Achilles Rupture: Difference between revisions
Rachael Lowe (talk | contribs) mNo edit summary |
Rachael Lowe (talk | contribs) mNo edit summary |
||
| Line 15: | Line 15: | ||
The incidence is 7 per 100 000 per year but goes up to 15 to 25 per 100 000 per year for (recreational) athletes, with a peak incidence at the age of 30 to 50 years<ref name="p1">American college of foot and ankle surgeons/ foot health artikel. Achilles Tendon Rupture (2016 ) https://www.foothealthfacts.org/conditions/achilles-tendon-rupture</ref>. ‘ It affects mostly 'middle-aged weekend warriors' but this aetiology accounts for only about 70% of such injuries. | The incidence is 7 per 100 000 per year but goes up to 15 to 25 per 100 000 per year for (recreational) athletes, with a peak incidence at the age of 30 to 50 years<ref name="p1">American college of foot and ankle surgeons/ foot health artikel. Achilles Tendon Rupture (2016 ) https://www.foothealthfacts.org/conditions/achilles-tendon-rupture</ref>. ‘ It affects mostly 'middle-aged weekend warriors' but this aetiology accounts for only about 70% of such injuries. | ||
An achilles tendon rupture occurs more frequently among men than women<ref name=" | An achilles tendon rupture occurs more frequently among men than women<ref name=":0">Vosseller JT, Ellis SJ, Levine DS, Kennedy JG, Elliott AJ, Deland JT, Roberts MM, O’Malley MJ. [https://www.ncbi.nlm.nih.gov/pubmed/23386761/ Achilles tendon rupture in women]. Foot & ankle international. 2013 Jan;34(1):49-53.</ref>. | ||
== Aetiology == | == Aetiology == | ||
[[Image:Achilles tendon rupture.jpg|thumb|right|225x275px|Fig. 2 : achilles Tendon Rupture]]The inherent characteristics, function, and blood supply of the Achilles tendon predispose it to both acute and chronic rupture. | |||
In the situation of an acute rupture, patients are usually engaged in athletic activities<ref name=":0" />, accounting for 68 % of injuries<ref name=":1">Raikin SM, Garras DN, Krapchev PV. [https://www.ncbi.nlm.nih.gov/pubmed/23386750 Achilles tendon injuries in a United States Population]. Foot Ankle Int. 2013;34:475–480. doi: 10.1177/1071100713477621.</ref>. It is common in stop-and-go sports such as badminton, soccer, volleyball, basketball, tennis, racquetball, squash as eccentric movement puts an enormous amount of stress on the tendon. | |||
There are some conditions that predispose to rupture, research suggests that injuries in this patient population are more likely to be missed on first examination, these include: | There are some conditions that predispose to rupture, research suggests that injuries in this patient population are more likely to be missed on first examination<ref name=":1" />, these include: | ||
* | * The natural ageing process<ref name=":1" /> | ||
* | * Obesity<ref name=":1" /> | ||
* | * Use of some commonly prescribed medications such as fluoroquinolone and steroids | ||
* | * Poor running mechanics | ||
* Altered biomechanics such as flat foot (pes planus), high foot arch (pes cavus),and leg length discrepancy | |||
* flat foot (pes planus) | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Three categories of indirect injury that may result in rupture are<ref name="p3" />: | |||
# Pushing off with a weight bearing forefoot while also extending the knee, as occurs at the beginning of a sprint, running, and some forms of jumping | |||
# Sudden and unexpected dorsiflexion of the ankle, which may occur when a person slips off a chair or a ladder, when stumbling into a hole, or suddenly falling forward | |||
# Violent dorsiflexion of a plantar-flexed foot when one falls from a height. | |||
A complete rupture of the achilles tendon will show the following characteristics: | A complete rupture of the achilles tendon will show the following characteristics: | ||
* At the moment of rupture a sharp pain will be felt, as if the patient was stabbed in the heel with a dagger<ref name="p6">Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. Jul 1999;81(7):1019-36.</ref><ref name="p0" /><ref name="p7">Jacobs B, Lin D, Schwartz E. Achilles tendon rupture. Medscape 2009 [accessed 2014 May 29] fckLRhttp://emedicine.medscape.com/article/85024-overview</ref><ref name="p2" /><ref name="p8">Gravlee J, Hatch R. Achilles tendon rupture: a challenging diagnosis. J Am Board Fam Med. 2000;13(5) fckLRhttp://www.medscape.com/viewarticle/405807</ref><ref name="p1" />. | * At the moment of rupture a sharp pain will be felt, as if the patient was stabbed in the heel with a dagger<ref name="p6">Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. Jul 1999;81(7):1019-36.</ref><ref name="p0">Saglimbeni A, Fulmer C. Achilles tendon injuries and tendonitis. Medscape 2009 [accessed 2014 May 29]. fckLRhttp://emedicine.medscape.com/article/309393-overview</ref><ref name="p7">Jacobs B, Lin D, Schwartz E. Achilles tendon rupture. Medscape 2009 [accessed 2014 May 29] fckLRhttp://emedicine.medscape.com/article/85024-overview</ref><ref name="p2" /><ref name="p8">Gravlee J, Hatch R. Achilles tendon rupture: a challenging diagnosis. J Am Board Fam Med. 2000;13(5) fckLRhttp://www.medscape.com/viewarticle/405807</ref><ref name="p1" />. | ||
* Often the rupture will coincide with a loud crack or pop sound.<ref name="p6" /><ref name="p8" /> | * Often the rupture will coincide with a loud crack or pop sound.<ref name="p6" /><ref name="p8" /> | ||
* When palpating the tendon, a gap may be felt.<ref name="p6" /><ref name="p0" /><ref name="p7" /> | * When palpating the tendon, a gap may be felt.<ref name="p6" /><ref name="p0" /><ref name="p7" /> | ||
| Line 53: | Line 48: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
In most of the available literature, an achilles tendon rupture is described as chronic if it occurs at least 4 to 6 weeks after injury.<ref name="p3" /> The symptoms of chronic achilles tendon rupture include pain, decreased strength, fatigue, and ankle stiffness.<ref name="p5"/> Acute ATR’s represent those less than 7 days from insult.<ref name="p3" /> A correct distinction needs to be made, because the treatments differ.<ref name="p6"/> | In most of the available literature, an achilles tendon rupture is described as chronic if it occurs at least 4 to 6 weeks after injury.<ref name="p3" /> The symptoms of chronic achilles tendon rupture include pain, decreased strength, fatigue, and ankle stiffness.<ref name="p5">2016 Mar;23(10):34-6; quiz p 37. doi: 10.7748/en.23.10.34.s24. Achilles tendon rupture in atypical patient populations. fckLRKingsley P1. 1South East Coast Ambulance Service NHS Foundation Trust, Surrey</ref> Acute ATR’s represent those less than 7 days from insult.<ref name="p3" /> A correct distinction needs to be made, because the treatments differ.<ref name="p6"/> | ||
Differential diagnosis includes: | Differential diagnosis includes: | ||
| Line 80: | Line 75: | ||
== Examination == | == Examination == | ||
''' | '''Observation''' | ||
For the inspection of an ATR, the therapist may observe the patient in several positions: | |||
# Standing - to look for fallen arches (flat feet) and other postural complications. | |||
# Laying - usually on the front. This can be used to observe the tendon more closely for thickening, redness, swelling and nodules. | |||
# Walking and running - to look for overpronation. | |||
# Swelling: a swollen ankle can point to a rupture of the achilles tendon.<ref name="p7" /><ref name="p8" /><ref name="p9" /><ref name="p0" /> | |||
# On palpation: The achilles tendon is easily palpable. When palpating along the entire length of the tendon, a gap may be present. <ref name="p0" /><ref name="p1" /> | |||
'''Active Movements''' | |||
In this part of the examination the therapist asks the patient to fulfil some active movements which can aid in the diagnosis of a tendon rupture. | |||
There are several active movements: | |||
# Observing the gait pattern can be an important indication for a possible rupture. A patient with an ATR can possibly not make a plantar flexion of his ankle. So if the plantar flexion movement in the walking phase is hindered and painful, it can be an indication of an achilles rupture. <ref name="p7" /><ref name="p9" /><ref name="p1" /> A patient with a achilles rupture will show an overpronation of the injured ankle. The patient will also show a lack of push-off at the end of the stance phase as a result of the dysfunction of the Gastrocnemius and Soleus muscles.<ref name="p1" /> | |||
# Instructing the patient to stand on his/her toes for making a plantar flexion. This will be impossible if the patient has an ATR. <ref name="p0" /> | |||
# Ask the patient to actively plantar flex the ankle. <ref name="p0" /><ref name="p1" /> | |||
# Every active movement containing a plantar flexion of the heel will be almost, if totally not impossible. <ref name="p7" /><ref name="p2" /> | |||
'''Special Test''' | |||
<br> | There exist several special tests for the observation of an ATR: | ||
# <u>The [[Thompson Test|Thompson Test]]/calf squeeze test</u>: <ref name="p3" /><ref name="p7" /><ref name="p8" /><br> This test is especially useful for diagnosing complete achilles tendon ruptures and less useful for the diagnosis of partial ATR. <ref name="p4" /> | |||
# <u>Matles Test</u> <ref name="p5" />The patient lies in prone position and is asked to actively flex the knee through 90 degrees. The therapeut observes the feet and ankles throughout the movement. The test is negative when the foot displays slight plantar flexion; the test is positive if the foot falls into the neutral position or the movement results in dorsiflexion. Maffulli reports a sensitivity of 0.88. <ref name="p2" /><ref name="p3" /> | |||
# <u>achilles Tendon Total Rupture</u> (ATR-score)<br> (level of evidence 1A) <ref name="p9" /><ref name="p1" /><br> The ATR-score is an important questionnaire that <br> refers to the limitations/difficulties a patient with <br> a tendon rupture will face. <ref name="p9" /><ref name="p1" /> | |||
# <u>Realtime achilles Ultrasound Thompson Test</u><br> (level of evidence 2) <ref name="p6" /><br>This test is exactly similar to the Thompson test, but under ultrasound visualization. It can be used by surgeons with minimal training in ultrasonography. It provides improved diagnostic characteristics compared with static ultrasound. <ref name="p6" /><br><br>[[Image:AngleOfDangle1.jpg|thumb|left|200x200px|Fig. 3 : Matles Test (1)]] [[Image:MatlesTest1.jpg|thumb|center|200x200px|Fig. 4: Matles Test (2)]] | |||
== Management == | |||
There is still considerable controversy as the most optimal treatment plan. Debate about nonoperative vs surgical repair for acute ruptures, minimally invasive vs traditional open repair, and early functional rehabilitation protocols instead of a more traditional rehabilitation program are only a few of the arguments that continue to exist in the realm of treatment. | |||
== Surgical management == | |||
== | |||
After medical diagnosis of an achilles Tendon Rupture (ATR) different kinds of therapy can be offered and evaluated. These repair methods can be either by surgery or in a non-operative way where the tendon cures in a natural way with support of a brace and rest <ref name="p2" />. The results of a systematic review of Wu, Yaohong, et al (level of evidence 1a) showed that when functional rehabilitation was used, the effect of non-surgical intervention was similar to surgical treatment regarding the incidence of range of motion, a future chance of rerupture, calf circumference and functional outcomes and also the incidence of other complications was reduced. Non-surgical intervention significantly increased the rerupture rate if functional rehabilitation was not considered <ref name="p3" />. | After medical diagnosis of an achilles Tendon Rupture (ATR) different kinds of therapy can be offered and evaluated. These repair methods can be either by surgery or in a non-operative way where the tendon cures in a natural way with support of a brace and rest <ref name="p2" />. The results of a systematic review of Wu, Yaohong, et al (level of evidence 1a) showed that when functional rehabilitation was used, the effect of non-surgical intervention was similar to surgical treatment regarding the incidence of range of motion, a future chance of rerupture, calf circumference and functional outcomes and also the incidence of other complications was reduced. Non-surgical intervention significantly increased the rerupture rate if functional rehabilitation was not considered <ref name="p3" />. | ||
| Line 108: | Line 111: | ||
<u>Chronic ATR [[Image:ATR Medical.jpg|thumb|right|300x225px|Fig. 5 : Treatment strategy for chronic achilles tendon rupture]]<br>By evaluating the presence or absence of achilles tendon stumps and the gap length of the rupture, different surgical options (V-Y advancement, gastrocnemius fascial turndown flap, or flexor halluces longus tendon transfer) can be selected for tendon repair (figure: 6) Yangjing Lin et al (level of evidence 2b)) <ref name="p0"/>. | <u>Chronic ATR [[Image:ATR Medical.jpg|thumb|right|300x225px|Fig. 5 : Treatment strategy for chronic achilles tendon rupture]]<br>By evaluating the presence or absence of achilles tendon stumps and the gap length of the rupture, different surgical options (V-Y advancement, gastrocnemius fascial turndown flap, or flexor halluces longus tendon transfer) can be selected for tendon repair (figure: 6) Yangjing Lin et al (level of evidence 2b)) <ref name="p0"/>. | ||
<u>Acute ATR</u><br>Due to a high complication rate after open surgical repair, including wound infection, abnormal sensation, adhesion and thrombosis new technics which require much smaller incisions have been developed and are published in specialised literature <ref name="p1" />. Minimal invasive technics and percutaneous repair become more and more common because they reduce the above mentioned complications and have both a good outcome, as described in the literature of Carmont et al (level of evidence 3a) <ref name="p1"/>.<br>There is ongoing controversy about the best post-operative treatment. A few randomised controlled trials (level of evidence 1b) have been published comparing early mobilization with immobilization after surgery. Most studies have shown slightly better results with early mobilisation or no difference in outcome. Anyway most studies agree early functional treatment is recommended <ref name="p1" /><ref name="p2"/>.<br> <br>Post-operative immobilization consists of rest by wearing a protective plaster cast or brace for about 8 weeks. Partial-weight-bearing crutches can be used 6 weeks after surgery, but strenuous sports (such as running) can only be practiced 1 year postoperatively <ref name="p0" />.<br> <br>More recent studies however tend to an early mobilisation. The objective is to work actively on the recovery, to prevent muscle atrophy and to regain strength and movement after surgery as a tendon requires movement to heal <ref name="p1" />. These exercises are performed in the first 6 to 8 weeks after surgery with a below-knee brace which allows free plantar flexion of the ankle and walking <ref name="p2" />.<br> <br>The systematic review of Wu Yaohong, et al (level of evidence 1a) concludes that the findings of meta-analyses regarding surgical versus non-surgical treatment for acute achilles tendon rupture are inconsistent. The current best available evidence suggests that a functional rehabilitation is recommended after a non-surgical intervention. If functional rehabilitation can’t be provided by a rehabilitation centre, a surgical treatment may be preferred for the healing of an acute achilles tendon rupture. <ref name="p3"/><br><br> | <u>Acute ATR</u><br>Due to a high complication rate after open surgical repair, including wound infection, abnormal sensation, adhesion and thrombosis new technics which require much smaller incisions have been developed and are published in specialised literature <ref name="p1" />. Minimal invasive technics and percutaneous repair become more and more common because they reduce the above mentioned complications and have both a good outcome, as described in the literature of Carmont et al (level of evidence 3a) <ref name="p1" />.<br>There is ongoing controversy about the best post-operative treatment. A few randomised controlled trials (level of evidence 1b) have been published comparing early mobilization with immobilization after surgery. Most studies have shown slightly better results with early mobilisation or no difference in outcome. Anyway most studies agree early functional treatment is recommended <ref name="p1" /><ref name="p2" />.<br> <br>Post-operative immobilization consists of rest by wearing a protective plaster cast or brace for about 8 weeks. Partial-weight-bearing crutches can be used 6 weeks after surgery, but strenuous sports (such as running) can only be practiced 1 year postoperatively <ref name="p0" />.<br> <br>More recent studies however tend to an early mobilisation. The objective is to work actively on the recovery, to prevent muscle atrophy and to regain strength and movement after surgery as a tendon requires movement to heal <ref name="p1" />. These exercises are performed in the first 6 to 8 weeks after surgery with a below-knee brace which allows free plantar flexion of the ankle and walking <ref name="p2" />.<br> <br>The systematic review of Wu Yaohong, et al (level of evidence 1a) concludes that the findings of meta-analyses regarding surgical versus non-surgical treatment for acute achilles tendon rupture are inconsistent. The current best available evidence suggests that a functional rehabilitation is recommended after a non-surgical intervention. If functional rehabilitation can’t be provided by a rehabilitation centre, a surgical treatment may be preferred for the healing of an acute achilles tendon rupture. <ref name="p3" /><br><br><br> | ||
<br> | |||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
On day 0, in the emergency department the diagnosis is made based on the following criteria :<br>1) a patient’s history with a clear sense of “snap” of the achilles tendon<br>2) a palpable defect, usually located 3–6 cm above the calcaneal tubercle<br>3) a positive calf squeeze test <ref name="p0"/>. A plaster of Paris is applied to the patient’s foot in a <br> plantigrade position of 30–45 degrees. No weight bearing is allowed. | On day 0, in the emergency department the diagnosis is made based on the following criteria :<br>1) a patient’s history with a clear sense of “snap” of the achilles tendon<br>2) a palpable defect, usually located 3–6 cm above the calcaneal tubercle<br>3) a positive calf squeeze test <ref name="p0" />. A plaster of Paris is applied to the patient’s foot in a <br> plantigrade position of 30–45 degrees. No weight bearing is allowed. | ||
<u>Week 0-6</u><br>Whether the tendon was treated surgically or non-surgically, the patient should wear a plaster cast for immobilization for at least 6 weeks on the injured ankle or a below-knee dorsal brace which allows the ankle to make a plantar flexion to start early mobilization in the first 6 weeks after injury or surgery as described in Groetelaers, René et al.(level of evidence 1b (prospective randomized trial))<ref name="p1" /> . Lantto, Iikka, et al. level of evidence 1b (RCT) <ref name="p2" /> .<br><br>'''Rehabilitation schedule and sample physiotherapy exercises''' <ref name="p5"/> | <u>Week 0-6</u><br>Whether the tendon was treated surgically or non-surgically, the patient should wear a plaster cast for immobilization for at least 6 weeks on the injured ankle or a below-knee dorsal brace which allows the ankle to make a plantar flexion to start early mobilization in the first 6 weeks after injury or surgery as described in Groetelaers, René et al.(level of evidence 1b (prospective randomized trial))<ref name="p1" /> . Lantto, Iikka, et al. level of evidence 1b (RCT) <ref name="p2" /> .<br><br>'''Rehabilitation schedule and sample physiotherapy exercises''' <ref name="p5" /> | ||
In general physical therapy for an achilles tendon rupture starts immediately after the cast is removed and is mainly focused on firstly improving the range of motion (ROM) of the ankle. Later the physical therapy is focussed on increasing the muscle strength and muscle coordination <ref name="p4"/>. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient <ref name="p4" />.<br><br> | In general physical therapy for an achilles tendon rupture starts immediately after the cast is removed and is mainly focused on firstly improving the range of motion (ROM) of the ankle. Later the physical therapy is focussed on increasing the muscle strength and muscle coordination <ref name="p4" />. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient <ref name="p4" />.<br><br> | ||
► At the start of the therapy until 6-8 weeks after surgery : <br>Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Possible exercises for the patient are :<br>● Active flexion/extension of the ankle<br>● Ankle circles (clockwise and counterclockwise)<br>● Hip abduction<br>● Straight leg raise<br>[[Image:Straight leg Raise.jpg|thumb|left|330x225px|Fig. 6 : Straight Leg Raise Test]]<br> | ► At the start of the therapy until 6-8 weeks after surgery : <br>Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Possible exercises for the patient are :<br>● Active flexion/extension of the ankle<br>● Ankle circles (clockwise and counterclockwise)<br>● Hip abduction<br>● Straight leg raise<br>[[Image:Straight leg Raise.jpg|thumb|left|330x225px|Fig. 6 : Straight Leg Raise Test]]<br> | ||
| Line 154: | Line 155: | ||
● Cycling on a stationary bicycle<br> | ● Cycling on a stationary bicycle<br> | ||
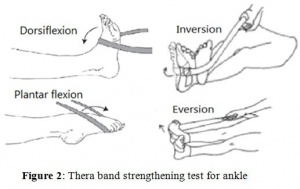
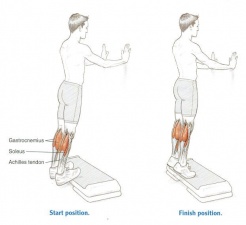
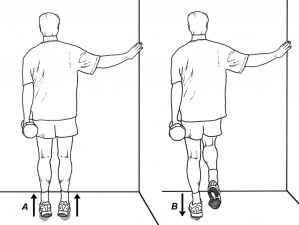
<br>► 8-12 weeks after surgery : <br>Ten weeks after the injury or surgery, gait training exercises can be started, followed by activity specific movements. The patient can start with a thera-band exercise program by starting from the lowest resistance and work up from there for regaining strength. The patient should also continue with the previous exercises. [[Image:Theraband.jpg|thumb|right|300x250px|Fig. 8: Thera-Band exercises]]<br>● Ankle range of motion : plantar flexion and dorsiflexion to 90° : 2 x 8 repetitions<br>● Ankle range of motion : inversion and eversion<br>● Ankle range of motion : pronation and supination : 2 x 8 repetitions<br>● One leg standing balance exercise : 3 × 30 seconds <ref name="p8"/><ref name="p9"/><br>● Standing heel-rise (2 × 3 seconds tempo) : 3 × 10 repetitions<br>[[Image:Standing Heel Rise.jpg|thumb|left|300x225px|Fig. 9 : Standing Heel-Rise Test]]<br> <br> | <br>► 8-12 weeks after surgery : <br>Ten weeks after the injury or surgery, gait training exercises can be started, followed by activity specific movements. The patient can start with a thera-band exercise program by starting from the lowest resistance and work up from there for regaining strength. The patient should also continue with the previous exercises. [[Image:Theraband.jpg|thumb|right|300x250px|Fig. 8: Thera-Band exercises]]<br>● Ankle range of motion : plantar flexion and dorsiflexion to 90° : 2 x 8 repetitions<br>● Ankle range of motion : inversion and eversion<br>● Ankle range of motion : pronation and supination : 2 x 8 repetitions<br>● One leg standing balance exercise : 3 × 30 seconds <ref name="p8" /><ref name="p9" /><br>● Standing heel-rise (2 × 3 seconds tempo) : 3 × 10 repetitions<br>[[Image:Standing Heel Rise.jpg|thumb|left|300x225px|Fig. 9 : Standing Heel-Rise Test]]<br> <br> | ||
<br> | <br> | ||
| Line 186: | Line 187: | ||
<br>► Starting from week 14 until the end of the therapy <br>The patient is able to run approximately 14 weeks after the injury or surgery.<br>● Running on even ground is allowed when the patient can perform 5 single-legged heel-rises with approximately 90% of the height of the <br> uninjured leg. <ref name="p8" /><ref name="p9" /><br>● Jogging upwards on stairs is allowed if the patient can walk 5 meters on their toes without the heel falling down. | <br>► Starting from week 14 until the end of the therapy <br>The patient is able to run approximately 14 weeks after the injury or surgery.<br>● Running on even ground is allowed when the patient can perform 5 single-legged heel-rises with approximately 90% of the height of the <br> uninjured leg. <ref name="p8" /><ref name="p9" /><br>● Jogging upwards on stairs is allowed if the patient can walk 5 meters on their toes without the heel falling down. | ||
The last step after surgery is eccentric exercise. During the eccentric part (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is used <ref name="p6"/>. | The last step after surgery is eccentric exercise. During the eccentric part (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is used <ref name="p6" />. | ||
• Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go <br> stand on his/her toes and to raise the non-injured leg so that his/her bodyweight is on his injured leg. Now the patient slowly lowers the <br> heel. In this way the calf muscle eccentrically guides the motion and is eccentrically trained.<br>• When the patient can perform this exercise without discomfort, he/she can increase the load by adding books or other weight to a <br> backpack, or to perform the exercise with a flexed knee. | • Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go <br> stand on his/her toes and to raise the non-injured leg so that his/her bodyweight is on his injured leg. Now the patient slowly lowers the <br> heel. In this way the calf muscle eccentrically guides the motion and is eccentrically trained.<br>• When the patient can perform this exercise without discomfort, he/she can increase the load by adding books or other weight to a <br> backpack, or to perform the exercise with a flexed knee. | ||
When treated with an eccentric training program, the patient is more likely to be able to return faster to sport. The eccentric exercises should reduce pain and tendon thickness and should improve function of the tendon (and muscles). The eccentric calf-muscle exercises, as described below, should be executed twice daily for 12 weeks. The exercise program consists of 1-3sets of 15 repetitions per exercise, according to the improvement of the patient as described in . Murali K. Sayana, Maffulli N. et al, level of evidence 2b (individual cohort study) <ref name="p6" />. <br>But not all patients benefit equally from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes (Roos, M.E., et al., level of evidence 1b) <ref name="p7"/>. | When treated with an eccentric training program, the patient is more likely to be able to return faster to sport. The eccentric exercises should reduce pain and tendon thickness and should improve function of the tendon (and muscles). The eccentric calf-muscle exercises, as described below, should be executed twice daily for 12 weeks. The exercise program consists of 1-3sets of 15 repetitions per exercise, according to the improvement of the patient as described in . Murali K. Sayana, Maffulli N. et al, level of evidence 2b (individual cohort study) <ref name="p6" />. <br>But not all patients benefit equally from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes (Roos, M.E., et al., level of evidence 1b) <ref name="p7" />. | ||
► End of the therapy : <br>After completing the rehabilitation program, new examination of the tendon healing and functions is required. If needed, a new referral for further physiotherapy sessions can be provided to the patient. Gradual return to sports is recommended. For example before participating to contact sports, the patient should wait at least 6–9 months after the injury. (Nilsson-Helander K, et al. level of evidence 1b <ref name="p8" /> Willits K, Et al.level of evidence 1b <ref name="p9" />).<br><br> | ► End of the therapy : <br>After completing the rehabilitation program, new examination of the tendon healing and functions is required. If needed, a new referral for further physiotherapy sessions can be provided to the patient. Gradual return to sports is recommended. For example before participating to contact sports, the patient should wait at least 6–9 months after the injury. (Nilsson-Helander K, et al. level of evidence 1b <ref name="p8" /> Willits K, Et al.level of evidence 1b <ref name="p9" />).<br><br> | ||
== Key Evidence | == Key Evidence == | ||
Links and reviews of high evidence can be added here.<br> | Links and reviews of high evidence can be added here.<br> | ||
== Resources | == Resources == | ||
• American Journal of Sports Medicine<br>• American Journal of Orthopedics<br>• Foot and Ankle International<br>• The Journal of Foot and Ankle Injury<br>• International Journey of Surgery<br><br> | • American Journal of Sports Medicine<br>• American Journal of Orthopedics<br>• Foot and Ankle International<br>• The Journal of Foot and Ankle Injury<br>• International Journey of Surgery<br><br> | ||
== Clinical Bottom Line | == Clinical Bottom Line == | ||
An achilles Tendon Rupture also known as ATR is described as a typical sports-related pathology. We distinguish two sorts of ruptures: a complete rupture or a partial rupture. An ATR can be treated surgically or nonsurgically. Medical therapy consists of an operative repair by sewing the torn ends of the injured achilles tendon together. The physical rehabilitation changes from physical non-weight bearing exercises (at the beginning of the therapy) to more weightbearing exercises at the end of the revalidation.<br><br> | An achilles Tendon Rupture also known as ATR is described as a typical sports-related pathology. We distinguish two sorts of ruptures: a complete rupture or a partial rupture. An ATR can be treated surgically or nonsurgically. Medical therapy consists of an operative repair by sewing the torn ends of the injured achilles tendon together. The physical rehabilitation changes from physical non-weight bearing exercises (at the beginning of the therapy) to more weightbearing exercises at the end of the revalidation.<br><br> | ||
| Line 222: | Line 223: | ||
<br> | <br> | ||
[[Category:Tendons]] [[Category:Ankle]] [[Category:Sports_Injuries]] [[Category:Foot_and_Ankle_Conditions]] [[Category:Musculoskeletal/Orthopaedics]] | [[Category:Tendons]] | ||
[[Category:Ankle]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Foot_and_Ankle_Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
Revision as of 13:39, 13 November 2017
Original Editors - Sam Verhelpen as part of the Vrije Universiteit Brussel Evidence-based Practice Project
Top Contributors - Yannick Goubert, Sam Verhelpen, Kim Jackson, Thorvald De Saeger, Rachael Lowe, Mariam Hashem, Shaimaa Eldib, Admin, Nick Libotton, Daphne Dörge, Uchechukwu Chukwuemeka, Andeela Hafeez, Tarina van der Stockt, Lucinda hampton, Lynn De Saegher, Magdalena Hytros, Wanda van Niekerk, Sweta Christian, 127.0.0.1, Yelena Gesthuizen, Evan Thomas, Oyemi Sillo, Claire Knott, Olajumoke Ogunleye, Robin Tacchetti, Alexandre Lheureux, Franca Ebomah, Kardelen Aktas, WikiSysop, Vidya Acharya, Naomi O'Reilly, Daphne Jackson, Mandy Roscher and Jess Bell
Introduction[edit | edit source]
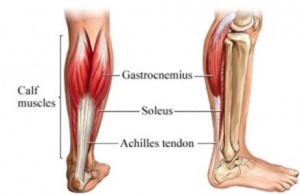
The achilles tendon is the strong fibrous band that attaches the calf muscles to the calcaneus bone. A rupture of the achilles tendon is a common pathology and it is the most commonly ruptured tendon in the human body[1]. The main causes of a rupture can be overstretching of the heel during recreational sports, a forceful plantar flexion of the heel or a fall from an important height[2]. .
Clinically relevant anatomy[edit | edit source]
The achilles tendon is the longest and strongest tendon in the whole human body and consists of strong, inelastic fibrous connective tissue. It is the insertion of the soleus and gastrocnemius muscles and connects these muscles to the calcaneal tuberosity. These claf muscles are the main plantar flexors of the ankle.
Epidemiology[edit | edit source]
The incidence is 7 per 100 000 per year but goes up to 15 to 25 per 100 000 per year for (recreational) athletes, with a peak incidence at the age of 30 to 50 years[3]. ‘ It affects mostly 'middle-aged weekend warriors' but this aetiology accounts for only about 70% of such injuries.
An achilles tendon rupture occurs more frequently among men than women[4].
Aetiology[edit | edit source]
The inherent characteristics, function, and blood supply of the Achilles tendon predispose it to both acute and chronic rupture.
In the situation of an acute rupture, patients are usually engaged in athletic activities[4], accounting for 68 % of injuries[5]. It is common in stop-and-go sports such as badminton, soccer, volleyball, basketball, tennis, racquetball, squash as eccentric movement puts an enormous amount of stress on the tendon.
There are some conditions that predispose to rupture, research suggests that injuries in this patient population are more likely to be missed on first examination[5], these include:
- The natural ageing process[5]
- Obesity[5]
- Use of some commonly prescribed medications such as fluoroquinolone and steroids
- Poor running mechanics
- Altered biomechanics such as flat foot (pes planus), high foot arch (pes cavus),and leg length discrepancy
Characteristics/Clinical Presentation[edit | edit source]
Three categories of indirect injury that may result in rupture are[2]:
- Pushing off with a weight bearing forefoot while also extending the knee, as occurs at the beginning of a sprint, running, and some forms of jumping
- Sudden and unexpected dorsiflexion of the ankle, which may occur when a person slips off a chair or a ladder, when stumbling into a hole, or suddenly falling forward
- Violent dorsiflexion of a plantar-flexed foot when one falls from a height.
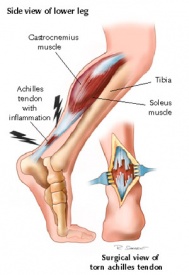
A complete rupture of the achilles tendon will show the following characteristics:
- At the moment of rupture a sharp pain will be felt, as if the patient was stabbed in the heel with a dagger[6][7][8][1][9][3].
- Often the rupture will coincide with a loud crack or pop sound.[6][9]
- When palpating the tendon, a gap may be felt.[6][7][8]
- The back of the heel will be swollen.[6][7][8]
- Decreased active plantar flexion of the ankle.[3]
- Increased passive dorsoflexion
- inability to heel raise
- Impaired gait
- A positive outcome of the calf muscle squeeze test or Thompson Test.
- Some patients will have a history of tendinopathy in the heel or a prior cortisone injection.[6][7][8]
Differential Diagnosis[edit | edit source]
In most of the available literature, an achilles tendon rupture is described as chronic if it occurs at least 4 to 6 weeks after injury.[2] The symptoms of chronic achilles tendon rupture include pain, decreased strength, fatigue, and ankle stiffness.[10] Acute ATR’s represent those less than 7 days from insult.[2] A correct distinction needs to be made, because the treatments differ.[6]
Differential diagnosis includes:
- Acute achilles tendon peritendinitis [7][9]
- Gastrocnemius tear)[7][9]
- Calf muscle strain or rupture[10][9]
- Posterior tibialis stress syndrome[9]
- Ligament injuries[10][9]
- Fracture[7][9]
- Posterior tibialis tendon injuries[9]
- Peroneal injuries[9]
Classification[edit | edit source]
Achilles tendon tears may be grouped into 4 types, according to severity of the tear and degree of retraction:
- type I: partial ruptures ≤50% - typically treated with conservative management
- type II: complete rupture with tendinous gap ≤3 cm - typically treated with end-end anastomosis
- type III: complete rupture with tendinous gap 3 to 6 cm - often requires tendon/synthetic graft
- type IV: complete rupture with defect of >6 cm (neglected ruptures) - often requires tendon/synthetic graft and gastrocnemius recession
Outcome Measures[edit | edit source]
The outcome measures used to evaluate functional results following an ATR can be broadly divided into two types: objective measures and patient-reported measures. The former are parameters directly registered by the physiotherapist, such as ankle range of motion (ROM) or calf muscle strength measurements. These objective data, derived from the patient’s physical examination, have traditionally formed the basis of functional assessment following an ATR.[9][7][11] However, over the past two decades, it has become increasingly recognized that the patient’s own appraisal of outcome is of the most important when judging the results of a treatment. [11]
The best choice of outcome tools for reporting the results of treatment in patients with foot and ankle disorders remains uncertain and controversial. Nevertheless, on the basis of the available evidence, a patient treated for an ATR should be assessed with a disease-specific measure, such as the ATRS[11][3] in combination with a generic measure, such as the SF-36 [10][6]. The 36-item Short Form (SF-36) is a commonly used instrument for measuring the Health Related Quality of Life, it is a valid and reliable tool. The SF-36 has been proven useful in monitoring population health, estimating the burdens of different diseases, monitoring outcome in clinical practice, and evaluating medical treatment effects.[6] . These patient-reported outcome scales focus on the patient’s perception of his/her health status, which has to be considered as the most important indicator of the success of a treatment. Patient-reported outcome scales should be complemented by objective indicators of function, such as muscle strength [1][2], calf muscle endurance [12] and return to previous activity level, in order to obtain a complete picture of the effect of the treatment. [11]
Examination[edit | edit source]
Observation
For the inspection of an ATR, the therapist may observe the patient in several positions:
- Standing - to look for fallen arches (flat feet) and other postural complications.
- Laying - usually on the front. This can be used to observe the tendon more closely for thickening, redness, swelling and nodules.
- Walking and running - to look for overpronation.
- Swelling: a swollen ankle can point to a rupture of the achilles tendon.[8][9][11][7]
- On palpation: The achilles tendon is easily palpable. When palpating along the entire length of the tendon, a gap may be present. [7][3]
Active Movements
In this part of the examination the therapist asks the patient to fulfil some active movements which can aid in the diagnosis of a tendon rupture.
There are several active movements:
- Observing the gait pattern can be an important indication for a possible rupture. A patient with an ATR can possibly not make a plantar flexion of his ankle. So if the plantar flexion movement in the walking phase is hindered and painful, it can be an indication of an achilles rupture. [8][11][3] A patient with a achilles rupture will show an overpronation of the injured ankle. The patient will also show a lack of push-off at the end of the stance phase as a result of the dysfunction of the Gastrocnemius and Soleus muscles.[3]
- Instructing the patient to stand on his/her toes for making a plantar flexion. This will be impossible if the patient has an ATR. [7]
- Ask the patient to actively plantar flex the ankle. [7][3]
- Every active movement containing a plantar flexion of the heel will be almost, if totally not impossible. [8][1]
Special Test
There exist several special tests for the observation of an ATR:
- The Thompson Test/calf squeeze test: [2][8][9]
This test is especially useful for diagnosing complete achilles tendon ruptures and less useful for the diagnosis of partial ATR. [12] - Matles Test [10]The patient lies in prone position and is asked to actively flex the knee through 90 degrees. The therapeut observes the feet and ankles throughout the movement. The test is negative when the foot displays slight plantar flexion; the test is positive if the foot falls into the neutral position or the movement results in dorsiflexion. Maffulli reports a sensitivity of 0.88. [1][2]
- achilles Tendon Total Rupture (ATR-score)
(level of evidence 1A) [11][3]
The ATR-score is an important questionnaire that
refers to the limitations/difficulties a patient with
a tendon rupture will face. [11][3] - Realtime achilles Ultrasound Thompson Test
(level of evidence 2) [6]
This test is exactly similar to the Thompson test, but under ultrasound visualization. It can be used by surgeons with minimal training in ultrasonography. It provides improved diagnostic characteristics compared with static ultrasound. [6]
Management[edit | edit source]
There is still considerable controversy as the most optimal treatment plan. Debate about nonoperative vs surgical repair for acute ruptures, minimally invasive vs traditional open repair, and early functional rehabilitation protocols instead of a more traditional rehabilitation program are only a few of the arguments that continue to exist in the realm of treatment.
Surgical management[edit | edit source]
After medical diagnosis of an achilles Tendon Rupture (ATR) different kinds of therapy can be offered and evaluated. These repair methods can be either by surgery or in a non-operative way where the tendon cures in a natural way with support of a brace and rest [1]. The results of a systematic review of Wu, Yaohong, et al (level of evidence 1a) showed that when functional rehabilitation was used, the effect of non-surgical intervention was similar to surgical treatment regarding the incidence of range of motion, a future chance of rerupture, calf circumference and functional outcomes and also the incidence of other complications was reduced. Non-surgical intervention significantly increased the rerupture rate if functional rehabilitation was not considered [2].
The choice which one will be applied depends on personal factors such as age of the patient, desire to have a sportive life afterwards and the individual preference. Operative repair by sewing the torn ends of the injured achilles tendon together will reduce risk of a future rerupture but wound infection can be a possible complication factor [3]. Therefore younger persons are recommended to choose for the operative repair and elderly and less active patients will be recommended for a more conservative, natural healing process [3].
There is a difference between surgery for chronic and acute ATR.
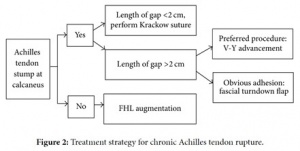
Chronic ATR
By evaluating the presence or absence of achilles tendon stumps and the gap length of the rupture, different surgical options (V-Y advancement, gastrocnemius fascial turndown flap, or flexor halluces longus tendon transfer) can be selected for tendon repair (figure: 6) Yangjing Lin et al (level of evidence 2b)) [7].
Acute ATR
Due to a high complication rate after open surgical repair, including wound infection, abnormal sensation, adhesion and thrombosis new technics which require much smaller incisions have been developed and are published in specialised literature [3]. Minimal invasive technics and percutaneous repair become more and more common because they reduce the above mentioned complications and have both a good outcome, as described in the literature of Carmont et al (level of evidence 3a) [3].
There is ongoing controversy about the best post-operative treatment. A few randomised controlled trials (level of evidence 1b) have been published comparing early mobilization with immobilization after surgery. Most studies have shown slightly better results with early mobilisation or no difference in outcome. Anyway most studies agree early functional treatment is recommended [3][1].
Post-operative immobilization consists of rest by wearing a protective plaster cast or brace for about 8 weeks. Partial-weight-bearing crutches can be used 6 weeks after surgery, but strenuous sports (such as running) can only be practiced 1 year postoperatively [7].
More recent studies however tend to an early mobilisation. The objective is to work actively on the recovery, to prevent muscle atrophy and to regain strength and movement after surgery as a tendon requires movement to heal [3]. These exercises are performed in the first 6 to 8 weeks after surgery with a below-knee brace which allows free plantar flexion of the ankle and walking [1].
The systematic review of Wu Yaohong, et al (level of evidence 1a) concludes that the findings of meta-analyses regarding surgical versus non-surgical treatment for acute achilles tendon rupture are inconsistent. The current best available evidence suggests that a functional rehabilitation is recommended after a non-surgical intervention. If functional rehabilitation can’t be provided by a rehabilitation centre, a surgical treatment may be preferred for the healing of an acute achilles tendon rupture. [2]
Physical Therapy Management (current best evidence)[edit | edit source]
On day 0, in the emergency department the diagnosis is made based on the following criteria :
1) a patient’s history with a clear sense of “snap” of the achilles tendon
2) a palpable defect, usually located 3–6 cm above the calcaneal tubercle
3) a positive calf squeeze test [7]. A plaster of Paris is applied to the patient’s foot in a
plantigrade position of 30–45 degrees. No weight bearing is allowed.
Week 0-6
Whether the tendon was treated surgically or non-surgically, the patient should wear a plaster cast for immobilization for at least 6 weeks on the injured ankle or a below-knee dorsal brace which allows the ankle to make a plantar flexion to start early mobilization in the first 6 weeks after injury or surgery as described in Groetelaers, René et al.(level of evidence 1b (prospective randomized trial))[3] . Lantto, Iikka, et al. level of evidence 1b (RCT) [1] .
Rehabilitation schedule and sample physiotherapy exercises [10]
In general physical therapy for an achilles tendon rupture starts immediately after the cast is removed and is mainly focused on firstly improving the range of motion (ROM) of the ankle. Later the physical therapy is focussed on increasing the muscle strength and muscle coordination [12]. A return to activities should be expected at 4-6 months of therapy. The rate of rehabilitation greatly depends on the quality of the treatment and the motivation of the patient [12].
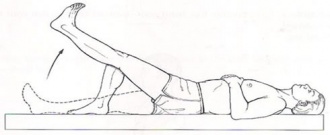
► At the start of the therapy until 6-8 weeks after surgery :
Start off with gentle passive mobilization of the ankle and the subtalar joints. Later go on to active ROM exercises. After two weeks of physiotherapy, progressive resistance exercises are added. Possible exercises for the patient are :
● Active flexion/extension of the ankle
● Ankle circles (clockwise and counterclockwise)
● Hip abduction
● Straight leg raise
● Standing hamstring curl
● Cycling on a stationary bicycle
► 8-12 weeks after surgery :
Ten weeks after the injury or surgery, gait training exercises can be started, followed by activity specific movements. The patient can start with a thera-band exercise program by starting from the lowest resistance and work up from there for regaining strength. The patient should also continue with the previous exercises.
● Ankle range of motion : plantar flexion and dorsiflexion to 90° : 2 x 8 repetitions
● Ankle range of motion : inversion and eversion
● Ankle range of motion : pronation and supination : 2 x 8 repetitions
● One leg standing balance exercise : 3 × 30 seconds [9][11]
● Standing heel-rise (2 × 3 seconds tempo) : 3 × 10 repetitions
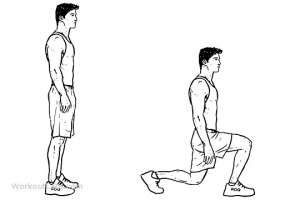
► 12-24 weeks after surgery :
The first set of exercises can now be executed with ankle weights. The following exercises can be added to the training program, but also basic exercises (described above) should still be executed :
● Calf stretch
● Toe raises
● Single leg balancing
● Walk on toes with support to start with (if needed) : 2 × 5 meters
● Standing heel-rise is performed with increased weight on injured leg :
5 × 10 repetitions
● Heel-rise in supine position with flexed legs
(with increased weight on injured leg) : 2 × 15 repetition
● Leg press with one leg at a time (10 repetitions maximum) : 2 × 10 repetitions
● Balance exercises on a trampoline : 2 × 45 seconds
● Walk/jog on a trampoline : 2 × 45 seconds
● Cross trainer : 1 min and 45 seconds
● The plank (core exercise) : 2 × 45 seconds
● Lunges (only with injured leg in front) : 2 × 10 repetitions
→ This program is performed as circle training.[9][11]
► Starting from week 14 until the end of the therapy
The patient is able to run approximately 14 weeks after the injury or surgery.
● Running on even ground is allowed when the patient can perform 5 single-legged heel-rises with approximately 90% of the height of the
uninjured leg. [9][11]
● Jogging upwards on stairs is allowed if the patient can walk 5 meters on their toes without the heel falling down.
The last step after surgery is eccentric exercise. During the eccentric part (lowering the heel), the patient has full weight on the injured foot, and during the concentric part (raising on tiptoe) only the non-injured foot is used [6].
• Patient takes places on a step, standing with full bodyweight on the forefoot of both feet, the knees are extended. Then he is asked to go
stand on his/her toes and to raise the non-injured leg so that his/her bodyweight is on his injured leg. Now the patient slowly lowers the
heel. In this way the calf muscle eccentrically guides the motion and is eccentrically trained.
• When the patient can perform this exercise without discomfort, he/she can increase the load by adding books or other weight to a
backpack, or to perform the exercise with a flexed knee.
When treated with an eccentric training program, the patient is more likely to be able to return faster to sport. The eccentric exercises should reduce pain and tendon thickness and should improve function of the tendon (and muscles). The eccentric calf-muscle exercises, as described below, should be executed twice daily for 12 weeks. The exercise program consists of 1-3sets of 15 repetitions per exercise, according to the improvement of the patient as described in . Murali K. Sayana, Maffulli N. et al, level of evidence 2b (individual cohort study) [6].
But not all patients benefit equally from an eccentric exercise program. It’s also proven that these exercises are less effective in sedentary people in comparison to athletes (Roos, M.E., et al., level of evidence 1b) [8].
► End of the therapy :
After completing the rehabilitation program, new examination of the tendon healing and functions is required. If needed, a new referral for further physiotherapy sessions can be provided to the patient. Gradual return to sports is recommended. For example before participating to contact sports, the patient should wait at least 6–9 months after the injury. (Nilsson-Helander K, et al. level of evidence 1b [9] Willits K, Et al.level of evidence 1b [11]).
Key Evidence[edit | edit source]
Links and reviews of high evidence can be added here.
Resources[edit | edit source]
• American Journal of Sports Medicine
• American Journal of Orthopedics
• Foot and Ankle International
• The Journal of Foot and Ankle Injury
• International Journey of Surgery
Clinical Bottom Line[edit | edit source]
An achilles Tendon Rupture also known as ATR is described as a typical sports-related pathology. We distinguish two sorts of ruptures: a complete rupture or a partial rupture. An ATR can be treated surgically or nonsurgically. Medical therapy consists of an operative repair by sewing the torn ends of the injured achilles tendon together. The physical rehabilitation changes from physical non-weight bearing exercises (at the beginning of the therapy) to more weightbearing exercises at the end of the revalidation.
Recent Related Research (from pubmed)[edit | edit source]
• Arverud E.D., et al., “Ageing, deep vein thrombosis and male gender predict poor outcome after acute achilles tendon rupture.” Bone Joint J.
2016 Dec;98-B(12):1635-1641.
• Gedam P.N., Rushnaiwala F.M. “Endoscopy-Assisted achilles Tendon Reconstruction With a Central Turndown Flap and Semitendinosus
Augmentation.” Foot Ankle Int. 2016 Dec;37(12):1333-1342. Epub 2016 Sep 20.
• Lantto, Iikka, et al. "A Prospective Randomized Trial Comparing Surgical and Nonsurgical Treatments of Acute achilles Tendon Ruptures."
The American journal of sports medicine 44.9 (2016): 2406.
→ level of evidence 1b
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Nicola Maffulli*1, Umile Giuseppe Longo2, Nikolaos Gougoulias1 and Vincenzo Denaro2. fckLRIpsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. 2008
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Flint, James H., et al. "Defining the Terms Acute and Chronic in Orthopaedic Sports Injuries. A Systematic Review." The fckLRAmerican journal of sports medicine42.1 (2014): 235-241.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 American college of foot and ankle surgeons/ foot health artikel. Achilles Tendon Rupture (2016 ) https://www.foothealthfacts.org/conditions/achilles-tendon-rupture
- ↑ 4.0 4.1 Vosseller JT, Ellis SJ, Levine DS, Kennedy JG, Elliott AJ, Deland JT, Roberts MM, O’Malley MJ. Achilles tendon rupture in women. Foot & ankle international. 2013 Jan;34(1):49-53.
- ↑ 5.0 5.1 5.2 5.3 Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States Population. Foot Ankle Int. 2013;34:475–480. doi: 10.1177/1071100713477621.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. Jul 1999;81(7):1019-36.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 Saglimbeni A, Fulmer C. Achilles tendon injuries and tendonitis. Medscape 2009 [accessed 2014 May 29]. fckLRhttp://emedicine.medscape.com/article/309393-overview
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Jacobs B, Lin D, Schwartz E. Achilles tendon rupture. Medscape 2009 [accessed 2014 May 29] fckLRhttp://emedicine.medscape.com/article/85024-overview
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 Gravlee J, Hatch R. Achilles tendon rupture: a challenging diagnosis. J Am Board Fam Med. 2000;13(5) fckLRhttp://www.medscape.com/viewarticle/405807
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 2016 Mar;23(10):34-6; quiz p 37. doi: 10.7748/en.23.10.34.s24. Achilles tendon rupture in atypical patient populations. fckLRKingsley P1. 1South East Coast Ambulance Service NHS Foundation Trust, Surrey
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 Berkson E. Achilles tendon rupture. Quincy medical center
- ↑ 12.0 12.1 12.2 12.3 AchillesTendon.com (2004-2016) : http://achillestendon.com/physiology/