Accessory Navicular Bone: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 8: | Line 8: | ||
Also known as '''Prehallux, Os Tibiale Externum and Navicular Secundum'''. | Also known as '''Prehallux, Os Tibiale Externum and Navicular Secundum'''. | ||
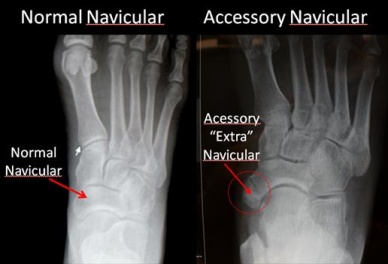
An accessory navicular bone is an accessory bone of the foot that occasionally develops abnormally causing a plantar medial enlargement of the navicular. The accessory navicular bone presents as a sesamoid in the posterior tibial tendon, in articulation with the navicular<ref name=" | An accessory navicular bone is an accessory bone of the foot that occasionally develops abnormally causing a plantar medial enlargement of the navicular. The accessory navicular bone presents as a sesamoid in the posterior tibial tendon, in articulation with the navicular<ref name="p1">Raymond T., Morrissy and Stuart L.Weinstein .Lovell, Winter’s Padiatric Orthopaedics. United States: Lippincot William’s Wilkin Publication, 2005.</ref> or as an enlargement of the navicular.<br> | ||
[[Image:Normal-Navicular-and-Accessory-Navicular.jpg|423x264px]]<br> | [[Image:Normal-Navicular-and-Accessory-Navicular.jpg|423x264px]]<br> | ||
| Line 38: | Line 38: | ||
<br> | <br> | ||
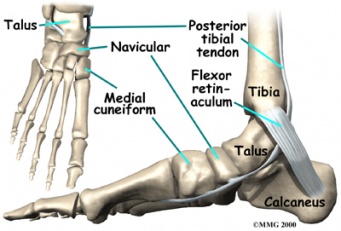
Navicular (boat shaped) is an intermediate tarsal bone on the medial side of the foot.<ref name=" | Navicular (boat shaped) is an intermediate tarsal bone on the medial side of the foot.<ref name="p3">D.Richard, V.Wayne, M. Adam,Gray’s Anatomy for Students. Spain: Elsevier Publishers, 2005</ref> It is located on the medial side of the foot, and articulates proximally with the talus. Distally it articulates with the three cuneiform bones. In some cases it articulates laterally with the cuboid. The tibialis posterior inserts to the os naviculare.<ref name="p4">Golano P., ‘The anatomy of the navicular and periarticular structures.’ Foot Ankle Clinics, 2004, March, vol. 9, p. 1-23.</ref> The tibialis posterior muscle also contracts to produce inversion of the foot and assists in the plantar flexion of the foot at the ankle. Tibialis posterior also has a major role in supporting the medial arch of the foot. <sup><ref name="p5">Kiter E., Erdan N., Karatosun V., Gunall I., ‘Tibialis posterior tendon abnormalities in feet with accessory navicular bone and flatfoot’. Acta orthopaedica Scandinavia, 1999, December, vol. 70, p. 618-621</ref> </sup>This supports is compromised by abnormal insertion of the tendon into the accessory navicular bone when present. <ref name="p6">Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999</ref> <ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref>This lead to loss of suspension of tibialis posterior tendon and may cause peroneal spastic pes planus or simple pes planus. But, yet a cause and effect relationship between the accessory navicular and pes planus is doubtful and is yet unproved clearly.<ref name="p8">Kidner FC. Pre-hallux in relation to flatfoot. JAMA 1933; 101: 1539-42.</ref><br> | ||
The presence of accessory navicular 2 or 3 is also a cause of PTT tendinopathy as the insertion of PTT on accessory navicular leads to its proximal insertion (dashed line). Here by the leverage of malleolus on the PTT is reduced and therefore stress on the tendon increase. <ref name=" | The presence of accessory navicular 2 or 3 is also a cause of PTT tendinopathy as the insertion of PTT on accessory navicular leads to its proximal insertion (dashed line). Here by the leverage of malleolus on the PTT is reduced and therefore stress on the tendon increase. <ref name="p9">A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1 Accessory navicular bone: Not Such a normal variant. JBR–BTR, 2004, 87 (5) page 250-252</ref><br><br> | ||
[[Image:ANGLE CHANGE IN AN.PNG]]<br> | [[Image:ANGLE CHANGE IN AN.PNG]]<br> | ||
| Line 46: | Line 46: | ||
<br> | <br> | ||
There also occurs calcaneal pitch angle lowering in patients with with symptomatic accessory navicular than in normal subjects.<ref name=" | There also occurs calcaneal pitch angle lowering in patients with with symptomatic accessory navicular than in normal subjects.<ref name="p0">Prichausuk S, Sinphurmsukskul O: Kinder Procedure for symptomatic accessory navicular and its relation to pes planus, Foot Ankle 16:500,1995</ref><br> | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
The foot and ankle have numerous accessory ossification centres. But the most common is accessory tarsal navicular bone occurring between 4-14% of population. <ref name=" | The foot and ankle have numerous accessory ossification centres. But the most common is accessory tarsal navicular bone occurring between 4-14% of population. <ref name="p1">Harris RI. Army foot survey: an investigation of foot ailments in Canadian soldiers. National Research Council of Canada, 1947</ref><ref name="p2">Shands AR Jr, Wentz IJ. Congenital anomalies, accessory bones and osteochondritis in the feet of 850 children. Surg.Clin.North Am 1953:97:1643-1666</ref><ref name="p3">Geist ES. The accessory scaphoid bone. J Bone Joint Surg Am 1925; 7:570</ref> <br> | ||
*an accessory navicular bone is present in ~10% of the population | *an accessory navicular bone is present in ~10% of the population | ||
*first appears in adolescence. In children its incidence is 4-21% of the population.<ref name=" | *first appears in adolescence. In children its incidence is 4-21% of the population.<ref name="p9">A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1 Accessory navicular bone: Not Such a normal variant. JBR–BTR, 2004, 87 (5) page 250-252</ref> | ||
*more common in female patients<ref name=" | *more common in female patients<ref name="p1">Raymond T., Morrissy and Stuart L.Weinstein .Lovell & Winter’s Padiatric Orthopaedics. United States: Lippincot William’s & Wilkin Publication, 2005.</ref> | ||
*reported prevalence of bilaterality is ~70% (range 50-90%)<br> | *reported prevalence of bilaterality is ~70% (range 50-90%)<br> | ||
| Line 81: | Line 81: | ||
*Stress fracture | *Stress fracture | ||
*Tendinitis | *Tendinitis | ||
*Medial tuberosity fracture <ref name=" | *Medial tuberosity fracture <ref name="p5">Jamshid Tehranzadeh; Musculoskeletal Imaging; page 680; Ed.2009</ref> | ||
*Cartilage forming bone Tumor | *Cartilage forming bone Tumor | ||
*Kohler’s disease <ref name=" | *Kohler’s disease <ref name="p6">Helen Carty, Donald Shaw, Francis Brunelle, Brain Kendall; Imaging in Children; Churchill Livingston publication. Vol.2; pg no.866.</ref><br> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 101: | Line 101: | ||
== Examination == | == Examination == | ||
Patient with accessory navicular may present with complex pain patterns requiring thorough examination. <ref name=" | Patient with accessory navicular may present with complex pain patterns requiring thorough examination. <ref name="p7">Ray S, Goldberg VM. Surgical treatment of the accessory navicular. Clin. Orthop 1983;177: 61-66.</ref> The examination importantly includes | ||
*Differentiation of navicular prominence from talar head prominence in flat foot deformity by inverting and everting through the subtalar joint with a thumb over the bony prominence.<ref name=" | *Differentiation of navicular prominence from talar head prominence in flat foot deformity by inverting and everting through the subtalar joint with a thumb over the bony prominence.<ref name="p8">Sullivan JA, Miller WA. The relationship of the accessory navicular to the development of the flat foot. ClinOrthop 1979; 144: 233-237.</ref> | ||
*Recognition of the loss of structural integrity of the longitudinal arch is important because this component of the deformity will not be corrected by surgical treatment if required. <ref name=" | *Recognition of the loss of structural integrity of the longitudinal arch is important because this component of the deformity will not be corrected by surgical treatment if required. <ref name="p9">S.TerryCanale, James S. Beaty,Campbell Operative Orthopaedics. United States: Mosby Publication.2008</ref> | ||
*Thought examination of gait.<br> | *Thought examination of gait.<br> | ||
| Line 112: | Line 112: | ||
# Physical therapy | # Physical therapy | ||
#Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed. In some cases, oral or injected steroid medications may be used in combination with immobilization to reduce pain and inflammation. <ref name=" | #Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed. In some cases, oral or injected steroid medications may be used in combination with immobilization to reduce pain and inflammation. <ref name="p9">Macnicol M. F., Voutsinass, ‘Surgical treatment of the symptomatic accessory navicular’, The Journal of Bone and Joint Surgery, 1984, vol. 66, p. 218-226.</ref> | ||
'''SURGICAL:''' Depending upon the severity the non operative or conservative treatment should be maintained for at least 4- 6 months before any surgical intervention. | '''SURGICAL:''' Depending upon the severity the non operative or conservative treatment should be maintained for at least 4- 6 months before any surgical intervention. | ||
| Line 118: | Line 118: | ||
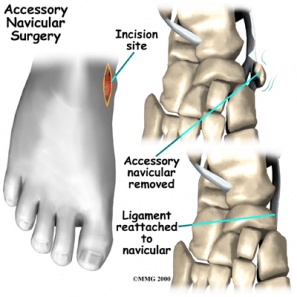
There are 2 surgeries that can be performed depending upon the condition and symptoms | There are 2 surgeries that can be performed depending upon the condition and symptoms | ||
'''FIRST''' is simple surgical excision. In this generally the accessory navicular along with its prominence is removed. In this procedure, skin incision is made dorsally to the prominence of accessory navicular. Bone is removed to the point where the medial foot has no bony prominence over the navicular, between the head of the talus and first cuneiform. Symptoms are relieved in 90% of cases.<ref>Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999.&lt;/ref&gt;&lt;ref name=" | '''FIRST''' is simple surgical excision. In this generally the accessory navicular along with its prominence is removed. In this procedure, skin incision is made dorsally to the prominence of accessory navicular. Bone is removed to the point where the medial foot has no bony prominence over the navicular, between the head of the talus and first cuneiform. Symptoms are relieved in 90% of cases.<ref>Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999.&lt;/ref&gt;&lt;ref name="p7"&gt;Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref> | ||
[[Image:Accessory navicular surgery.jpg|364x297px]]<br> | [[Image:Accessory navicular surgery.jpg|364x297px]]<br> | ||
'''SECOND''' is Kindler procedure.<ref name=" | '''SECOND''' is Kindler procedure.<ref name="p6">Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999</ref><ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref> In this the ossicle and navicular prominence is excised as in simple excision but along with the posterior tibial tendon advancement. Posterior tibial tendon is split and advanced along the medial side of foot to provide support to longitudinal arch.<br> | ||
After surgery 4 week short leg cast, well moulded into the arch with the foot plantigrade is applied. Partial weight bearing till the 8th week and later full weight bearing is allowed.<ref name=" | After surgery 4 week short leg cast, well moulded into the arch with the foot plantigrade is applied. Partial weight bearing till the 8th week and later full weight bearing is allowed.<ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref><ref name="p9">S.Terry Canale, James S. Beaty,Campbell Operative Orthopaedics. United States: Mosby Publication.2008.</ref>. When the cast is being removed can start building up the ROM to counter atrophy and other physical therapy treatment which include stretching and strengthening exercises. <ref name="p8">Leonard Z. C., Fortin P. T., ‘Adolescent accessory navicular bone’ Foot Ankle Clinics, 2010, vol. 15, p. 337-347.</ref><br> | ||
[[Image:CAST MOULDING.jpg|297x274px]] [[Image:SHORT LEG CAST.jpg|347x261px]]<br> | [[Image:CAST MOULDING.jpg|297x274px]] [[Image:SHORT LEG CAST.jpg|347x261px]]<br> | ||
| Line 132: | Line 132: | ||
Occasionally, a limited fusion of the cuneiform metatarsal or talonavicular joints also was recommended. The rationale and efficacy of this operation have been questioned. | Occasionally, a limited fusion of the cuneiform metatarsal or talonavicular joints also was recommended. The rationale and efficacy of this operation have been questioned. | ||
Arthrodesis may be a reasonable treatment option in selected cases of patients with symptomatic recalcitrant Type II accessory naviculars that are large enough to accept small fragment screws.<ref name=" | Arthrodesis may be a reasonable treatment option in selected cases of patients with symptomatic recalcitrant Type II accessory naviculars that are large enough to accept small fragment screws.<ref name="p1">Scott AT.,Sabesan VJ, Saluta JR, Wilson MA, Easley ME.Fusion versus excision of the symptomatic Type II accessory navicular: a prospective study.Foot Ankle Int. 2009 Jan;30(1):10-5</ref><br> | ||
== Physical Therapy Management == | == Physical Therapy Management == | ||
| Line 142: | Line 142: | ||
*Well padded shoe orthotic should be worn for arch support. This decrease direct pressure over the navicular. | *Well padded shoe orthotic should be worn for arch support. This decrease direct pressure over the navicular. | ||
*Stretching of peroneal and posterior tibialis along with strengthening exercises. | *Stretching of peroneal and posterior tibialis along with strengthening exercises. | ||
*Strengthening the intrinsic foot muscles and lateral thigh rotators muscles and decrease inflammation.<ref name=" | *Strengthening the intrinsic foot muscles and lateral thigh rotators muscles and decrease inflammation.<ref name="p9">A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1Accessory navicular bone: Not Such a normal variant.JBR–BTR, 2004, 87 (5) page 250-252</ref> | ||
*Activity modification, such as limiting or stopping any strenuous activities that cause the Accessory Navicular bone to become symptomatic can be used for initial treatment.<ref name=" | *Activity modification, such as limiting or stopping any strenuous activities that cause the Accessory Navicular bone to become symptomatic can be used for initial treatment.<ref name="p9">A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel. Accessory navicular bone: Not Such a normal variant.JBR–BTR, 2004, 87 (5) page 250-252</ref> | ||
*Gait training and Balance exercise for proper normal gait when required.<br><br> | *Gait training and Balance exercise for proper normal gait when required.<br><br> | ||
| Line 167: | Line 167: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Usually the type I accessory navicular is rarely associated with symptoms and if the symptoms appears then it respond well to the conservative/ physical therapy management. Patients with Type II accessory navicular are at the risk for disruption either from traction injury or shear forces in the region and and mostly the onset is insidious or post trauma. It fails to respond to conservative treatment when severe and fusion of the accessory navicular to the navicular may successfully relieve pain without disrupting the tibialis posterior tendon insertion.<ref name=" | Usually the type I accessory navicular is rarely associated with symptoms and if the symptoms appears then it respond well to the conservative/ physical therapy management. Patients with Type II accessory navicular are at the risk for disruption either from traction injury or shear forces in the region and and mostly the onset is insidious or post trauma. It fails to respond to conservative treatment when severe and fusion of the accessory navicular to the navicular may successfully relieve pain without disrupting the tibialis posterior tendon insertion.<ref name="p2">Chung JW, Chu IT.,Outcome of fusion of a painful accessory navicular to the primary navicular. Foot Ankle Int. 2009 Feb;30(2):106-9.</ref><br> | ||
Type III when symptomatic then excising the accessory navicular rather than excising navicular beak is more helpful.<ref name=" | Type III when symptomatic then excising the accessory navicular rather than excising navicular beak is more helpful.<ref name="p9">S.TerryCanale, James S. Beaty,Campbell Operative Orthopaedics. United States: Mosby Publication.2008.</ref> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
Revision as of 12:42, 6 June 2017
Original Editors - Carlos De Coster
Top Contributors - Aarti Sareen, Admin, Carlos De Coster, Scott Cornish, Kim Jackson, Laura Ritchie, WikiSysop, Lucinda hampton, 127.0.0.1, Evan Thomas, Tony Lowe and Oyemi Sillo
Definition/Description[edit | edit source]
Also known as Prehallux, Os Tibiale Externum and Navicular Secundum.
An accessory navicular bone is an accessory bone of the foot that occasionally develops abnormally causing a plantar medial enlargement of the navicular. The accessory navicular bone presents as a sesamoid in the posterior tibial tendon, in articulation with the navicular[1] or as an enlargement of the navicular.
The Geist classification divides these into three types:
Type I: is sesamoid bone in the posterior tibialis tendon. There is a small distance (<3mm) between the sesamoid and the navicular.
File:Type I AN dia.PNG File:TYPE I AN X RAY.jpg
Type II: consists of an accessory bone, upto 1.2cm in diameter, in which a synchondrosis exist between it and the navicular.
File:Type II AN.PNG File:TypeIIAccessoryNavicular.jpg
Type III: is the fused accessory navicular to the navicular resulting in large cornuate navicular.
File:TYPE III AN.PNG File:TYPE III ACCESSORY N. X RAY.PNG
Clinically Relevant Anatomy[edit | edit source]
 File:Foot accessory navicular clinical antomy 2.jpg
File:Foot accessory navicular clinical antomy 2.jpg
Navicular (boat shaped) is an intermediate tarsal bone on the medial side of the foot.[2] It is located on the medial side of the foot, and articulates proximally with the talus. Distally it articulates with the three cuneiform bones. In some cases it articulates laterally with the cuboid. The tibialis posterior inserts to the os naviculare.[3] The tibialis posterior muscle also contracts to produce inversion of the foot and assists in the plantar flexion of the foot at the ankle. Tibialis posterior also has a major role in supporting the medial arch of the foot. [4] This supports is compromised by abnormal insertion of the tendon into the accessory navicular bone when present. [5] [6]This lead to loss of suspension of tibialis posterior tendon and may cause peroneal spastic pes planus or simple pes planus. But, yet a cause and effect relationship between the accessory navicular and pes planus is doubtful and is yet unproved clearly.[7]
The presence of accessory navicular 2 or 3 is also a cause of PTT tendinopathy as the insertion of PTT on accessory navicular leads to its proximal insertion (dashed line). Here by the leverage of malleolus on the PTT is reduced and therefore stress on the tendon increase. [8]
There also occurs calcaneal pitch angle lowering in patients with with symptomatic accessory navicular than in normal subjects.[9]
Epidemiology /Etiology[edit | edit source]
The foot and ankle have numerous accessory ossification centres. But the most common is accessory tarsal navicular bone occurring between 4-14% of population. [1][10][2]
- an accessory navicular bone is present in ~10% of the population
- first appears in adolescence. In children its incidence is 4-21% of the population.[8]
- more common in female patients[1]
- reported prevalence of bilaterality is ~70% (range 50-90%)
People who have an accessory navicular often are unaware of the condition if it causes no problems. However, some people with this extra bone develop a painful condition known as accessory navicular syndrome when the bone and/or posterior tibial tendon are aggravated. This can result from any of the following:
- Trauma, as in a foot or ankle sprain
- Chronic irritation from shoes or other footwear rubbing against the extra bone
- Excessive activity or overuse
Characteristics/Clinical Presentation[edit | edit source]
- Typical young female (10-20 years of age) complaining of mid food/arch pain which may be insidious or post trauma
- Difficulty with footwear
- Prominent navicular
- Tenderness over the prominence
- Pain over the posterior tibialis tendon from a tendinitis and tightness of the tendo-achillis in long standing cases
- Often pes planus
- Inflamed bursa
Differential Diagnosis[edit | edit source]
- Stress fracture
- Tendinitis
- Medial tuberosity fracture [4]
- Cartilage forming bone Tumor
- Kohler’s disease [5]
Diagnostic Procedures[edit | edit source]
- Routine standing AP and lateral view are enough to look for accessory navicular but in some cases oblique view is also obtained in order to completely define the abnormality of navicular. Bilateral films may be indicated as there occurs high incidence of symmetrical abnormalities.
- On lateral weight bearing/standing film, the talonavicular cuneiform first metatarsal dorsal alignment should be carefully examined. “Sag” at this joint indicates structural integrity of the area.
- MRI or CT is indicated (very rare) in order to exclude tumor, fracture of medial tuberosity, bone marrow edema.
AP Veiw' Lateral Veiw 'Oblique Veiw
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
Patient with accessory navicular may present with complex pain patterns requiring thorough examination. [6] The examination importantly includes
- Differentiation of navicular prominence from talar head prominence in flat foot deformity by inverting and everting through the subtalar joint with a thumb over the bony prominence.[7]
- Recognition of the loss of structural integrity of the longitudinal arch is important because this component of the deformity will not be corrected by surgical treatment if required. [8]
- Thought examination of gait.
Medical Management[edit | edit source]
CONSERVATIVE:
- Physical therapy
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed. In some cases, oral or injected steroid medications may be used in combination with immobilization to reduce pain and inflammation. [8]
SURGICAL: Depending upon the severity the non operative or conservative treatment should be maintained for at least 4- 6 months before any surgical intervention.
There are 2 surgeries that can be performed depending upon the condition and symptoms
FIRST is simple surgical excision. In this generally the accessory navicular along with its prominence is removed. In this procedure, skin incision is made dorsally to the prominence of accessory navicular. Bone is removed to the point where the medial foot has no bony prominence over the navicular, between the head of the talus and first cuneiform. Symptoms are relieved in 90% of cases.[11]
SECOND is Kindler procedure.[5][6] In this the ossicle and navicular prominence is excised as in simple excision but along with the posterior tibial tendon advancement. Posterior tibial tendon is split and advanced along the medial side of foot to provide support to longitudinal arch.
After surgery 4 week short leg cast, well moulded into the arch with the foot plantigrade is applied. Partial weight bearing till the 8th week and later full weight bearing is allowed.[6][8]. When the cast is being removed can start building up the ROM to counter atrophy and other physical therapy treatment which include stretching and strengthening exercises. [7]
File:CAST MOULDING.jpg File:SHORT LEG CAST.jpg
Occasionally, a limited fusion of the cuneiform metatarsal or talonavicular joints also was recommended. The rationale and efficacy of this operation have been questioned.
Arthrodesis may be a reasonable treatment option in selected cases of patients with symptomatic recalcitrant Type II accessory naviculars that are large enough to accept small fragment screws.[1]
Physical Therapy Management[edit | edit source]
If the accessory navicular bone becomes problematic physical therapy may be prescribed.
This will include use of therapeutic modalities which relieves pain include ultrasonic therapy, TENS, massage, ROM exercises and treatments to strengthen the intrinsic foot muscles and lateral thigh rotators muscles and decrease inflammation. Often is the accessory navicular bone linked to Posterior tibial dysfunction to a pes planus. To adjust the arch of the foot, orthotic devices may be used.
- Well padded shoe orthotic should be worn for arch support. This decrease direct pressure over the navicular.
- Stretching of peroneal and posterior tibialis along with strengthening exercises.
- Strengthening the intrinsic foot muscles and lateral thigh rotators muscles and decrease inflammation.[8]
- Activity modification, such as limiting or stopping any strenuous activities that cause the Accessory Navicular bone to become symptomatic can be used for initial treatment.[8]
- Gait training and Balance exercise for proper normal gait when required.
Some examples of basic and functional posterior tibialis strengthening:
| [12] | [13] |
| [14] | [15] |
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
Usually the type I accessory navicular is rarely associated with symptoms and if the symptoms appears then it respond well to the conservative/ physical therapy management. Patients with Type II accessory navicular are at the risk for disruption either from traction injury or shear forces in the region and and mostly the onset is insidious or post trauma. It fails to respond to conservative treatment when severe and fusion of the accessory navicular to the navicular may successfully relieve pain without disrupting the tibialis posterior tendon insertion.[10]
Type III when symptomatic then excising the accessory navicular rather than excising navicular beak is more helpful.[8]
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-y-ZWVYINKeHZi7bpsugXOuniIrzEOQffwjhNAPouwaB4tkT_: Error parsing XML for RSS
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area. |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Raymond T., Morrissy and Stuart L.Weinstein .Lovell, Winter’s Padiatric Orthopaedics. United States: Lippincot William’s Wilkin Publication, 2005. Cite error: Invalid
<ref>tag; name "p1" defined multiple times with different content Cite error: Invalid<ref>tag; name "p1" defined multiple times with different content Cite error: Invalid<ref>tag; name "p1" defined multiple times with different content - ↑ 2.0 2.1 D.Richard, V.Wayne, M. Adam,Gray’s Anatomy for Students. Spain: Elsevier Publishers, 2005 Cite error: Invalid
<ref>tag; name "p3" defined multiple times with different content - ↑ Golano P., ‘The anatomy of the navicular and periarticular structures.’ Foot Ankle Clinics, 2004, March, vol. 9, p. 1-23.
- ↑ 4.0 4.1 Kiter E., Erdan N., Karatosun V., Gunall I., ‘Tibialis posterior tendon abnormalities in feet with accessory navicular bone and flatfoot’. Acta orthopaedica Scandinavia, 1999, December, vol. 70, p. 618-621 Cite error: Invalid
<ref>tag; name "p5" defined multiple times with different content - ↑ 5.0 5.1 5.2 Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999 Cite error: Invalid
<ref>tag; name "p6" defined multiple times with different content Cite error: Invalid<ref>tag; name "p6" defined multiple times with different content - ↑ 6.0 6.1 6.2 6.3 Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831 Cite error: Invalid
<ref>tag; name "p7" defined multiple times with different content Cite error: Invalid<ref>tag; name "p7" defined multiple times with different content Cite error: Invalid<ref>tag; name "p7" defined multiple times with different content - ↑ 7.0 7.1 7.2 Kidner FC. Pre-hallux in relation to flatfoot. JAMA 1933; 101: 1539-42. Cite error: Invalid
<ref>tag; name "p8" defined multiple times with different content Cite error: Invalid<ref>tag; name "p8" defined multiple times with different content - ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1 Accessory navicular bone: Not Such a normal variant. JBR–BTR, 2004, 87 (5) page 250-252 Cite error: Invalid
<ref>tag; name "p9" defined multiple times with different content Cite error: Invalid<ref>tag; name "p9" defined multiple times with different content Cite error: Invalid<ref>tag; name "p9" defined multiple times with different content Cite error: Invalid<ref>tag; name "p9" defined multiple times with different content Cite error: Invalid<ref>tag; name "p9" defined multiple times with different content Cite error: Invalid<ref>tag; name "p9" defined multiple times with different content - ↑ Prichausuk S, Sinphurmsukskul O: Kinder Procedure for symptomatic accessory navicular and its relation to pes planus, Foot Ankle 16:500,1995
- ↑ 10.0 10.1 Shands AR Jr, Wentz IJ. Congenital anomalies, accessory bones and osteochondritis in the feet of 850 children. Surg.Clin.North Am 1953:97:1643-1666 Cite error: Invalid
<ref>tag; name "p2" defined multiple times with different content - ↑ Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999.</ref><ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831
- ↑ ShaychiITA. Tibialis Posterior Basic Strengthening. Available from: http://www.youtube.com/watch?v=zmh1FisBeeM [last accessed 24/11/12]
- ↑ ShaychiITA. Tibialis Posterior Basic Multiplanar Strengthening. Available from: http://www.youtube.com/watch?v=qv76eBxGQXI [last accessed 01/12/12]
- ↑ ShaychiITA. Tibialis Posterior Functional Strengthening: Full Body Weight Maintaining Supination. Available from: http://www.youtube.com/watch?v=1C_C5N9reB8[last accessed 01/12/12]|}
- ↑ ShaychiITA. Tibialis Posterior Functional Strengthening: Maintain Arch with Compass Squats. Available from: http://www.youtube.com/watch?v=TdHgyFZbOPk[last accessed 24/11/12]|}