edit source]
A high level of comorbidity is associated with poor self care, decreased mobility and incontinence. Increased co-morbidity is associated with lower cognitive score observed through a mini-mental status examination.
Vascular Disease
Thyroid Disease
Sleep Apnoea
Osteoporosis
GlaucomaCancer
Rheumatoid Arthritis & NSAIDs
DepressionCite error: Closing </ref> missing for <ref> tag
Causes[edit | edit source]
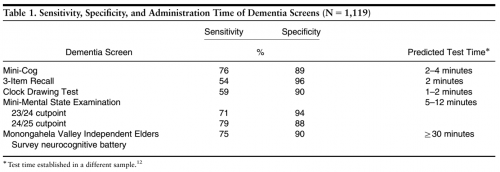
Objective tools have been validated in the practice of physical therapy in order to screen for AD such as the Mini-Cog, Mini-Mental State Exam (MMSE), Clock-Drawing, & Neurobehavioral Cognitive Status Exam. Screening tools can be chosen based upon sensitivity, specificity and time to administer the screen.
Mini-Mental State Exam was validated for detecting possible dementia, however time to administer the exam keeps physicians from using it. The MMSE takes 5-12 minutes to administer and is composed of 20 questions in 5 categories to observe orientation, memory, attention-concentration, language and constructing[20].
- Cut off scores: (out of 25)
- ≥ 24 = no impairment
- 18-23 = mild impairment
- ≤ 17 = severe impairment
- ≥ 27 = no impairment
- 21–26 = mild impairment
- 11–20 = moderate impairment
- ≤ 10 = severe impairment
- < 23 is generally accepted as indicating cognitive impairment and was associated with the diagnosis of dementia in at least 79% of cases (Lancu & Olmer, 2006) [21]
Mini-Cog takes 2-4 minutes to administer and combines constructing (clock drawing) and memory. [22]
Below are current findings for ruling the differential diagnosis of AD in or out, due to how the tests perform in terms of sensitivity, it would be best to cluster these tests in order to rule in the possibility of dementia or AD.
Systemic Involvement[edit | edit source]
The most noticeable symptoms initially are the cognitive and memory related symptoms. However Alzheimer's disease can affect other parts of the body causing symptoms other than those affecting the memory and cognition. Often abnormal motor signs can be apparent depending on the area of the brain affected by the disease.The presence of tremors can be associated with increased risk for cognitive decline, presence of bradykinesia with increased risk for functional decline, and presence of postural-gait impairments with increased risk of institutionalization and death. Additionally, patients may develop disorders of sleeping, eating, and sexual behavior.[24]
Medical Management (current best evidence)[edit | edit source]
There is currently no cure for Alzheimer's Disease, so medical management is focused on maintaining quality of life, maximizing function, enhancing cognition, fostering a safe environment and promoting self engagement. Maximizing dementia functioning involves monitoring the patient's health and cognition, patient and family education, initiation of pharmacological and non pharmacological treatments.
● Cognitive symptom treatment
○ Although the disease progression cannot be altered, it may be slowed by the pharmacological medication listed above.
● Behavioral and psychological symptom treatment
○ Agitation, aggression, depression and psychosis are the primary cause of assisted living or nursing home placement.
○ Assessment of behaviors occurring suddenly is important to increase patient comfort, security and ease of mind.
● Monitoring Alzheimer’s disease
○ Patients should return on a regular basis in order for the physician to monitor the course of Alzheimer’s disease (behavioral and cognitive changes).
○ Regular follow-up appointments allow for adaptation of treatment styles to fit the needs of the patient.
○ Nonmedical/Social Issues the patients need to address:
■ Need for ongoing support & information
■ A living will or power of attorney
■ Review of finances/planning for future and end of life care
● Alternative Treatment
○ There are concerns regarding alternative treatments in addition to physician-prescribed medicine. If any concerns are questions are brought to attention, the physician should be notified.
● Importance of Caregiver
○ Many caregivers seek to meet the needs of the physician and the patient which increases rates of stress and depression. Physicians should continue to monitor the status of the caregivers watching out for burnout and providing them with resources as well. [25]
Physical Therapy Management (current best evidence)[edit | edit source]
| [26] |
It is important to modify risk factors that can be changed through lifestyle activities. Hypertension has been shown to interact with a particular genotype that is at risk for developing Alzheimer’s disease. This interaction increases amyloid deposition in cognitively healthy middle aged and older adults. Thus, when at risk it is important to manage blood pressure, which can be done through exercise. [27]
Physical activity is important to incorporate in a patient’s with Alzheimer’s disease life, and the sooner the better. “Earlier application of physical activity to mitigate pathological processes and to assuage cognitive decline is imperative given recent evidence from clinical trials suggesting that interventions applied earlier in the course of Alzheimer's Disease are more likely to achieve disease modification, whereas those applied later have a significant but more limited effect after the emergence of neuronal degeneration.” [28]
A community based exercise program has been shown improve multiple domains of life for individuals with Alzheimer's. In a study by Vreugdenhil et al., community dwelling individuals with Alzheimer's added a daily home exercise program and walking under supervision to a usual treatment plan. Those participating in the additional exercise improved in cognition, mobility, and instrumental activities of daily living. [29] It has been suggested that aerobic exercise in the form of walking and upper limb cycle ergometer in particular helps to improve exercise tolerance as well as quality of life in individuals with Alzheimer's. [30] Strength training in addition to aerobic training has been supported in the research. The combination of both activities have shown greater improvements in cognition than aerobic training alone. [31]
Individuals with dementia are at an increased risk for falling compared to the average population of community dwelling older adults. [32] Preliminary research has been conducted looking at falls prevention training for individuals with intellectual disorders such as Alzheimer’s disease. A study found that using a modified Otago Exercise program was effective at decreasing falls risk for some adults with intellectual disabilities. [33] A pilot study found that the Berg Balance Scale had relative reliability values that support its use in clinical settings. However, MDC values are not established for this population. [34] More research is needed in this area to best assess falls risk in this population.
Frequently,when a physical therapist works with a patient who has been diagnosed with an Alzheimer's, the patient may be in a structured living environment because they have progressed to a stage in the disease where their caregivers can not give the patient the proper attention that they need. Physical therapy can provide the patient with an activity that the patient can perform successfully at and it also can help to improve their breathing, mobility, and endurance. Restlessness and wandering can be typical of the patients with Alzheimer's patient and may be managed with physical therapy (by releasing some of the energy through exercises). These exercises can help to reduce the night time wanderings called sundowning. Group therapy is also successful with patients with Alzheimer's disease, but the session must not provide more stimulation than the patient is able to tolerate. Repetition and encouragement are also very important to help keep the patient's confidence high and to help with remembering the exercises. Knowing the patient is important to the therapist because it can allow for better communication, by using words and terms that the specific patient may be more familiar with. The Preferred Practice Pattern is 5E: Impaired Motor Function and Sensory Integrity Associated with Progressive Disorders of the Central Nervous System. The physical therapist can use the Global Deterioration Scale to assess the level of dementia. When a patient with Alzheimer's is placed in a comprehensive cognitive stimulation program it enhances the neuroplasticity of the patient. The exercise can also help to improve mobility, balance, and ROM for the patient as well as improve the mood.[35]
Staying physically and socially active can possibly help to decrease the risk for dementia along with staying mentally active. This web site has some suggestions on how to keep active socially, mentally, and physically as well as some tips on a brain healthy diet.
Dietary Management (current best evidence)[edit | edit source]
It has been found that maintaining a healthy diet may help to prevent or slow the progression of Alzheimer's. It is suggested that the diet be low in fat, high in omega-3 oils, and high in dark vegetables and fruits, also adding vitamin C to the diet along with coenzyme Q10, and folate may work to lower the risk of Alzheimer's. There does not seem to be one single aspect of diet that provides neuroprotection, rather that the items work together to decrease risk of AD.[36]There is also some interest in the use of antioxidants such as vitamin E and ginkgo, along with anti-inflammatory agents, and estrogen replacement therapy for women.[37]
Differential Diagnosis[edit | edit source]
- Pick's Disease
- Lewy Body Dementia
- Frontotemporal Dementia
- Dementia from multiple medications
- other potentially reversible causes of dementia
Case Reports
[edit | edit source]
Electronic tracking system and wandering in Alzheimer's disease: a case study.
Frontiers proposal. National Institute on Aging "Bench to bedside: estrogen as a case study".
Resources
[edit | edit source]
- http://www.alz.org/index.asp
- http://www.nia.nih.gov/Alzheimers/Publications/adfact.htm
- http://www.physio-pedia.com/Carers_guide_to_dementia
- http://www.physio-pedia.com/Promoting_Independence_for_Persons_with_Dementia;_A_Guide_for_Carers
Recent Related Research[edit | edit source]
References[edit | edit source]
- ↑ Alzheimer's Disease and Dementia [Internet]. Alzheimer's Association. [cited 2017Apr1]. Available from: http://www.alz.org/alzheimers_disease_what_is_alzheimers.asp
- ↑ Anand, R., Gill, K.D. and Mahdi, A.A. (2014) 'Therapeutics of Alzheimers disease: past, present and future', Neuropharmacology, 76, 27-50
- ↑ Goodman CC, Fuller KS. Pathology: implications for the physical therapist. St. Louis, MO: Elsevier Saunders; 2015.
- ↑ Porth C. Pathopysiology Concepts of Altered Health States. Philadelphia PA: Lippincott and Wilkins; 2005.
- ↑ actionalz. What is Alzheimer's Disease?. Available from: http://www.youtube.com/watch?v=9Wv9jrk-gXc [last accessed 08/12/12
- ↑ wenk, G.L. (2003) 'Neuropathological changes in Alzheimers disease', Journal of clinical psychiatry, 64, 7-10
- ↑ actionalz. What is Alzheimer's Disease?. Available from: http://www.youtube.com/watch?v=9Wv9jrk-gXc [last accessed 08/12/12]
- ↑ Erdinç Nayır. Alzheimer's Disease - 3D Health Animations. Available from: http://www.youtube.com/watch?v=y3g4emLQ1Ic [last accessed 08/12/12]
- ↑ Latest Alzheimer's Facts and Figures [Internet]. Latest Facts; Figures Report | Alzheimer's Association. 2016 [cited 2017Apr1]. Available from: http://www.alz.org/facts/
- ↑ Alzheimer's &amp;amp;amp;amp;amp;amp;amp; Dementia Causes, Risk Factors | Research Center [Internet]. Alzheimer's Association. [cited 2017Apr1]. Available from: http://www.alz.org/research/science/alzheimers_disease_causes.asp
- ↑ Alzheimer's and Dementia Causes, Risk Factors | Research Center [Internet]. Alzheimer's Association. [cited 2017Apr1]. Available from: http://www.alz.org/research/science/alzheimers_disease_causes.asp#apoe
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="APOE"&amp;amp;amp;amp;amp;amp;gt;
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="Facts"&amp;amp;amp;amp;amp;amp;gt;
- ↑ Traumatic Brain Injury | Signs, Symptoms, &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Diagnosis [Internet]. Dementia. [cited 2017Apr1]. Available from: http://www.alz.org/dementia/traumatic-brain-injury-head-trauma-symptoms.asp
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="Facts"&amp;amp;amp;amp;amp;amp;gt;
- ↑ Duthie A, Chew D, Soiza RL. Non-psychiatric comorbidity associated with Alzheimer's disease. Qjm [Internet]. 2011 [cited 2017Apr1];104(11):913–20. Available from: https://academic.oup.com/qjmed/article/104/11/913/1563428/Non-psychiatric-comorbidity-associated-with
- ↑ Stages of Alzheimer's Symptoms [Internet]. Alzheimer's Association. [cited 2017Apr1]. Available from: http://www.alz.org/alzheimers_disease_stages_of_alzheimers.asp
- ↑ Post Gazette Now. Battling Early Onset Alzheimer's Disease. Available from: http://www.youtube.com/watch?v=Kd9p2YGlTO8 [last accessed 08/12/12]
- ↑ Alzheimer's Society. Later Stage Dementia: Bruce and Jan's Story. Available from: http://www.youtube.com/watch?v=chgshB6LCyc [last accessed 08/12/12]
- ↑ Benson AD, Slavin MJ, Tran T-T, Petrella JR. Screening for Early Alzheimer's Disease: Is There Still a Role for the Mini-Mental State Examination? The Primary Care Companion [Internet]. [cited 2017Apr1]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1079697/
- ↑ Rehab Measures - Mini-Mental State Examination [Internet]. The Rehabilitation Measures Database. [cited 2017Apr1]. Available from: http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=912
- ↑ Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a Screen for Dementia: Validation in a Population-Based Sample. Journal of the American Geriatrics Society. 2003;51(10):1451–4.
- ↑ &amp;amp;amp;amp;amp;lt;ref name="Borson"&amp;amp;amp;amp;amp;gt;
- ↑ &amp;amp;amp;amp;amp;lt;ref name="Goodman"&amp;amp;amp;amp;amp;gt;
- ↑ Medical Management and Patient Care [Internet]. Alzheimer's Association. [cited 2017Apr1]. Available from: http://www.alz.org/health-care-professionals/medical-management-patient-care.asp
- ↑ Pollom E, Little J. PT Management of Alzheimer's Disease [Internet]. YouTube. YouTube; 2017 [cited 2017Apr2]. Available from: https://www.youtube.com/watch?v=rW3rQ73rQFE&amp;amp;amp;amp;amp;amp;amp;t=8s
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="Goodman"&amp;amp;amp;amp;amp;amp;gt;
- ↑ Phillips, C. et al. "The Link Between Physical Activity And Cognitive Dysfunction In Alzheimer Disease". Physical Therapy 95.7 (2015): 1046-1060. Web. 1 Apr. 2017.
- ↑ Vreugdenhil, Anthea et al. "A Community-Based Exercise Programme To Improve Functional Ability In People With Alzheimer’S Disease: A Randomized Controlled Trial". Scandinavian Journal of Caring Sciences 26.1 (2011): 12-19. Web. 1 Apr. 2017.
- ↑ Mahmoud S. “Role of aerobic exercise training in changing exercise tolerance and quality of life in Alzheimer's disease”. European journal of general medicine. 2011;8(1):1-6. Web. 1 Apr. 2017.
- ↑ Manckoundia, Patrick et al. "Impact Of Ambulatory Physiotherapy On Motor Abilities Of Elderly Subjects With Alzheimer's Disease". Geriatrics&amp;amp;amp;amp;amp;nbsp;; Gerontology International 14.1 (2013): 167-175. Web. 1 Apr. 2017.
- ↑ Renfro M, Bainbridge D, Smith M. Validation of Evidence-Based Fall Prevention Programs for Adults with Intellectual and/or Developmental Disorders: A Modified Otago Exercise Program. Frontiers in Public Health. 2016;4. Web. 1 Apr. 2017.
- ↑ Muir-Hunter S, Graham L, Montero Odasso M. Reliability of the Berg Balance Scale as a Clinical Measure of Balance in Community-Dwelling Older Adults with Mild to Moderate Alzheimer Disease: A Pilot Study. Physiotherapy Canada. 2015;67(3):255-262. Web. 1 Apr. 2017.
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="Renfro"&amp;amp;amp;amp;amp;amp;gt;
- ↑ &amp;amp;amp;amp;amp;amp;lt;ref name="Goodman"&amp;amp;amp;amp;amp;amp;gt;
- ↑ &amp;amp;amp;amp;amp;lt;ref name="Goodman"&amp;amp;amp;amp;amp;gt;
- ↑ Porth C. Pathopysiology Concepts of Altered Health States. Philadelphia PA: Lippincott and Wilkins; 2005.