Shoulder Bursitis
Original Editor - Willem Vanderpooten
Top Contributors - Matthias Proost, Dries Meeusen, Lucinda hampton, Vanderpooten Willem, Mariam Hashem, Fasuba Ayobami, Rachael Lowe, Naomi O'Reilly, Kim Jackson, Admin, Wanda van Niekerk, Venus Pagare, Claire Knott and Bouzarpour Faryân
Introduction[edit | edit source]
Shoulder bursae refers to sacs surrounding the shoulder joint that are filled with synovial fluid. As with bursae in general, they facilitate movement and reduce friction at tendon-tendon and tendon-bone interfaces. Shoulder bursitis (inflammation of a bursa) is one of the leading causes of shoulder pain. It can lead to lost workdays and, in some cases, even disability.
The symptoms of bursitis vary by type and severity, but may include swelling, excessive warmth at the site, tenderness, pain and/or fever.
Depending on the type of shoulder bursitis, treatment may include activity modification, immobilization with a splint, icing, injections, aspiration of the bursa (removing fluid with a syringe), antibiotics or anti-inflammatory pain medication.[1][2]
Clinically Relevant Anatomy[edit | edit source]
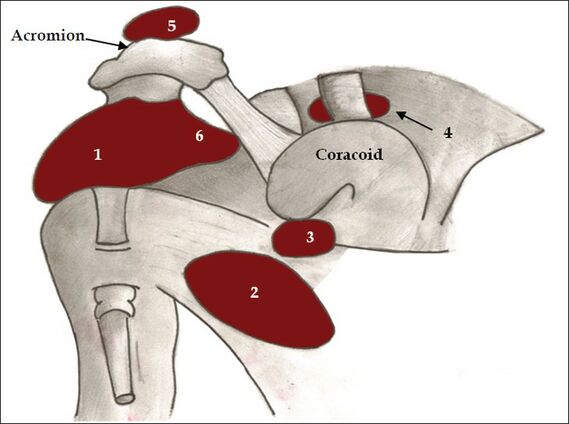
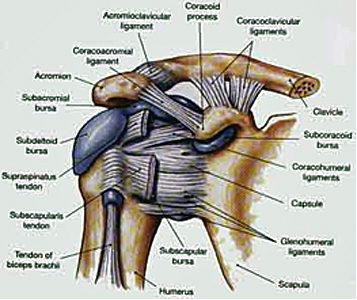
There are five main bursae around the shoulder. They include:
- Subacromial-subdeltoid (SASD) bursa
- Subscapular recess
- Subcoracoid bursa
- Coracoclavicular bursa
- Supra-acromial bursa
Sometimes authors include a 6th bursal space which is the
6. Medial extension of subacromial-subdeltoid bursa[1]
Nerve Supply: There is a nerve supply to bursa. eg The Subacromial Bursae has Suprascapular and Axillary nerve endings with nociceptors such as free nerve endings giving information about painful stimulation and inflammatory responses to the brain[3]. Also mechanoreceptors in the bursae of the shoulder are capable of giving proprioceptive information of shoulder joint position.[4] This shows that bursae don’t strictly function as a lubricator between tissues.
Etiology[edit | edit source]
There are several ways to develop bursitis, but the condition is usually caused by too much stress on the bursa. In general, however, bursal irritation can be roughly divided into three groups.
- Chronic bursitis: most common and develops over time due to repetitive irritation of the bursa. At risk people include those who have gout, pseudogout, diabetes, rheumatoid arthritis, uremia, and other conditions.
- Infected bursitis: in this type, the bursa becomes infected with bacteria. If the infection spreads, it can cause serious problems.
- Traumatic bursitis (or acute traumatic bursitis): Due to an accident, the bursa could become irritated and inflamed[2].
Characteristics / Clinical Presentation[edit | edit source]
Bursitis is typically identified by localized pain or swelling, tenderness, and pain with motion of the tissues in the affected area. Bursitis of the shoulder presentations include:
- Younger and middle-aged patients are much more likely to experience acute bursitis than older patients with chronic rotator cuff syndrome.[5]
- Shoulder bursitis is often accompanied by tendinitis of tendons adjacent to the affected bursa in the shoulder.
- Subacromial Bursitis typically presents with lateral or anterior shoulder pain. Overhead lifting or reaching activities become uncomfortable, and the pain is often worse at night; interrupting sleep.
- Activities of daily living, household tasks and hygiene may be affected, due to limited and painful overhead movements.
- May have interrupted sleep patterns. Rolling over the affected shoulder during sleeping can cause pressure on the inflamed bursa increasing the pain..[6][7]
- Activities like contact sports are difficult to perform because may cause pain.
See also Subacromial Pain Syndrome
Treatment[edit | edit source]
The treatment depends on the type of bursitis.
- Chronic bursitis is treated by a reduction in the activities that cause swelling. In addition use of anti-inflammatory medications (i.e., ibuprofen, Naprosyn, Celebrex, etc.) for a few weeks as well as icing two or three times per day for 20 to 30 minutes each time until the swelling is gone. Heat should not be used since it will increase the inflammation. Injection of steroids into the bursa may decrease the swelling and inflammation but can be associated with unwanted side effects (infection, skin atrophy, chronic pain). Injection of cortisone is best reserved for those bursae that do not get better with the treatment above. In addition, any bursa that might be infected should not be injected with cortisone.
- Infected bursitis requires immediate evaluation by the doctor. Aspirating the bursa may an option to reduce its size and for biopsy. Antibiotics are needed to kill bacteria. The true danger with this type of bursitis is the risk that bacteria can spread to the blood. As with the other types of bursal inflammation, ice, rest, and anti-inflammatory medications improve swelling and inflammation.
- Traumatic bursitis is normally treated by aspirating the bursa (i.e., using a small needle to draw fluid/blood from the affected bursa). Icing and NSAIDs (anti-inflammatory medications) help to reduce swelling[2].
Physical therapy can be used to aid the recovery from bursitis, especially when it is accompanied by a frozen shoulder. See Physiotherapy treatment section.
Differential Diagnosis[edit | edit source]
Bursitis is frequently caused by another medical condition. For example, patients who suffer from subacromial bursitis, are likely to suffer from adhesive capsulitis, rotator cuff tendinopathy, Supraspinatus Tendinopathy or bicipital tendinopathy.[7]
Other conditions include:
- Supraspinatus Tendinopathy: "Empty Can" test. The patient abducts the arms to 90 degrees with the elbows extended and the arms internally rotated. The arms are placed 30 degrees anteriorly (in the coronal plane), and the patient resists as the examiner forces the arms downward.
- Frozen shoulder[8]
Acromioclaviculair syndrome: patient presents with horizontal abduction restriction. In addition to pain in the area of the acromioclavicular joint and/or C4 dermatome.
Diagnostic Procedures[edit | edit source]
Bursitis is typically identified by localized pain and/or swelling, tenderness, and pain with motion of the tissues in the affected area. X-ray testing can sometime detect calcification in the bursa when bursitis has been chronic or recurrent, with bursa fluid puncture is it possible to rule out infections.. While MRI scanning can be used to identify bursitis, but it is uncommonly used for the diagnosis[9]
The Subacromial Deltoid bursa comes into conflict with the Acromioclavicular joint dysfunction. Positive painful arc ( pain between 60 and 120 degrees of abduction) indicates Subacromial Deltoid Bursitis.
- To test the painful arc, patient stands up with arms alongside the body. then actively abduct the shoulder from 0° to 180°. Test is positive when the patient complains of pain between 60°-120° abduction. The pain results from compression of the Supraspinatus tendon and the Subacromial Bursa in the subacromial space which becomes narrower at this range. Beyond 120° the pressure on the bursa decreases and the pain is lessened. [10][11]
The Subcoracoid Bursa stands in relation with the anterior joint capsule. We speak of a Subcoracoid Bursa when the passive external rotation in 90 degrees of abduction is negative and the passive external rotation on 0 degrees is positive.
A test for the Scapulothoracic Bursa focuses on the strength of the scapular muscles—including the Trapezius (upper, middle, and lower), Levator Scapula, Serratus Anterior, Latissimus Dorsi, Deltoids and Rotator Cuff muscles. A loss of muscle tone or an alteration of scapulothoracic rhythm may lead to increased friction between the medial border of the scapula and the rib cage, resulting in crepitus or snapping.
Snapping scapula is a painful crepitus of the scapulothoracic articulation. This crepitus is a grinding or snapping noise with scapulothoracic motion that may or may not accompany pain. This condition is commonly seen in overhead-throwing athletes. Treatment of patients with this syndrome begins with nonoperative methods; when nonoperative treatment fails, several surgical options exist.[12][13]
Shoulder bursitis commonly co-exists with different shoulder pathologies (see differential diagnosis), which can make it hard to diagnose. Torn tendons or ligaments can cause as well the irritated bursa.
Shoulder bursitis can be caused due a repeated minor trauma. This can be an overuse of the shoulder joint and muscles according to a more single significant trauma such as a fall for example.[14]
Physical Examination[edit | edit source]
Bursitis can often be diagnosed by clinical examination; by visual inspection it is possible to notice some redness and warmth, local tenderness or stiffness in the joint with some swelling when the inflammation is worse.
Physical examination of the subacromial bursitis reveals a reduced active range of motion with decreased elevation, internal rotation and abduction, primarily because of pain. The most painful arc of motion is between 70 and 120 degrees of abduction. Tenderness is found laterally below the acromion, anteriorly at the insertion of the Supraspinatus tendon on the greater tuberosity and, occasionally, along the supraspinatus muscle belly beneath the trapezius.
Strength testing may reveal weakness with internal and external rotation, a finding that demonstrates an important factor in the etiology of these injuries: functional instability due to rotator cuff weakness.
The impingement signs are usually positive. The Neer's sign is performed by forcibly forward flexing the internally rotated arm maximally above 90 degrees. The Hawkin's impingement sign refers to forced internal rotation of the arm performed during forward elevation to 90 degrees. Both tests are considered positive if they produce pain.[15]
The Compression test can also be used. This test is positive if the patient experiences subacromial pain. It may also indicate Supraspinatus Tendinitis. It’s also an axis pressure test for the humerus.[17]
The European Society of Shoulder and Elbow Surgery recommends using the Walch-Duplay score which was inspired by the Rowe rating scale and takes into account both subjective and objective data (stability, pain, sport level recovery, mobility) to assess clinical outcome. The Walch-Duplay score is the most currently used score in Europe for the assessment of the patient undergoing shoulder stabilization surgery. However, it is not a self-administrated questionnaire.
The Walch-Duplay score (0 to 100 points) is composed of four items: activity, stability, pain and mobility. According to the Walch-Duplay score, results were classified as excellent (91 and 100 points), good (76 and 90 points), fair (51–75 points) or poor (under 50).[19]
Outcome Measures[edit | edit source]
- Visual Analogue Scale
- DASH-questionnaire
- Shoulder Pain and Disability Index (SPADI)
- Constant-Murley score (CMS)
- Shoulder Disability Questionnaire (SDQ)
Physical Therapy Management[edit | edit source]
Treatment in the acute phase include:
- Rest from all activity
- RICE regime to reduce inflammation and treat pain
- Codman’s pendulum exercises and AAROM exercises to keep the joint in motion, prevent stiffness and speed recovery[20]
The aim of the therapy:
1) Reduce the symptoms
2) Minimize damage
3) Maintain Rotator Cuff motion and strength
Once the inflammation has been reduced, ultrasound therapy can be used to continue the healing process.[21]
The best initial approach for a Scapulothoracic bursitis is a nonoperative treatment plan that combines scapular strengthening, postural reeducation, and core strength endurance.
One study focusing examined the difference between one group treated with ultrasound-guided injection (UGI) and another group with ultrasound-guided injection and home exercise program (UGI-exercise) for 1 month the treatment of Subacromial Bursitis. Exercises included exercises for shoulder lowering with decoaptation that the patient must remember to reproduce during all the common daily activities. In addition to assisted active self-mobilization for the recovery of range of motion in all directions and isometric strengthening with elastic bands for Rotator Cuff muscles and Deltoid. Lastly, stretching in elevation, abduction and rotation performed statically by placing the patient-specific postures that allow the lengthening of the shortened muscles and the recovery of the last degrees of movement. The study concluded that ultrasound-guided injection combined with shoulder exercises in the treatment of Subacromial Bursitis is effective in relieving pain in the short and medium term.[22]
Once the pain starts to diminish, the physiotherapist will set up an individualized shoulder strengthening and stretching exercise program. Patients with shoulder bursitis can learn ways to move the shoulder in ways that will not reproduce inflammation.[14]
The following are exercises that can be implemented into the therapy program and built up progressively:
Table Slides (Flexion): Start with your hand on a table (facing the table) on a towel as shown below, Stretch your arm forward on the table by sliding the towel. Feel a stretch under your arm. Do 20-30 repetitions. This exercise is modified for abduction as well.
Scapular wall slides: Stand in an upright position with your back against the wall. Raise your arms in 90 degrees abduction and flex your elbows to the 90 degree position as well. Your arms have to be pressed against the wall at all times. Make sure your handpalms are facing forward. Now you will abduct your arms as high as you can while extending the elbows at the same time. Do this slowly and go back to the starting position. Do 10 – 12 repititions.[20]
Upper Trap (UT) Stretch: Sit on a table or chair and use the hand of the affected side to grip under the table, stabilizing the shoulder downward. With the opposite hand, pull the head to the opposite shoulder, maintaining your gaze forward and feeling a stretch in the upper trap muscle. Hold for 30 seconds and do 1-3 repetitions two times a day. [21]
Open Book Stretch: Placed a rolled up towel on a mat table between the shoulder blades and lie flat on your back. Keep your arms folded together over the top of your body, with your hands together. Open your arms up, like you are simulating the opening of a book, feeling a stretch in the front of your shoulder. Hold for 30-60 seconds and do 1-3 repetitions two times a day.
Rowing (using a theraband): This is a good exercise to train the scapular stabilizing muscles.[27]
Sit in a chair as shown or stand. Anchor a theraband to a door or pole, making sure that the anchor point is around
chest level. Pull the theraband backwards most importantly pulling the shoulder blades together. Do two sets of 10-20 repetitions three times a week.
Low Row Isometric: .[12]
Key Evidence[edit | edit source]
Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61. Level of evidence: 1B
Clinical Bottom Line[edit | edit source]
Shoulder bursitis is a common cause of shoulder pain. This bursitis is in most cases caused by an overload, trauma, an inflamed joint or elder age as it lays between different structures such as muscles, bones or other structures. Since it is mostly caused by another pathology nearby, it is very difficult to differentiate these many shoulder pathologies. Pain, decreased range of motion, loss of strength and loss of functionality are the main complaints of the patients. There is evidence using ultrasound guided-injection in combination with physical therapy reduces pain and are beneficial for the recovery.
References[edit | edit source]
- ↑ 1.0 1.1 radiopedia Shoulder Bursae Available;https://radiopaedia.org/articles/shoulder-bursae (accessed 13.4.2022)
- ↑ 2.0 2.1 2.2 John Hopkins Shoulder Bursitis Available:https://www.hopkinsmedicine.org/health/conditions-and-diseases/shoulder-bursitis (accessed 13.4.2022)
- ↑ Chang, Won Hyuk, et al. "Comparison of the therapeutic effects of intramuscular subscapularis and scapulothoracic bursa injections in patients with scapular pain: a randomized controlled trial." Rheumatology international34.9 (2014): 1203-1209
- ↑ Hsieh, Lin-Fen, et al. "Is ultrasound-guided injection more effective in chronic subacromial bursitis?." Medicine and science in sports and exercise 45.12 (2013): 2205-2213.
- ↑ J. Willis Hurst, Douglas C. Morris, Chest pain, Futura publishing company, 2001.
- ↑ Salzman, Keith L., W. A. Lillegard, and J. D. Butcher. "Upper extremity bursitis." American family physician 56 (1997): 1797-1814
- ↑ 7.0 7.1 Walker‐Bone, Karen, et al. "Prevalence and impact of musculoskeletal disorders of the upper limb in the general population." Arthritis Care & Research 51.4 (2004): 642-651.
- ↑ Downing, Deborah Swan, and Arthur Weinstein. "Ultrasound therapy of subacromial bursitis A double blind trial." Physical therapy 66.2 (1986): 194-199
- ↑ Lee JH, Lee SH, Song SH. Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. Clinical journal Pain. 2011 Jul-Aug: 27 page 523 - 528
- ↑ Lee S, Park J, Lee D. The Effects of Cervical Stabilization Exercises on the Electromyographic Activity of Shoulderstabilizers. Journal Of Physical Therapy Science, 2013 December: 12 page 1557 - 1660
- ↑ Gardner E. The innervation of the shoulder joint. The Anatomical Record,1948:102 page 1-18.
- ↑ 12.0 12.1 Conduah, Augustine H., and Champ L. Baker. "Clinical management of scapulothoracic bursitis and the snapping scapula." Sports Health: A Multidisciplinary Approach 2.2 (2010): 147-155
- ↑ Hitzrot, James Morley. "Surgical diseases of the shoulder bursae." Annals of surgery 98.2 (1933): 273.
- ↑ 14.0 14.1 O. Dreeben-Irimia, introduction to physical therapy for physical therapist assistants, 2011, p 84-85.
- ↑ Hardwick DH, Beebe JA, McDonnell MK, Lang CE. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. Journal of Orthopedic Sports Physical Therapy, 2006 December: 36(12) page 903 – 910.
- ↑ Hawkin's Test. available from: https://www.youtube.com/watch?v=OYK5qL2om-c
- ↑ Ide K, Shirai Y, Ito H, Ito H. Sensory nerve supply in the human subacromial bursa. Journal of Shoulder and Elbow Surgery, 1996 September – October: 5 page 371 – 382.
- ↑ shoulder compression/rotation test. available from: https://www.youtube.com/watch?v=bxbluwK-IfM
- ↑ Mamiko Noguchi, Jaclyn N. Chopp, Stephanie P. Borgs, Clark R. Dickerson. Scapular orientation following repetitive prone rowing: Implications for potential subacromial impingement mechanisms. Journal of Electromyography and Kinesiology, 2013 Decemeber: 23 page 1356 – 61
- ↑ 20.0 20.1 O. Dreeben, physical therapy clinical handbook, Jones and Barlett, 2008, p209-211.
- ↑ 21.0 21.1 Williams, bursitis of the shoulder, home therapy, 2001
- ↑ Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61.
- ↑ Shoulder Flexion Table Slides - Ask Doctor Jo. Available from: https://www.youtube.com/watch?v=pgsPQ1_5e0w
- ↑ Scapular Wall Slides. available from: https://www.youtube.com/watch?v=UB_n4DxOTCo&t=61s
- ↑ Upper Trapezius Stretch - Ask Doctor Jo. available from: https://www.youtube.com/watch?v=-r0eoFS7_5Q
- ↑ Open Book Reach Stretch. available from: https://www.youtube.com/watch?v=MJNCJOFhVtI
- ↑ Chen, Max JL, et al. "Ultrasound-guided shoulder injections in the treatment of subacromial bursitis." American journal of physical medicine & rehabilitation 85.1 (2006): 31-35.
- ↑ Thera Band Rows. available from: https://www.youtube.com/watch?v=4g8NSz4crE0
- ↑ isometric low row. available from: https://www.youtube.com/watch?v=y3KoUkInlMc