Myasthenia Gravis
Originating Editor: Wendy Walker
Definition[edit | edit source]
Myasthenia Gravis is a relatively rare anautoimmune neuromuscular disease leading to fluctuating muscle weakness and fatigue. Muscle weakness is caused by circulating antibodies that block acetylcholine receptors at the postsynaptic neuromuscular junction,inhibiting the excitatory effects of the neurotransmitter acetylcholine on nicotinic receptors at neuromuscular junctions.[1]
Clinically Relevant Anatomy
[edit | edit source]
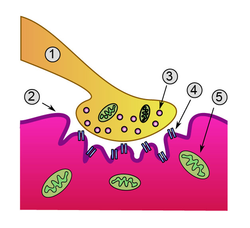 This is a detailed view of a neeuromuscular junction.
This is a detailed view of a neeuromuscular junction.
1. Presynaptic terminal
2. Sarcolemma
3. Synaptic vesicle
4. Nicotinic acetylcholine receptor
5. Mitochondrion
Mechanism of Injury / Pathological Process
[edit | edit source]
In Myasthenia gravis (MG) antibodies form against nicotinic acetylcholine (ACh) postsynaptic receptors at the neuromuscular junction (NMJ) of the skeletal muscles[2].The basic pathology is a reduction in the number of ACh receptors (AChRs) at the postsynaptic muscle membrane brought about by an acquired autoimmune reaction producing anti-AChR antibodies[3].
Clinical Presentation[edit | edit source]
The usual initial complaint is a specific muscle weakness rather than generalized weakness - frequently ocular (eye) symptoms.
Extraocular muscle weakness or ptosis is present initially in 50% of patients, and occurs during the course of illness in 90% of patients.
The disease remains exclusively ocular in only 16% of patients.
Rarely, patients have generalized weakness without ocular muscle weakness.
Bulbar muscle weakness is also common, along with weakness of head extension and flexion.
Limb weakness may be more severe proximally than distally.
Isolated limb muscle weakness is the presenting symptom in fewer than 10% of patients.
Weakness is typically least severe in the morning and worsens as the day progresses.
Weakness is increased by exertion and alleviated by rest.
Weakness progresses from mild to more severe over weeks or months, with exacerbations and remissions.
Weakness tends to spread from the ocular to facial to bulbar muscles and then to truncal and limb muscles.
About 87% of patients have generalized disease within 13 months after onset.
Less often, symptoms may remain limited to the extraocular and eyelid muscles for many years.
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ http://en.m.wikipedia.org/wiki/Myasthenia_gravis
- ↑ Strauss AJL, Seigal BC, Hsu KC. Immunofluorescence demonstration of a muscle binding complement fixing serum globulin fraction in Myasthenia Gravis. Proc Soc Exp Biol. 1960;105:184
- ↑ Patric J, Lindstrom JM. Autoimmune response to acetylcholine receptor. Science. 1973;180:871






