Chronic Pelvic Pain: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
</div> | </div> | ||
== Search Strategy == | == Search Strategy == | ||
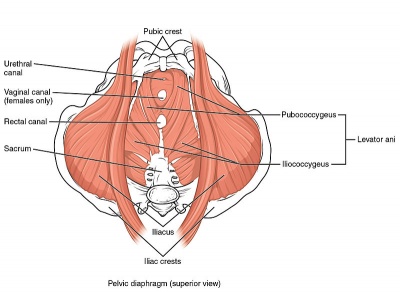
[[Image:Pelvic_Floor_Muscles.jpg|right|400px]] | |||
PubMed (most successful keywords): | PubMed (most successful keywords): | ||
Revision as of 16:17, 19 April 2014
Top Contributors - Nina Lefeber, Kim Jackson, Laura Ritchie, Khloud Shreif, Andeela Hafeez, Admin, Nicole Hills, Aminat Abolade, Vidya Acharya, 127.0.0.1, WikiSysop, Melissa Coetsee, Rachael Lowe and Evan Thomas
Search Strategy[edit | edit source]
PubMed (most successful keywords):
- Chronic pelvic pain
- Chronic pelvic pain women
- Physical therapy chronic pelvic pain
- Chronic pelvic pain rehabilitation
Definition/Description
[edit | edit source]
Chronic pelvic pain (CPP) is commonly defined as nonmalignant intermittent or continuous pain in the lower abdomen, pelvis or intrapelvic structures, lasting at least 3–6 months.[1] If nonacute and central sensitization pain mechanisms are present, the condition is considered chronic, regardless of the time frame.[2] Central sensitization is characterized by amplification or increased sensory perception, where stimuli that are normally not painful are now perceived as painful.[3] CPP is in women not exclusively associated with the menstrual cycle, sexual intercourse or pregnancy[1], but is sufficiently severe to cause functional disability or to lead to medical care.[4]
Clinically Relevant Anatomy
[edit | edit source]
Epidemiologically CPP has a greater incidence in women than in men, and is mostly present between the ages of 36 and 50 years.[2] The etiology of CPP however is not clear. It can be difficult and complex to determine the cause of pain; in fact, no specific cause may be discovered. Many women are not able to identify a specific set of problems which can cause the problems and allowing for the diagnosis to be made.[5] CPP may originate from one or more organ systems or pathologies and may have multiple contributing factors. It usually involves an interaction between the gastrointestinal, urinary, gynecologic, musculoskeletal, neurologic and endocrine systems. It can also be influenced by psychological and sociocultural factors.[4]
Epidemiology /Etiology
[edit | edit source]
add text here
Characteristics/Clinical Presentation[edit | edit source]
Chronic pelvic pain has numerous presentations, and women with the same problem may exhibit different characteristics. Common symptoms include:
- constant severe pelvic pain
- intermittent pain
- sharp or cramping pain
- dull aching
- pressure
Many women miss work, have difficulty doing non strenuous exercises, and have difficulty sleeping. The level of pain can vary greatly and can contrast from mild to disabling.[5]
Differential Diagnosis
[edit | edit source]
| Gastrointestinal | Celiac disease, colitis, colon cancer, inflammatory bowel disease, irritable bowel syndrome |
| Gynecologic | Adhesions, adenomyosis, adnexal cysts, chronic endometritis, dysmenorrhea, endometriosis, gynecologic malignancies, leiomyomata pelvic congestion syndrome, pelvic inflammatory disease |
| Musculoskeletal | Degenerative disk disease, fibromyalgia, levator ani syndrome, myofascial pain, peripartum pelvic pain syndrome, stress fractures |
| Psychiatric/neurologic | Abdominal epilepsy, abdominal migraines, depression, nerve entrapment, neurologic dysfunction, sleep disturbances, somatization |
| Urologic | Bladder malignancy, chronic urinary tract infection, interstitial cystitis, radiation cystitis, urolithiasis |
| Other | Familial Mediterranean fever, herpes zoster, porphyria |
Diagnostic Procedures[edit | edit source]
add text here
Outcome Measures
[edit | edit source]
add text here
Examination
[edit | edit source]
add text here
Medical Management[edit | edit source]
add text here
Physical Therapy Management[edit | edit source]
The optimal treatment of CPP is based on a biopscychosocial model delivered by a multidisciplinary approach. This multidisciplinary treatment concludes oral analgesics and other medications, pain management, pelvic floor rehabilitation, nerve stimulation therapies, teaching cognitive coping strategies, educate about the importance of planning and pacing exercise and activities.[3]
Pelvic Floor Rehabillitation
Increasing evidence suggests that PFM dysfunction is associated with CPP. Montenegro et al found recently a significant difference between the prevalence of PFM pain in women with multiple CPP conditions and in women who were healthy. This suggests a relationship between the presence of an organic pain condition and PFM pain. A recent (2010) systematic review concluded that myofascial pain in the PFMs is associated with several different CPP conditions that occur in women.[2] (Level of evidence: 2C)
Therefore pelvic floor rehabilitation is a part of the treatment. Treatment interventions which are applied are[2]
- manual therapy of the pelvic floor muscles
- electromyographic biofeedback
- electrical stimulation
- myofascial release of painful trigger points of the pelvic floor
- Thiele massage techniques
- relaxation
- PFM exercises
- specific stretches; although this may take in excess of six months to show any benefit[3]
Pain physiotherapy / management
Pain management and cognitive coping strategies should include education about how psychological factors, such as catastrophizing, pain related fear and anxiety, may affect sexual function and the perception of pain during intercourse and other activities for which patients may report pain.[6] (Level of evidence: 3A)
Pain management should also include educating patients about the importance of planning and pacing exercise and activities. The goal is to enable patients to pace their activity to achieve a similar amount each day. Overactive patients may experience constant pain with exacerbations called flare-ups, while others may have constant pain with flare-ups associated with minimal activity.[3] (Level of evidence : 2A)
In addition, therapy can include education about vulvodynia, dyspareunia (painful intercourse), muscle relaxation, Kegel exercises, and vaginal dilation. The goals of the therapy are reducing the fear of pain and other pain-related cognitions associated with intercourse, increase sexual activity level, and decrease pain.[6] (Level of evidence: 3A)
Key Research
[edit | edit source]
add links and reviews of high quality evidence here
Resources[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Díaz Mohedo E, Barón López FJ, Pineda Galán C, Dawid Milner MS, Suárez Serrano C, Medrano Sánchez E., Discriminating power of CPPQ-Mohedo: a new questionnaire for chronic pelvic pain, J Eval Clin Pract. 2011 Oct 26. doi: 10.1111/j.1365-2753.2011.01778.x. (Level of evidence : 2C)
- ↑ 2.0 2.1 2.2 2.3 Alappattu MJ, Bishop MD., Psychological factors in chronic pelvic pain in women: relevance and application of the fear-avoidance model of pain, Phys Ther. 2011 Oct;91(10):1542-50. doi: 10.2522/ptj.20100368. Epub 2011 Aug 11. (Level of evidence : 2C)
- ↑ 3.0 3.1 3.2 3.3 Cambitzi J, Chronic pelvic pain: causes, mechanisms and effects, Nursing Standard, 25, 20, 35-38. Date of acceptance: March 26 2010 (Level of evidence : 2A)
- ↑ 4.0 4.1 Silva GP, Nascimento AL, Michelazzo D, Alves Junior FF, Rocha MG, Silva JC, Reis FJ, Nogueira AA, Poli Neto OB., High prevalence of chronic pelvic pain in women in Ribeira˜o Preto, Brazil and direct association with abdominal surgery, Clinics (Sao Paulo). 2011;66(8):1307-12. (Level of evidence : 2B)
- ↑ 5.0 5.1 John D. Paulson, MD, Joseph N. Paulson, Anterior Vaginal Wall Tenderness (AVWT) as a Physical Symptom in Chronic Pelvic Pain, JSLS. 2011 Jan-Mar;15(1):6-9. (Level of evidence : 2B)
- ↑ 6.0 6.1 6.2 David D. Ortiz, MD, Chronic Pelvic Pain in Women, Am Fam Physician. 2008;77(11):1535-1542, 1544. (Level of evidence : 3A)