Achilles Tendinopathy
Search Strategy[edit | edit source]
We began with the template of the VUB. We searched articles based on the 16 contents. Some contents already had information about our disease on the current Physiopedia page and other contents didn’t. We added the information from the articles to the existing text. Databases searched: VUBis, Pubmed, Physiopedia, JOSPT, Google Scholar, British Journal of Sport Medicine, Web of Science, Fai sagepub Keywords searched:
achilles tendonitis
achilles tendinopathy
achilles tendinitis
clinical characteristics and achilles tendonitis
achilles tendonitis treatment
achilles tendonitis physical therapy
physiotherapy and achilles tendonitis
differential diagnose and achilles tendinopathy
achilles tendinopathy and diagnostic procedures
...
Definition and mechanism of injury[edit | edit source]
Achilles tendinitis is a common overuse injury caused by an excessive stretching or tearing of the Achilles tendon in an acute context. This can lead to a sudden injury, or in the worst case, can cause a rupture of the Achilles tendon. In both cases, a lack of flexibility or a stiff Achilles tendon can increase the risk of these injuries. [1]
A lot of descriptions are given concerning Achilles Tendinopathy. Usually a difference is made between the insertional and the mid portion form. The difference is in the localisation. The insertional form is situated at the level of transition between the Achilles tendon and the bone. The midportion form is located at the level of the tendon body. It is described as the gradually emerged of pain 2-6 cm above the calcaneal insertion of the Achilles tendon, associated with degenerative changes and often with thickening of the tendon. [2] Surgical specimens show a range of degenerative changes of the affected tendon, such as in the tendon fibre structure and arrangement as well as an increase in glycosaminoglycans, which may explain the swelling of the tendon. [3] The precise cause of tendonitis remains unclear. Even though tendonitis of the achilles tendon is often connected to sport activities, the ailment is also often found with people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the achilles tendon can be latently present, but pain only appears when the tendon is overburdened. It is also noted that the ailment is usually not preceded by a trauma. [4], [5]
The terms “tendinose”, “tendonitis” or “tendinitis” and “tendinopathy” are commonly used. The definitions of those terms are often described in a different manner. Because of that, it's difficult to evaluate articles and to compare them (Alfredson, 2003). [6] Tendinitis is the inflammation of the tendon and is caused by micro-tears that happen when the musculotendinous unit is acutely overloaded with a tensile force that is too heavy and/or too sudden. [7] Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury [8] or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. [9] In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendonitis is more appropriate. Tendonitis is a degeneration of the tendon’s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury. Even tiny movements, such as clicking on a mouse, can cause tendinosis, when done repeatedly.
Achilles tendonitis is a degenerative change of the Achilles Tendon associated with pain and often with the thickening of the tendon. It is common in athletes, but it also occurs in non athletes. Surgical specimens show a range of degenerative changes of the affected tendon, such as changes in tendon fibre structure and arrangement as well as an increase in glycosaminoglycans, which may explain the swelling of the tendon. [10] The precise cause of tendonitis remains unclear. Even though tendonitis of the achilles tendon is often connected to sport activities, the ailment is also often found with people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the achilles tendon can be latently present, but pain only comes into being when the tendon is overburdened. It is also noted that the ailment is usually not preceded by a trauma. [11], [12] Tendonitis is often confused with tendonitis, but it is important to understand the difference between these two pathologies. Tendonitis is an inflammation of the tendon. This inflammation causes micro-tears in the tendon when it is acutely overloaded. This diagnosis is often mistakenly used when the patient actually has tendonitis. Tendonitis is a degeneration process in which no temperature rises occur, as opposed to tendonitis. It is very important to distinguish between these disorders, to discover which treatment is required, and what the expected duration of the treatment will be. The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendonitis has become chronic. [13], [14]
Clinically Relevant Anatomy[edit | edit source]
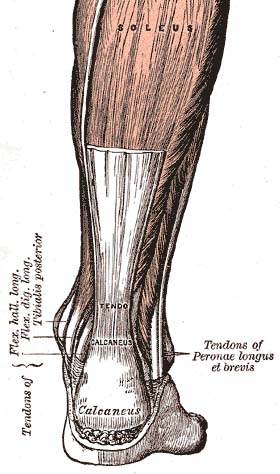
The achilles tendon is the biggest and strongest tendon in the h
uman body. The tendon has the capacity to resist large tensile forces. It stems from a distal confluence of the gastrocnemius and soleus muscle and inserts at the bottom of the calcaneus. Like other tendons, Achilles has a hierarchical structure. [15] The M. soleus is a prime mover plantar flexor of the ankle and the m. gastrocnemius is a flexor of the knee. A typical tendon structure consists of thin, cylindrical cells and an extracellular matrix. The cells of the tendon, respectively tenocytes tenoblasts, are responsible for the synthesis of all of the components of the extracellular matrix. Inside the matrix we find bundles of type I collagen and elastin. This type-I collagen is responsible for the strength of the tendon. Between the collagen there is a ground substance located which is made up of proteoglycans and glycosaminoglycans. [16] The achilles tendon is surrounded by parthenon and not by the common known synovial membrane. The parthenon works as an elastic sleeve around the tendon which allows the tendon to move freely between surrounding tissue. The parthenon consists out a layer of cells and is responsible for blood transportation of the tendon. The layers that are formed under the parthenon are in chronological order: the epitenon which is a thin membrane and the endotenon wichon his turn surrounds the collagen fibers which results in bundles. [17]
Epidemiology / Etiology[edit | edit source]
The etiology of Achilles tendonitis is still unclear. Straining the tendon during physical exercise has been seen as one of the biggest pathological stimulus. Systematic overloading of the Achilles tendon above his physiological limit can cause a micro-trauma.
Repetitive micro-traumas that are linked with a non-uniform tension between the M. gastrocnemius and M.soleus, cause frictional forces between the fibers and abnormal concentrations of the loading in the achilles tendon. This has consequences such as the inflammation of the tendon sheath, degeneration, or a combination of both. Without the minimum time for recovery, this can lead to a tendinopathy. [18]
In acute trauma, the external factors dominate , while injuries caused by overuse generally have a multifactorial origin. The acute phase of Achilles tendinopathy is caused by acute overload, blunt trauma or acute muscle fatigue, and is characterized by an inflammatory reaction and edema formation. If the treatment of the acute phase fails or if they overlooked it, it can cause a fibrin and form adhesions off the tendon.
Often, tendon degeneration is found in combination with peritendinous adhesions, but this does not mean that one condition causes the other one. Decreased arterial blood flow, local hypoxia, decreased metabolic activity, nutrition, and a persistent inflammatory response have been suggested as possible factors that could lead to chronic tendon overuse injuries and tendon degeneration.
In epidemiological studies, various alignments and biomechanical faults are claimed to play a causative role in two-thirds of the athletes with an Achilles tendon disorder.
The most common and perhaps the most important malalignment is the one of the ankle caused by hyperpronation of the foot. Increased foot pronation has been proposed to be associated with Achilles tendinopathy.
So we can say that the effects of overuse, poor circulation, lack of flexibility, gender, endocrine or metabolic factors can lead to tendinopathies. The structure of the tendon is disturbed by this repetitive strain (often eccentric nature) and collagen fibers go along together, break the crosslinks and the slide denaturation cause tissue, causing inflammation. This cumulative microtrauma is assumed not only weaken collagen cross-linking, but also the collagenous matrix and the vascular elements of influencing the tendon, which ultimately leads to tendonitis. [19]
Clinical representation[edit | edit source]
Morning pain is a hallmark symptom because the achilles tendon must tolerate full range of movement including stretch immediately after getting up in the morning. Symptoms are typically localized to the tendon and the immediate surrounding area. Swelling and pain are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes. [20] With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis. [21] The affected side of the tendon shows a larger diameter, higher stiffness and lower strain in comparison to the non affected side. Patients with an insertion Achilles tendinopathy (IAT) have lower echogenicity, correlated with a higher severity of symptoms. [22]
Symptoms and differential diagnose[edit | edit source]
Heel pain is a common symptom. There are many causes, but mechanical etiology is the most common. The location of the pain can be a guide to establish the correct diagnosis. The most common diagnosis is plantar fasciitis, a condition that leads to medial plantar heel pain. Other causes of pain can include a plantar heel calcaneal fracture stress. Heel pad syndrome (deep, bruises and pain in the center of the heel). Achilles tendinopathy is a common condition that causes posterior heel pain. This pain is localized to the site of insertion of the affected tendon. Posterior heel pain can also be attributed to anHaglund deformity. This is a prominence of the calcaneus that can cause bursitis between the calcaneus and the Achilles tendon (also called Sever's disease). To differentiate between the causes of pain in the heel can be achieved by a history and physical examination, with the right imaging studies (if indicated). [23] Posterior Ankle Impingement, Medial Tendinopathy, Retrocalcaneal Bursitis, Sural Nerve, Lumbar Radiculopathy, Ankle OA, DVT, Haglund Deformity, Partial Achilles Tendon Rupture. [24]
Diagnostic procedures[edit | edit source]
Outcome measures [edit | edit source]
Research [edit | edit source]
The four cornerstones of tendon histopathology are: 1: cellulaire activation and an increase in cell numbers, 2: an increase in ground substance, 3: collagen disarray and 4: neovascularization. An achilles tendinitis is primarily not seen as an inflammatory condition. However the signs of inflammation are real and irreversible. Research confirms that the inflammation is neurogenic.
The presence of neuropeptides such as ‘substance P’ and of calcitonin genes related to peptides indicate an inflammation in the tendon.
Medical Management[edit | edit source]
Corticosteroid injections[edit | edit source]
Sclerosering injections[edit | edit source]
Rehabilitation after a sclerosing injection consists in 1 - 3 days of rest; then tendon-loading activity increases gradually avoiding maximum loading. After 2 weeks tendon loading activity is allowed (jumping, fast runs, heaving strength training). This research suggests a clinical role for sclerosing therapy for those who fail to respond to eccentric exercise. [38] (level 3A)
Plateled-rich Plasma injections[edit | edit source]
Operative surgery[edit | edit source]
In 75% of subjects who underwent tenotomy experienced a positive result after 18 months. An open procedure of the achilles tendon resulted in better outcomes of tendons without a focal lesion. [40] (level 3A)
Physical management[edit | edit source]
Active rehabilitation[edit | edit source]
It was shown that strength training, that is stimulated externally and is linked to a motion expert task, not only helps reduce tendon pain but modulate excitatory and inhibitory control of muscle, and thus potentially tendon load. [41] (level 3A) A popular and effective option is the eccentric strength training. [42] (level 1A)
Eccentric exercises have been shown to have positive effects of Achilles tendonitis. [43], [44] In the past decade, an eccentric training (ECC) has become the main non-surgical choice of treatment for achilles tendinopathy [45] (level 2A) and remains as the gold standard for rehabilitation of this condition. [46], [47] But there is no convincing evidence that the most effective exercise regimen. In fact, a recent systematic review concluded that there is little clinical and mechanistic evidence that supports the use of the eccentric component and compare that well-conducted studies of different load programs are largely lacking. [48] (level 2A) New loading based exercise regimes such as insulated concentric exercise, heavy slow resistance training (HSR), and eccentric-concentric becoming ECC proposed but lack solid scientific evidence for their effectiveness in achilles tendinopathy. The results of a study suggest that HSR and ECC improve the symptoms and physical activity as well in patients with chronic mid-portion achilles tendinopathy. [49] (level 1A) A study by Roos et al concluded that eccentric exercises improve function and reduce pain and effects were apparent after 6 weeks of treatment, lasting for 1 year. [50] An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for midportion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises. [51] (level 1A), [52] (level 1A), [53] (level 1A) Thorough management guidelines for achilles tendinopathy is covered in detail in the Achilles Tendinopathy Toolkit. A treatment with a combination of 4 weeks of laser therapy prior to 6 weeks of eccentric exercise therapy gives significantly better results than eccentric exercise therapy without laser therapy. [54] (level 1A)
Passive rehabilitation[edit | edit source]
Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy. [56] (level 1A), [57] (level 1A)
Mobilisations[edit | edit source]
Previous studies have shown that Rocker shoes are able to internal plantar flexion related they have conducted research on the Achilles tendon to people who walked with the rocker and without shoes. People who walked with the rocker shoes cause a significant reduction in plantar flexion moment in the late stance phase of walking. [65] (level 2A)
Soft tissue treatment (Astym) plus eccentric exercise appears to be a beneficial treatment program that clinicians should consider incorporating into the management of their patients with insertional AT. [66] (level 2)
Recently, the use of Extracorporeal Shock Wave Therapy was proven. [67] (level 1A), [68] (level 2A), [69] (level 1B)
Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. [70] (level 1A), [71] (level 2A), [72] (level 1A)
Other treatments [edit | edit source]
Nitroglycerin patches have a firming impact on the achilles tendon when applied. [28] (level 3A)
Key Research[edit | edit source]
Resources[edit | edit source]
- SportMed
Clinical bottom line[edit | edit source]
[edit | edit source]
*Skalec, A., et al. "Ultrasonography and low-field magnetic resonance imaging of the common calcanean tendon in a rabbit model for tendinopathy research: a descriptive study of normal anatomy." Polish Journal of Veterinary Sciences19.3 (2016): 525-534.
*Yu, Hainan, et al. "The Effectiveness of Physical Agents for Lower-Limb Soft Tissue Injuries: A Systematic Review." Journal of Orthopaedic & Sports Physical Therapy 0 (2016): 1-101.
*McCormack, Joshua R., et al. "Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy A Randomized Controlled Trial." Sports Health: A Multidisciplinary Approach (2016): 1941738116631498.
*Fouré, Alexandre. "New Imaging Methods for Non-invasive Assessment of Mechanical, Structural, and Biochemical Properties of Human Achilles Tendon: A Mini Review." Frontiers in Physiology 7 (2016).
*Rio, Ebonie, et al. "Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review." British journal of sports medicine 50.4 (2016): 209-215. *McCormack, Joshua R., et al. "Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy A Randomized Controlled Trial." Sports Health: A Multidisciplinary Approach (2016): 1941738116631498.
Read 4 Credit[edit | edit source]
References[edit | edit source]
- ↑ Clain, Michael R., and Donald E. Baxter. "Achilles tendinitis." Foot & Ankle International 13.8 (1992): 482-487. Level 2A
- ↑ VAN DER, Arnt, and Liselot VAN DE WALLE. "HET EXCENTRISCH TRAINEN VAN DE KUITSPIEREN." Level 1B
- ↑ T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.fckLR Level 3B
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ Van Sterkenburg, M. N. (2006). Achilles tendinopathy: new insights in cause of pain, diagnosis and. Foot Ankle Clin, 11(2), 421-7. Level 1B
- ↑ Evelyn Bass. Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters Int J Ther Massage Bodywork. 2012; 5(1): 14–17.fckLRPublished online Mar 31, 2012. Level 2A
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.
- ↑ T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.fckLR Level 3B
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A
- ↑ Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2A
- ↑ Freedman, Benjamin R., Joshua A. Gordon, and Louis J. Soslowsky. "The Achilles tendon: fundamental properties and mechanisms governing healing." MLTJ Muscles, Ligaments and Tendons Journal 4.2 (2014): 245-255. Level 2A
- ↑ VAN DER, Arnt, and Liselot VAN DE WALLE. "HET EXCENTRISCH TRAINEN VAN DE KUITSPIEREN." Level 1B
- ↑ Kiewiet, Nathan J., et al. "Gastrocnemius recession for chronic noninsertional Achilles tendinopathy." Foot & ankle international (2013): 1071100713477620. Level 4
- ↑ Young, Jonathan S., and N. Maffuli. "Etiology and epidemiology of Achilles tendon problems." The Achilles Tendon (2007): 39-49. Level 2B
- ↑ Paavola, M., Kannus, P., Järvinen, T. A., Khan, K., Józsa, L., & Järvinen, M. (2002). Achilles tendinopathy. J Bone Joint Surg Am, 84(11), 2062-2076. Level 2B
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ Chimenti, Ruth L., et al. "Altered tendon characteristics and mechanical properties associated with insertional Achilles tendinopathy." Journal of Orthopaedic & Sports Physical Therapy 44.9 (2014): 680-689. Level 3B
- ↑ Tu, Priscilla, and Jeffrey R. Bytomski. "Diagnosis of heel pain." American family physician 84.8 (2011). Level 2A
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones Bartlett Learning.
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B
- ↑ Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.fckLR Level 5
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Fouré, Alexandre. "New Imaging Methods for Non-invasive Assessment of Mechanical, Structural, and Biochemical Properties of Human Achilles Tendon: A Mini Review." Frontiers in Physiology 7 (2016). Level 1B
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.
- ↑ D. Gould et al. Visual Analogue Scale (VAS). Journal of Clinical Nursing 2001; 10:697-706. Level 1A
- ↑ Alfredson, Håkan, and Jill Cook. "A treatment algorithm for managing Achilles tendinopathy: new treatment options." British journal of sports medicine 41.4 (2007): 211-216. Level 3A
- ↑ Alfredson, Håkan, and Jill Cook. "A treatment algorithm for managing Achilles tendinopathy: new treatment options." British journal of sports medicine 41.4 (2007): 211-216. Level 3A
- ↑ Alfredson, Håkan, and Jill Cook. "A treatment algorithm for managing Achilles tendinopathy: new treatment options." British journal of sports medicine 41.4 (2007): 211-216. Level 3A
- ↑ Ultrasound-Guided Injection Therapy of Achilles Tendinopathy With Platelet-Rich Plasma or Saline: A Randomized, Blinded, Placebo-Controlled Trial. Level 1A
- ↑ Alfredson, Håkan, and Jill Cook. "A treatment algorithm for managing Achilles tendinopathy: new treatment options." British journal of sports medicine 41.4 (2007): 211-216. Level 3A
- ↑ Rio, Ebonie, et al. "Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review." British journal of sports medicine 50.4 (2016): 209-215. Level 3A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.
- ↑ Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013;43(4):267-286. Level 2A
- ↑ Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.
- ↑ Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013;43(4):267-286. Level 2A
- ↑ Beyer, Rikke, et al. "Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy A Randomized Controlled Trial." The American journal of sports medicine (2015): 0363546515584760. Level 1A
- ↑ Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Photobiomodulation and eccentric exercise for Achilles tendinopathy: a randomized controlled trial. Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A
- ↑ ohn J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A
- ↑ ohn J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones Bartlett Learning.
- ↑ Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B
- ↑ James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.
- ↑ Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A
- ↑ ohn J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Sobhani, Sobhan, et al. "Rocker shoes reduce Achilles tendon load in running and walking in patients with chronic Achilles tendinopathy." Journal of Science and Medicine in Sport 18.2 (2015): 133-138. Level 2A
- ↑ McCormack, Joshua R., et al. "Eccentric Exercise Versus Eccentric Exercise and Soft Tissue Treatment (Astym) in the Management of Insertional Achilles Tendinopathy A Randomized Controlled Trial." Sports Health: A Multidisciplinary Approach (2016): 1941738116631498. Level 2
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A
- ↑ Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013;43(4):267-286. Level 2A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A