Achilles Rupture: Difference between revisions
No edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- [[User:Sam Verhelpen|Sam Verhelpen]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | '''Original Editors ''' - [[User:Sam Verhelpen|Sam Verhelpen]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
| Line 52: | Line 52: | ||
== Examination == | == Examination == | ||
==== | ==== Observation ==== | ||
*A swollen ankle can point to a rupture of the Achilles tendon.<ref name="one" /><ref name="four" /><ref name="five" /> | *A swollen ankle can point to a rupture of the Achilles tendon.<ref name="one" /><ref name="four" /><ref name="five" /> | ||
| Line 61: | Line 61: | ||
==== Active Movements ==== | ==== Active Movements ==== | ||
*One of the first ways to see if a patient has torn his Achilles tendon is by observing his gait pattern. Plantar flexion is nearly if not totally impossible | *One of the first ways to see if a patient has torn his/her Achilles tendon is by observing his/her gait pattern. Plantar flexion is nearly if not totally impossible, so if the patient has a lot of trouble walking, it can be an indication of an Achilles rupture.<ref name="one" /><ref name="seven" /><ref name="five" /> | ||
*Instructing the patient to stand on his toes. With an Achilles rupture this will be impossible.<ref name="five" /> | *Instructing the patient to stand on his/her toes. With an Achilles rupture this will be impossible.<ref name="five" /> | ||
*Ask the patient to actively | *Ask the patient to actively plantar flex the ankle.<ref name="seven" /><ref name="five" /> | ||
*[[Matles Test|Matles test]] .<ref name="one" /><ref name="seven" /> | *[[Matles Test|Matles test]] .<ref name="one" /><ref name="seven" /> | ||
==== | ==== Special Tests ==== | ||
*[http://www.physio-pedia.com/index.php5?title=Thompson_Test Thompson test] (calf squeeze test). <ref name="one" /><ref name="seven" /><ref name="four" /><ref name="five" /><ref name="six" /> | *[http://www.physio-pedia.com/index.php5?title=Thompson_Test Thompson test] (calf squeeze test). <ref name="one" /><ref name="seven" /><ref name="four" /><ref name="five" /><ref name="six" /> | ||
== Medical Management ( | == Medical Management (Current Best Evidence) == | ||
Therapy for a patient with an Achilles tendon rupture consists of rest, pain control, and serial casting. It will involve having a plaster cast or brace for about eight weeks to protect the tendon while it heals. The plaster cast or brace is positioned so that the ankle is slightly plantar flexed, which takes the strain off the tendon. | |||
Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Now there is a trend towards early mobilisation. This involves fitting a plaster or brace which | Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Now there is a trend towards early mobilisation. This involves fitting a plaster or brace which one can walk on, <ref name="1">http://patient.info/health/achilles-tendon-rupture</ref> maing it more conventient as crutches will likely not be required. There is debate as to which treatment is best: surgery or conservative treatment. Conservative treatment may be suggested for older or less active people, and for people wishing to avoid surgery. But the choice of treatment depends on individual preference and circumstances. Surgery may also be recommended if there has been a delay in starting treatment. | ||
However, | However, new research has found surgery and conservative treatment demonstrated equally good results when patients were also given early mobilisation treatment using a brace.<ref name="1">http://patient.info/health/achilles-tendon-rupture</ref> | ||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Whether the tendon was treated surgically or non-surgically, the patient’s ankle will be immobilized by a cast for twelve weeks in case of surgery and 6 to 8 weeks when the condition | Whether the tendon was treated surgically or non-surgically, the patient’s ankle will be immobilized by a cast for twelve weeks in case of surgery and 6 to 8 weeks when the condition is treated non-surgically. | ||
Physical therapy for an Achilles tendon rupture starts immediately after the cast is removed and is mainly focused around firstly improving the range of motion (ROM) of the ankle, then increasing the muscle strength and muscle coordination<ref name="five" />. | |||
Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Ten weeks after the injury or surgery, start gait training exercises followed by activity specific movements. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient.<ref name="five" /> | Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Ten weeks after the injury or surgery, start gait training exercises followed by activity specific movements. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient.<ref name="five" /> | ||
| Line 88: | Line 90: | ||
Not all patients benefit from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes. <ref name="Roos">Roos, M.E., et al., ‘Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up’, Scand J Med Sci Sports, 2004, 14, p. 286-295.</ref> | Not all patients benefit from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes. <ref name="Roos">Roos, M.E., et al., ‘Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up’, Scand J Med Sci Sports, 2004, 14, p. 286-295.</ref> | ||
==== | ==== Sample Exercises<ref name="three" /> ==== | ||
At the start of the therapy, 6-8 weeks after surgery, let the patient do: | |||
*Active flexion/extension of the ankle | *Active flexion/extension of the ankle | ||
*Ankle circles (clockwise and counterclockwise) | *Ankle circles (clockwise and counterclockwise) | ||
*Straight leg lifts | *Straight leg lifts | ||
*Hip abduction | *Hip abduction | ||
*Standing | *Standing hamstring curl | ||
*Cycling on a stationary bicycle | *Cycling on a stationary bicycle | ||
8 | 8-12 weeks after surgery, the patient can start with a theraband exercise program (starting from least resistance and work up from there). The patient should also continue with the previous exercises. | ||
*Ankle eversion and eversion | *Ankle eversion and eversion | ||
*Ankle plantar- and dorsiflexion | *Ankle plantar- and dorsiflexion | ||
12 | 12-24 weeks after surgery, the first set of exercises can be executed with ankle weights. The following exercises can be added to the training program: | ||
*Calf stretch | *Calf stretch | ||
*Toe raises | *Toe raises | ||
*Single leg balancing | *Single leg balancing | ||
The last step | The last step after surgery is eccentric exercise. During the eccentric part (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is used. <ref name="Murali" /> | ||
*Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go stand on his/her toes and to raise the non-injured leg so that his/her bodyweight is on his injured leg. Now the patient slowly lowers the heel. In this way the calf muscle eccentrically guides the motion and is eccentrically trained. | |||
*Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go stand on his toes and to raise | *When the patient can perform this exercise without discomfort, he/she can increase the load by adding books or other weight to a backpack, or to perform the exercise with a flexed knee.<br> | ||
*When the patient can perform this exercise without discomfort he can increase the load by adding books or other weight to a backpack, or to perform the exercise with a flexed knee.<br> | |||
{{#ev:youtube|t0boD9MWRok}} | {{#ev:youtube|t0boD9MWRok}} | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid= | <div class="researchbox"> | ||
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zA4h3Qg-ND3LsxPmkSb0CBgv9Xvi2xKQrzC8J98U206JGxQIY|Short|max=10</rss> | |||
</div> | |||
== Reference == | == Reference == | ||
<references /> | <references /> | ||
<br> | |||
[[Category:Sports_Injuries]] [[Category:Ankle]] [[Category:Tendons]] [[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Ankle]] [[Category: | |||
Revision as of 08:01, 8 July 2016
Original Editors - Sam Verhelpen as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Yannick Goubert, Sam Verhelpen, Kim Jackson, Thorvald De Saeger, Rachael Lowe, Mariam Hashem, Shaimaa Eldib, Admin, Nick Libotton, Daphne Dörge, Uchechukwu Chukwuemeka, Tarina van der Stockt, Andeela Hafeez, Lucinda hampton, Lynn De Saegher, Magdalena Hytros, Wanda van Niekerk, Sweta Christian, 127.0.0.1, Yelena Gesthuizen, Evan Thomas, Oyemi Sillo, Claire Knott, Mandy Roscher, Jess Bell, Olajumoke Ogunleye, Robin Tacchetti, Alexandre Lheureux, Franca Ebomah, Kardelen Aktas, WikiSysop, Vidya Acharya, Naomi O'Reilly and Daphne Jackson
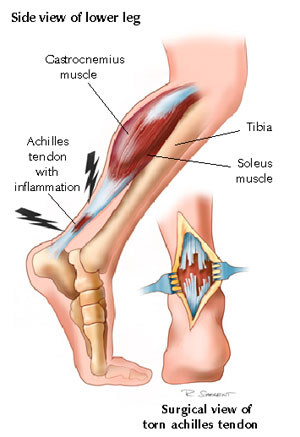
Definition/Description[edit | edit source]
Achilles tendon rupture is an injury that affects the back of your lower leg. It most commonly occurs in people playing recreational sports.The Achilles tendon is a strong fibrous cord that connects the muscles in the back of your calf to your heel bone. If you overstretch your Achilles tendon, it can tear (rupture) completely or just partially.If your Achilles tendon ruptures, you might feel a pop or snap, followed by an immediate sharp pain in the back of your ankle and lower leg that is likely to affect your ability to walk properly[1].
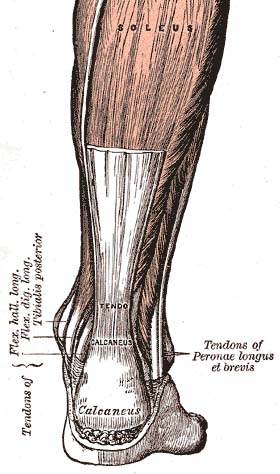
Relevant Anatomical Structures
[edit | edit source]
The Achilles tendon is the insertion of two lower leg muscles, the M. Soleus and the M. Gastrocnemius. These muscles are the main plantar flexors of the ankle. The Achilles tendon is the strongest and longest tendon in the body and connects these muscles to the calcaneal tuberosity[2][3]
Epidemiology /Etiology[edit | edit source]
An injury at the Achilles tendon usually occurs during sports that involve repeated stress on the lower leg muscles, such as badminton[2][4], soccer[4][5], volleyball[4], basketball[6][5], tennis[6][5], raquetball[6], squash[6]. Eccentric movement puts an enormous amount of stress on the tendon. An Achilles tendon rupture occurs more frequently in men than women, with a ratio ranging from 1.7:1 to 12:1[2]. The injury is most common in individuals between 30 to 50 years old[7].
Characteristics/Clinical Presentation[edit | edit source]
A complete rupture of the Achilles tendon will show the following characteristics:
- At the moment of rupture a sharp pain will be felt, as if the patient was kicked in the heel[2][7][3][8][5].
- Often the rupture will coincide with a loud crack or pop sound[2][5].
- When palpating the tendon, a gap may be felt[2][7][3].
- The back of the heel will be swollen[2][7][3].
- Walking will be nearly impossible[3].
- Standing on the toes will be impossible[3].
- A positive outcome of the calf muscle squeeze test or Thompson Test[2][7][3][8][5].
- Some patients will have a history of chronic tendonitis in the heel or a prior cortisone injection[2][7][3].
Differential Diagnosis[edit | edit source]
Differential diagnosis includes:
- Acute Achilles tendon peritendinitis[7][5]
- Tennis leg (medial gastrocnemius tear)[7][5]
- Calf muscle strain or rupture[3][5].
- Posterior tibialis stress syndrome[5]
- Ligament injuries[3][5]
- Fracture[7][5]
- Posterior tibialis tendon injuries[5]
- Peroneal injuries[5]
Examination[edit | edit source]
Observation[edit | edit source]
- A swollen ankle can point to a rupture of the Achilles tendon.[2][7][3]
- The Achilles tendon is easily palpable. When palpating along the entire length of the tendon, a gap may be present.[5][3]
It’s wise to compare to the healthy tendon on the other limb. Be aware that swelling can mask the gap[2][5]
Active Movements[edit | edit source]
- One of the first ways to see if a patient has torn his/her Achilles tendon is by observing his/her gait pattern. Plantar flexion is nearly if not totally impossible, so if the patient has a lot of trouble walking, it can be an indication of an Achilles rupture.[2][5][3]
- Instructing the patient to stand on his/her toes. With an Achilles rupture this will be impossible.[3]
- Ask the patient to actively plantar flex the ankle.[5][3]
- Matles test .[2][5]
Special Tests[edit | edit source]
Medical Management (Current Best Evidence)[edit | edit source]
Therapy for a patient with an Achilles tendon rupture consists of rest, pain control, and serial casting. It will involve having a plaster cast or brace for about eight weeks to protect the tendon while it heals. The plaster cast or brace is positioned so that the ankle is slightly plantar flexed, which takes the strain off the tendon.
Traditionally, crutches were used to keep weight off the leg during the first few weeks of treatment. Now there is a trend towards early mobilisation. This involves fitting a plaster or brace which one can walk on, Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title maing it more conventient as crutches will likely not be required. There is debate as to which treatment is best: surgery or conservative treatment. Conservative treatment may be suggested for older or less active people, and for people wishing to avoid surgery. But the choice of treatment depends on individual preference and circumstances. Surgery may also be recommended if there has been a delay in starting treatment.
However, new research has found surgery and conservative treatment demonstrated equally good results when patients were also given early mobilisation treatment using a brace.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Physical Therapy Management (current best evidence)[edit | edit source]
Whether the tendon was treated surgically or non-surgically, the patient’s ankle will be immobilized by a cast for twelve weeks in case of surgery and 6 to 8 weeks when the condition is treated non-surgically.
Physical therapy for an Achilles tendon rupture starts immediately after the cast is removed and is mainly focused around firstly improving the range of motion (ROM) of the ankle, then increasing the muscle strength and muscle coordination[3].
Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Ten weeks after the injury or surgery, start gait training exercises followed by activity specific movements. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient.[3]
When treated with an eccentric training program, the patient is more likely to be able to return faster to sport. The eccentric exercises should reduce pain an tendon thickness and should improve function of the tendon (and muscles). The eccentric calf-muscle exercises, as described below, should be executed twice daily for 12 weeks. The exercise program consists of one to three sets of 15 repetitions per exercise, according to the improvement of the patient. [9]
Not all patients benefit from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes. [10]
Sample Exercises[6][edit | edit source]
At the start of the therapy, 6-8 weeks after surgery, let the patient do:
- Active flexion/extension of the ankle
- Ankle circles (clockwise and counterclockwise)
- Straight leg lifts
- Hip abduction
- Standing hamstring curl
- Cycling on a stationary bicycle
8-12 weeks after surgery, the patient can start with a theraband exercise program (starting from least resistance and work up from there). The patient should also continue with the previous exercises.
- Ankle eversion and eversion
- Ankle plantar- and dorsiflexion
12-24 weeks after surgery, the first set of exercises can be executed with ankle weights. The following exercises can be added to the training program:
- Calf stretch
- Toe raises
- Single leg balancing
The last step after surgery is eccentric exercise. During the eccentric part (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is used. [9]
- Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go stand on his/her toes and to raise the non-injured leg so that his/her bodyweight is on his injured leg. Now the patient slowly lowers the heel. In this way the calf muscle eccentrically guides the motion and is eccentrically trained.
- When the patient can perform this exercise without discomfort, he/she can increase the load by adding books or other weight to a backpack, or to perform the exercise with a flexed knee.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zA4h3Qg-ND3LsxPmkSb0CBgv9Xvi2xKQrzC8J98U206JGxQIY|Short|max=10: Error parsing XML for RSS
Reference[edit | edit source]
- ↑ http://www.mayoclinic.org/diseases-conditions/achilles-tendon-rupture/basics/definition/con-20020370
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. Jul 1999;81(7):1019-36.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 Jacobs B, Lin D, Schwartz E. Achilles tendon rupture. Medscape 2009 [accessed 2014 May 29] http://emedicine.medscape.com/article/85024-overview
- ↑ 4.0 4.1 4.2 Leppilaht J, et al. Incidence of Achilles tendon rupture. Acta Ortbop Scand. 1996; 67 (3): 277-279.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 Gravlee J, Hatch R. Achilles tendon rupture: a challenging diagnosis. J Am Board Fam Med. 2000;13(5) http://www.medscape.com/viewarticle/405807
- ↑ 6.0 6.1 6.2 6.3 6.4 Berkson E. Achilles tendon rupture. Quincy medical center
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Saglimbeni A, Fulmer C. Achilles tendon injuries and tendonitis. Medscape 2009 [accessed 2014 May 29]. http://emedicine.medscape.com/article/309393-overview
- ↑ 8.0 8.1 8.2 Atkinson T, Easley M. Complete ruptures of the Achilles tendon. Medscape Orthopaedics Sports Medicine 2001;5(3) [accessed 2014 May 29] http://www.medscape.com/viewarticle/408535
- ↑ 9.0 9.1 Murali K. Sayana, Maffulli N., ‘Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy’, Journal of Science and Medicine in Sport, Volume 10, Issue 1, Feb. 2007, p. 52-58.
- ↑ Roos, M.E., et al., ‘Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up’, Scand J Med Sci Sports, 2004, 14, p. 286-295.