Trigger Finger: Difference between revisions
Holly Pulket (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Extracorporeal Shockwave Therapy (ESWT)" to "[[Extracorporeal Shockwave Therapy ") |
||
| (248 intermediate revisions by 25 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original and Lead Editors''' - [[User:Holly Pulket|Holly Pulket]], [[User:Hilary Zachary|Hilary Zachary]], [[User:Angela Dempski|Angela Dempski]], [[User:Dana Williams|Dana Williams]], [[User:Shannon Davis|Shannon Davis]] as part of the [[Texas State University Evidence-based Practice Project|Texas State University's Evidence-based Practice project space]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | </div> | ||
== Introduction == | |||
Each hand digit can move freely throughout a full range of motion (ROM) into flexion and extension. | |||
= | The efficiency, fluidity, and forcefulness of such movements are made possible by several "pulleys" on the digit of the hand. These pulley systems comprise a series of retinacular-type structures that are either annular or cruciform.<ref name="Makkouk">Makkouk AH, Oetgen ME, Swigart CR, Dodds SD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684207/ Trigger finger: aetiology, evaluation, and treatment.] Current Reviews in Musculoskeletal Medicine. 2008 Jun 1;1(2):92-6.</ref> There are five annular pulleys (A1-A5) and three cruciform pulleys (C1-C3). | ||
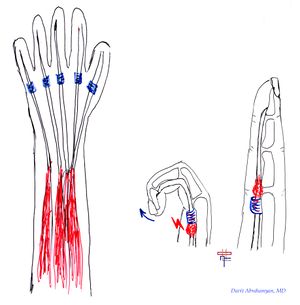
Trigger finger | '''Trigger finger is thought to be caused by inflammation and subsequent narrowing of the A1 pulley of the affected digit, typically the third or fourth.''' The A1 pulley is most often affected, but there are some reported cases where the A2 and A3 pulleys were involved <ref name="Makkouk" />. It can also occur in the [[Thumb Ligament Injuries|thumb]] and is then called trigger thumb.<ref name=":2">Deskur A, Deskur Z. [http://yadda.icm.edu.pl/yadda/element/bwmeta1.element.psjd-83febc66-25f7-4967-aab0-899f3637b269/c/CEJSSM_1_2017_07.pdf Surgical Treatment and Rehabilitation of Trigger Thumb and Finger.] Central European Journal of Sport Sciences and Medicine. 2017;17(1):61-6.</ref> A difference in size between the [[Flexor Tendon Injuries|flexor tendon]] sheath and the flexor tendons may lead to abnormalities of the gliding mechanism by causing actual abrasion between the two surfaces, resulting in progressive inflammation between the tendons and the sheath.<ref name="Andreu" /> | ||
[[File:Trigger finger .jpg|right|frameless]] | |||
Commonly, the trigger finger is referred to as "'''stenosing tenosynovitis'''". However, histologic studies have shown that the inflammation occurs more so in the tendon sheaths rather than the tendosynovium, making this name a false depiction of the actual pathophysiology of the condition.<ref name="Makkouk" /> | |||
== Epidemiology/ | == Epidemiology/Aetiology == | ||
Statistically, trigger finger is more likely to develop in the '''fifth or sixth decade of life''' and women are up to six times more likely to develop trigger finger than men.<ref name="Makkouk" /><ref name="Andreu" /> The average age is 58 years<ref name=":0" />. The chance of developing a trigger finger is 2-3%, but in the [[Diabetes|diabetic population]], it rises to 10%.<ref>Bianchi S, Gitto S, Draghi F. Ultrasound Features of Trigger Finger: Review of the Literature. Journal of Ultrasound in Medicine. 2019 Dec;38(12):3141-54.</ref> This is not due to glycemic control but rather due to the duration of the disease. Trigger finger can concomitantly occur in patients with: | |||
*[[Carpal Tunnel Syndrome|Carpal Tunnel Syndrome]] | |||
*[[De Quervain's Tenosynovitis|DeQuervain's disease]] | |||
*[[Hypothyroidism]] | |||
*[[Rheumatoid Arthritis|Rheumatoid arthritis]] | |||
*Renal disease | |||
*Amyloidosis<ref name="Makkouk" /><br> | |||
== | There have been many potential causes of trigger finger discussed throughout the literature. However, there is little to no evidence of precise aetiology. | ||
* Occupational-related causes of the trigger finger have been proposed. Still, the research linking the two is very inconsistent<ref name="Makkouk" /><ref name="Andreu">Andreu JL, Oton T, Silvia-Fernandez L, Sanz J. Hand pain other than carpal tunnel syndrome (CTS): The role of occupational factors. Best Practice and Research Clinical Rheumatology. 2011;25:31–42.</ref> | |||
* Authors suggest that trigger finger can manifest from any activity requiring '''prolonged forceful finger flexion''' (i.e. carrying shopping bags or a briefcase, prolonged writing, rock climbing, or the strenuous grasping of small tools or objects with sharp edges<ref name=":0">Szmiga L. Trigger Finger. Plus Course 2020 </ref>).<ref name="Makkouk" /><ref name="Andreu" /><ref name="Schoffl" /> | |||
* It is essential to consider that the cause of the trigger finger is often multi-factorial. | |||
* The condition could develop idiopathically or secondary to other pathologies. <ref name=":0" /> | |||
{{#ev:youtube|Ej8FwzKnmHo}} | |||
== Clinical Presentation == | |||
The trigger finger has a range of clinical presentations. Initially, patients may present with painless clicking during the movement of the digit. This can progress to painful catching or popping, typically at the metacarpophalangeal (MCP) or proximal interphalangeal (PIP) joints. | |||
'''Possible additional symptoms are:''' | |||
* Stiffness and [[Oedema Assessment|swelling]] (especially in the morning) | |||
* Intermittent finger locking during active flexion that requires a passive force to extend the finger<ref name=":0" /> | |||
* Finger locking or clicking in a bent position, then popping straight | |||
* Loss of full flexion/extension | |||
* Palpable painful nodule proximal to A1, and / or finger locked into a flexed position<ref name="Makkouk" /> | |||
* Slight thickening at the base of the digit and pain that may radiate to the palm or to the distal aspect of the digit<ref name="Colbourn" /> | |||
== Differential Diagnosis == | |||
The main characteristic of the trigger finger is popping and/or catching with the movement of the digit. However, this characteristic is not unique to just the trigger finger. Other aetiologies associated with a locking digit include:<ref name="Makkouk" /> | |||
*[[Dupuytren’s Contracture|Dupuytren's contracture.]]<ref name="Schoffl">Schöffl VR, Schöffl I. Finger pain in rock climbers: reaching the right differential diagnosis and therapy. J Sports Med Phys Fitness. 2007;47:70-78.</ref> | |||
*Focal [[dystonia]]. | |||
*Flexor tendon/sheath tumour. | |||
*[[Sesamoiditis|Sesamoid bone anomalies]]. | |||
*Post-traumatic tendon entrapment on the metacarpal head.<br> | |||
*DeQuervain's (for trigger thumb only) | Complaints of pain at the MCP joint could be associated with any of the following:<ref name="Makkouk" /> | ||
*Ulnar collateral ligament injury/Gamekeeper's thumb | *[[De Quervain's Tenosynovitis|DeQuervain]]'s (for trigger thumb only) | ||
*Ulnar collateral ligament injury / [[Gamekeeper’s Thumb|Gamekeeper's thumb]]<ref name="Schoffl" /> | |||
*MCP joint sprain | *MCP joint sprain | ||
*Extensor apparatus injury | *[[Traumatic Extensor Hood Rupture|Extensor apparatus injury]] | ||
*MCP joint osteoarthritis | *MCP joint [[osteoarthritis]]<ref name="Schoffl" /><br> | ||
Diagnosis of the trigger finger is based on the patient's signs and symptoms. | |||
< | * [[Ultrasound Scans|Ultrasound]] is used to measure the affected sheath's thickness and compare it with an unaffected sheath. The degree of thickening seen on ultrasound is correlated with symptom severity.<ref>Matthews A, Smith K, Read L, Nicholas J, Schmidt E. Trigger finger: An overview of the treatment options. Journal of the American Academy of PAs. 2019 Jan 1;32(1):17-21.</ref> Injection of lidocaine into the flexor sheath to relieve the pain and allow joint movement, can also help in the diagnosis.<ref name="Makkouk" /> | ||
'''Read these documents on differential diagnosis:''' | |||
*[http://www.scottsevinsky.com/pt/reference/wrist/johs_trigger_digits.pdf Trigger Digits: Principles, Management, and Complications] | |||
*[http://www.nursingcenter.com/pdfjournal?AID=1630354&an=00006416-201311000-00003&Journal_ID=403341&Issue_ID=1630347 Disorders of the Hand: A Case Study Approach] | |||
== Outcome Measures == | == Outcome Measures == | ||
*[[Numeric Pain Rating Scale]] | |||
*Grip Strength (Jamar [http://www.uhs.nhs.uk/Media/Southampton-Clinical-Research/Procedures/BRCProcedures/Procedure-for-measuring-gripstrength-using-the-JAMAR-dynamometer.pdf dynameter])<ref name="Colbourn" /> | |||
*[https://www.physio-pedia.com/DASH_Outcome_Measure DASH Outcome Measure] | |||
*Stages of Stenosing Tenosynovitis (SST)<ref name="Colbourn" /> | |||
**1 = Normal | |||
**2 = A painful palpable nodule | |||
**3 = Triggering | |||
**4 = The proximal interphalangeal (PIP) joint locks into flexion and is unlocked with active PIP joint extension | |||
**5 = The PIP joint locks and is unlocked with a passive PIP joint extension | |||
**6 = The PIP joint remains locked in a flexed position | |||
*Participant Perceived Improvement in Symptoms Rating Scale<ref name="Colbourn" /> | |||
**1 = Resolved | |||
**2 = Improved, but not completely resolved | |||
**3 = Not resolved | |||
**4 = Resolved but triggering at the distal interphalangeal/proximal interphalangeal joint(s) | |||
**5 = Resolved at ten weeks versus six weeks | |||
*Open & Close Hand 10 Times<ref name="Colbourn" /> - Patient is to actively make ten fists. The number of triggering events in ten active full fists is then scored out of 10. If the patient’s finger remains locked at any time, the test is completed, and an automatic score of 10/10 is recorded<ref name="Colbourn" /><u></u> | |||
== Examination == | |||
=== History === | |||
Ask the patient-specific questions to understand more about the nature of their symptoms that would help you in the diagnosis of their condition, such as: | |||
*Recent trauma<ref name="Makkouk" /> | |||
*Job-related repetitive movements | |||
*Locking or snapping while flexing or extending the affected digit<ref name="Harvard Women's Health Watch">Tendon trouble in hand: de Quervain's tenosynovitis and trigger finger. Harvard Women's Health Watch.2010:4-5.</ref> | |||
*Radiating pain to the palm or digits<ref name="Harvard Women's Health Watch" /> | |||
=== Past Medical History === | |||
*[[Diabetes|Diabetic]] individuals are four times more likely to develop trigger finger<ref name="Harvard Women's Health Watch" /> | |||
*Disorders which cause connective tissue changes such as RA and [[Gout]] are also associated with trigger finger<ref name="Colbourn">Colbourn J, Heath N, Manary S, Pacifico D. [https://d1wqtxts1xzle7.cloudfront.net/57978667/j.jht.2008.05.00120181212-4071-iwkj8x.pdf?1544619286=&response-content-disposition=inline%3B+filename%3DEffectiveness_of_Splinting_for_the_Treat.pdf&Expires=1608321474&Signature=ZzAeO4q-6Pp-Y7a4EUby6rL1QN92kZ Effectiveness of splinting for the treatment of trigger finger]. Journal of Hand Therapy.2008; 21(4):36-343.</ref><u></u> | |||
=== Observation === | |||
*A digit locked in flexion | |||
*Bony proliferative changes in the sub-adjacent PIP joint<ref name="Howitt">Howitt S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1864591/pdf/jcca-v50-4-249.pdf The conservative treatment of trigger thumb using Graston techniques and active release technique]. JCCA. 206;50(4):249-254.</ref> | |||
=== Palpation === | |||
*Painful nodule in the palmar MCP secondary to intratendinous swelling<ref name="Makkouk" /> | |||
=== Range of Movement === | |||
*Loss of motion, particularly in extension<u></u> | |||
=== Manual Muscle Testing === | |||
*[[Flexor Digitorum Profundus]] | |||
*[[Flexor Digitorum Superficialis|Flexor Digitorum Superficialis ]] | |||
*Grip strength using the Jamar Dynameter<ref name="Colbourn" /> | |||
Note: If the finger is locked, testing may not be possible. | |||
=== Joint Accessory Mobility === | |||
*PIP, MCP, Distal interphalangeal (DIP) joint, and carpometacarpal (CMC) joint of all affected digits<ref name="Makkouk" /> | |||
*Surrounding tissues | |||
*[[Wrist and Hand|Wrist joint]] | |||
=== Special Tests === | |||
*[[Wrist and Hand Examination|Open and Close hand]] 10x<ref name="Colbourn" /> | |||
== Management == | |||
The chronic symptoms associated with trigger fingers make conservative treatment difficult and often frustrating. Still, conservative care (listed below in Physical Therapy Management) is always recommended as a treatment plan before surgical intervention.<ref name="Howitt" /> | |||
=== Non-operative Management === | |||
==== Corticosteroid Injection ==== | |||
Corticosteroid use is effective in reducing pain and frequency of triggering. Different types of steroids can be injected into the affected tendon: triamcinolone, dexamethasone or methylprednisolone and their choice can significantly affect the clinical outcome: <ref>Roberts JM, Behar BJ, Siddique LM, Brgoch MS, Taylor KF. Choice of corticosteroid solution and outcome after injection for trigger finger. Hand. 2021 May;16(3):321-5.</ref> | |||
* triamcinolone: patients required additional injections | |||
* methylprednisolone: patients had surgical release performed earlier and more frequently. | |||
The goal of the injection is to reduce the inflammation and pressure on the tendon for better gliding through the flexor pulleys. Application by a primary care provider can be an effective and safe alternative to surgical therapy. Patient satisfaction, safety, and functional improvement are characteristics of steroidal injections compared to surgical treatment.<ref name="Peters-Veluthamaningal" /> Surgery is associated with higher costs, long absence from work, and possible surgical complications. Studies have also shown that the combination of corticosteroid injections with lidocaine is significantly more effective than lidocaine alone.<ref>Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for adult trigger finger. Cochrane Database Syst Rev. 2009; (1): CD005617. </ref> | |||
'''Possible Side effects<u><ref name="Peters-Veluthamaningal">Peters-Veluthamaningal C, Winters JC, Groenier KH et al. Corticosteroid injections effective for trigger finger in adults in general practice: a double-blinded randomised placebo-controlled trial. Annals of the Rheumatic Diseases. 2008;67;1262-1266.</ref></u>''' | |||
*Flaring at the injection site | |||
*Local infections | |||
*Tendon ruptures | |||
*Allergic reactions | |||
*Atrophy of subcutaneous fat tissue | |||
'''Contraindications<u><ref name="Peters-Veluthamaningal" /></u>''' | |||
*Under 18 years old | |||
*Any prior treatment or surgery to the area within the last six months | |||
*Possible traumatic or neoplastic origin of symptoms | |||
==== Physical Therapy Management ==== | |||
As with all upper extremity disorders, proximal segments must be screened. Also, because posture can contribute to distal problems, it should be addressed to provide the patient with optimal outcomes.<ref name="Yung">Yung E, Asavasopon S, Godges J. Screening for the head, neck, and shoulder pathology in patients with upper extremity signs and symptoms. Journal Of Hand Therapy [serial online]. April 2010;23(2):173-186. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed November 23, 2011.</ref> | |||
'''Patient Education''' | |||
Since the trigger finger is an overuse injury, education is critical. Education should be given on: | |||
*Rest | |||
*Modifications of activities<ref name="Salim">Salim, N., S. Abdullah, J. Sapuan, and N. H. M. Haflah.The outcome of corticosteroid injection versus physiotherapy in treating mild trigger fingers. Journal of Hand Surgery (European Volume) 0th ser. 0.0 (2011): 1-8. November 19, 2011.</ref> | |||
*Specialized tools | |||
*[[Splinting]] | |||
*Modalities | |||
*Posture | |||
'''Splinting''' | |||
== | The first step in treatment is to stop doing activities that aggravate the condition. Splinting is one of the best ways to limit motion. Most authors agree that splinting intends to alter the biomechanics of the flexor tendons while encouraging maximal differential tendon glide. However, authors disagree on which joints to include in the splint and the degree of joint positioning.<ref name="Colbourn" /> There are various ways to splint a patient, but, ultimately, it will depend on what provides the patient with the most relief. Splints are usually worn for 6-10 weeks<ref>Lunsford D, Valdes K, Hengy S. Conservative management of trigger finger: A systematic review. Journal of Hand Therapy. 2019 Apr 1;32(2):212-21.</ref>. Some authors recommended positioning the MCP joint at 0 degrees and allowing full DIP joint movement<ref name=":0" />. It should be noted that splinting yields lower success rates in patients with severe triggering or longstanding duration of symptoms.<ref name="Makkouk" /> | ||
'''Two major types of splinting most recently studied:''' | |||
== | #Splinting at the DIP joint. This showed to have a resolution in 50% of the patient’s symptoms<ref name="Makkouk" /> | ||
#Splinting at the MCP joint with 15 degrees of flexion. This showed a resolution of the patient’s symptoms of 92.9%.<ref name="Colbourn" /> | |||
#Night splinting of the affected finger for 6 to 9 weeks has been shown to augment the patient's compliance over continuous splinting. 55% of patients with grade 1 and 2 Trigger Finger demonstrated the resolution of symptoms for less than three months when wearing a night splint for six weeks.<ref>Merry SP, O’Grady JS, Boswell CL. [https://journals.sagepub.com/doi/abs/10.1177/2150132720943345 Trigger finger? Just shoot!.] Journal of Primary Care & Community Health. 2020 Jul;11:2150132720943345.</ref> | |||
[[Image:Splints.jpeg|MCP Splints]] [[Image:Splint on hand.jpeg|MCP Splint on Hand]] | |||
'''Exercises''' | |||
== | Three [[Therapeutic Exercise|exercises]] are recommended in the management of trigger fingers particularly following surgical release<ref name=":0" />: | ||
* Digit blocking: patient blocks the MCP joint and allows the PIP joints to bend. This exercise could be done with all fingers simultaneously or individually. The same activity could be repeated at the DIP joint. Repetition and frequency are advised according to the level of stiffness and pain | |||
* Tendon gliding: check the video below for the sequence of movement | |||
* Active range of motion: Finger abduction and adduction are recommended to strengthen the interossei and the lumbricals | |||
{{#ev:youtube|favZefGkiHk}}<ref>Tendon Glide Exercises | Ability Rehabilitation . Available from:https://www.youtube.com/watch?v=favZefGkiHk[last accessed 2/12/2020]</ref> | |||
'''Other modalities''' | |||
= | Modalities such as [[Thermotherapy|heat/ice]], [[Therapeutic Ultrasound|ultrasound]], [[Electrical Stimulation - Its role in upper limb recovery post-stroke|electric stimulation]], [[massage]], [[stretching]], and joint motion (active and passive) can have some positive effects on the trigger finger. It is thought that heat can help by providing increased blood flow and extensibility to the tendon. Stretching after applying heat can provide more extensibility with plastic deformation. Joint movement and mobilisations increase joint and soft tissue mobility via slow, passive therapeutic traction and translational gliding.<ref name="Salim" /><ref>Ferrara PE, Codazza S, Maccauro G, Zirio G, Ferriero G, Ronconi G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7459363/pdf/or-12-s1-8680.pdf Physical therapies for the conservative treatment of the trigger finger: a narrative review.] Orthop Rev (Pavia). 2020 Jun 26;12(Suppl 1):8680.</ref> | ||
Although the evidence is lacking, some documented cases and studies of improvement with various combinations of these techniques exist: | |||
== | *74 patients were treated with ten sessions of wax therapy, ultrasound, stretching muscle exercises and massage. At three months, 68.8 per cent of patients reported no pain or triggering. Of this 68.8 per cent of patients, none had pain or triggering at six months<ref name="Salim" /> | ||
*60 trigger thumbs in 48 children were treated daily with passive exercises of their affected thumb by their mother. This resulted in a cure rate of 80 per cent for stage 2 and 25 per cent for stage 3 thumbs after an average of 62 months<ref name="Watanabe">Watanabe, H., Yoshiki Hamada, Tadahito Toshima, and Koki Nagasawa. Conservative treatment for trigger thumb in children. Archives of Orthopaedic and Trauma Surgery. 2001;121(7):388-90.</ref> | |||
'''Extracorporeal Shockwave Therapy''' | |||
Recently, [[Extracorporeal Shockwave Therapy |extracorporeal shock wave therapy]] (ESWT) has been advanced as a possible alternative to surgery for treating musculoskeletal disorders in patients recalcitrant to traditional conservative treatment. | |||
== | Yildirim and colleagues carried out a prospective randomized controlled clinical trial to determine the efficacy of ESWT in the treatment of trigger finger versus corticosteroid injection.<ref name=":1" /> Patients were followed up at one, three and six months. They found that three sessions of ESWT treatment could be as effective as a corticosteroid injection for improving symptom severity and functional status in patients with a grade 2, according to the Quinnell classification. For three sessions, patients in the ESWT group received 1000 shocks at an energy flux density of 2.1 bar (frequency 15 Hz). There was a one-week break between each session.<ref name=":1">Yildirim P, Gultekin A, Yildirim A, Karahan AY, Tok F. Extracorporeal shock wave therapy versus corticosteroid injection in the treatment of trigger finger: a randomized controlled study. J Hand Surg Eur Vol. 2016 Nov;41(9):977-983.</ref> They found that ESWT and corticosteroid groups statistically significantly improved all outcomes after treatment.<ref name=":1" /> | ||
It is believed that ESWT induces the repair of inflamed tissues by tissue regeneration and stimulates nitric oxide synthase, leading to the suppression of ongoing inflammation in the soft tissues. There is also mild evidence that one of these mechanisms may benefit the thickening of the flexor tendon and its sheath. This may enable the obstruction in the trigger finger to be overcome.<ref>Seok H, Kim SH. The effectiveness of extracorporeal shock wave therapy vs. local steroid injection for management of carpal tunnel syndrome: a randomized controlled trial. Am J Phys Med Rehabil. 2013 Apr;92(4):327-34. </ref> Vahdatpour et al. <ref name=":3">Vahdatpour B, Momeni F, Tahmasebi A, Taheri P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7069581/pdf/oajsm-11-85.pdf The Effect of Extracorporeal Shock Wave Therapy in the Treatment of Patients with Trigger Finger]. Open Access J Sports Med. 2020 Mar 9;11:85-91. </ref> suggests that extracorporeal shock wave therapy can help with pain reduction, the severity of triggering, and the functional impact of triggering, lasting until the 18th week after the intervention. <ref name=":3" /> | |||
In general, it is recommended to use extracorporeal shock wave therapy in terms of a non-invasive intervention with no significant complications for patients with trigger finger.'''ESWT offers an alternative for people who reject corticosteroid injections because of potential complications, who are allergic to local anaesthetics or who have an intense fear of injections ('needle phobia'''').<ref>Akhtar S, Bradley MJ, Quinton DN, Burke FD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC558536/pdf/bmj33100030.pdf Management and referral for trigger finger/thumb]. BMJ. 2005 Jul 2;331(7507):30-3.</ref> | |||
=== Operative Management === | |||
< | |||
< | ==== Open Surgical Technique ==== | ||
</ | When conservative treatment fails, surgery is indicated.<ref name=":2" /> Open surgery combined with effective rehabilitation allows a rapid and significant improvement in hand function with a low complication risk.<ref name=":2" /> This technique, considered to be the gold standard,<ref name="Rajeswaran">Rajeswaran G., Lee J.C., Eckersley R., et al. Ultrasound-guided percutaneous release of the annular pulley in trigger digit. European Society of Radiology. 2009;19:2232-2237.</ref> is performed by making a longitudinal incision in the palmar crease over the metacarpophalangeal joint of the involved digit and followed by the release of the flexor digitorum superficialis and profundus tendons. This procedure lasts 2-7 minutes and has an average time of discomfort (45 days) post-op. An advantage to this technique is that it allows the pulley to be visualised and therefore has less risk of damage to the digital nerves than endoscopic techniques. | ||
==== Endoscopic Surgical Technique ==== | |||
This technique is performed by making two incisions: one at the palmar crease over the metacarpophalangeal and the other at the volar crease of the finger. An endoscope is then introduced to cut the pulley releasing the flexor tendons. This procedure lasts two to nine minutes and has a shorter average time of discomfort (23 days) post-op. Other advantages are the absence of scars and scar-related problems and shorter post-op rehabilitation. | |||
The endoscopic release offers complete visualization while minimizing soft tissue damage and incomplete or excessive release. <ref>Brown AM, DellaMaggiora RJ, Tsai EY, Kulber DA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7787330/pdf/gox-8-e3294.pdf Endoscopic Retrograde Approach for Trigger Finger Release: A Cadaver Study.] Plast Reconstr Surg Glob Open. 2020 Dec 21;8(12):e3294.</ref> However, the popularity of this technique is limited due to a steep learning curve and the cost of the instruments.<ref>Pegoli L, Cavalli E, Cortese P, Parolo C, Pajardi G. A comparison of endoscopic and open trigger finger release. Hand Surg. 2008;13(3):147-51. </ref> | |||
==== Percutaneous Release ==== | |||
This technique can be performed with or without imaging. Non-image-guided (blind) percutaneous release is performed by using anatomical landmarks to avoid injury to the tendons and neurovascular structures. The recovery time is shorter than open surgery, but the chance for damage to the digital nerves is higher, especially to digits 1, 2, and 5. A new technique using ultrasound-guided helps identify the tendons and neurovascular structures, preventing potential complications with a non-image-guided percutaneous release. It also compares favourably with surgical procedures. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Texas_State_University_EBP_Project]] | [[Category:Conditions]] | ||
[[Category:Hand - Conditions]] | |||
[[Category:Hand - Conditions]] | |||
[[Category:Hand]] | |||
[[Category:Tendons]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Texas_State_University_EBP_Project]] | |||
[[Category:Primary Contact]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Revision as of 18:25, 9 January 2024
Original and Lead Editors - Holly Pulket, Hilary Zachary, Angela Dempski, Dana Williams, Shannon Davis as part of the Texas State University's Evidence-based Practice project space
Top Contributors - Angela Dempski, Shannon Davis, Dana Williams, Holly Pulket, Hilary Zachary, Kim Jackson, Mariam Hashem, Jess Bell, Candace Goh, Shaimaa Eldib, Tarina van der Stockt, Evan Thomas, Deconinck Mathieu, Fasuba Ayobami, Ewa Jaraczewska, 127.0.0.1, Vidya Acharya, Admin, Rachael Lowe, Claire Knott, Amanda Ager, Lucinda hampton, Anas Mohamed, Stuart Wildman and WikiSysop
Introduction[edit | edit source]
Each hand digit can move freely throughout a full range of motion (ROM) into flexion and extension.
The efficiency, fluidity, and forcefulness of such movements are made possible by several "pulleys" on the digit of the hand. These pulley systems comprise a series of retinacular-type structures that are either annular or cruciform.[1] There are five annular pulleys (A1-A5) and three cruciform pulleys (C1-C3).
Trigger finger is thought to be caused by inflammation and subsequent narrowing of the A1 pulley of the affected digit, typically the third or fourth. The A1 pulley is most often affected, but there are some reported cases where the A2 and A3 pulleys were involved [1]. It can also occur in the thumb and is then called trigger thumb.[2] A difference in size between the flexor tendon sheath and the flexor tendons may lead to abnormalities of the gliding mechanism by causing actual abrasion between the two surfaces, resulting in progressive inflammation between the tendons and the sheath.[3]
Commonly, the trigger finger is referred to as "stenosing tenosynovitis". However, histologic studies have shown that the inflammation occurs more so in the tendon sheaths rather than the tendosynovium, making this name a false depiction of the actual pathophysiology of the condition.[1]
Epidemiology/Aetiology[edit | edit source]
Statistically, trigger finger is more likely to develop in the fifth or sixth decade of life and women are up to six times more likely to develop trigger finger than men.[1][3] The average age is 58 years[4]. The chance of developing a trigger finger is 2-3%, but in the diabetic population, it rises to 10%.[5] This is not due to glycemic control but rather due to the duration of the disease. Trigger finger can concomitantly occur in patients with:
- Carpal Tunnel Syndrome
- DeQuervain's disease
- Hypothyroidism
- Rheumatoid arthritis
- Renal disease
- Amyloidosis[1]
There have been many potential causes of trigger finger discussed throughout the literature. However, there is little to no evidence of precise aetiology.
- Occupational-related causes of the trigger finger have been proposed. Still, the research linking the two is very inconsistent[1][3]
- Authors suggest that trigger finger can manifest from any activity requiring prolonged forceful finger flexion (i.e. carrying shopping bags or a briefcase, prolonged writing, rock climbing, or the strenuous grasping of small tools or objects with sharp edges[4]).[1][3][6]
- It is essential to consider that the cause of the trigger finger is often multi-factorial.
- The condition could develop idiopathically or secondary to other pathologies. [4]
Clinical Presentation[edit | edit source]
The trigger finger has a range of clinical presentations. Initially, patients may present with painless clicking during the movement of the digit. This can progress to painful catching or popping, typically at the metacarpophalangeal (MCP) or proximal interphalangeal (PIP) joints.
Possible additional symptoms are:
- Stiffness and swelling (especially in the morning)
- Intermittent finger locking during active flexion that requires a passive force to extend the finger[4]
- Finger locking or clicking in a bent position, then popping straight
- Loss of full flexion/extension
- Palpable painful nodule proximal to A1, and / or finger locked into a flexed position[1]
- Slight thickening at the base of the digit and pain that may radiate to the palm or to the distal aspect of the digit[7]
Differential Diagnosis[edit | edit source]
The main characteristic of the trigger finger is popping and/or catching with the movement of the digit. However, this characteristic is not unique to just the trigger finger. Other aetiologies associated with a locking digit include:[1]
- Dupuytren's contracture.[6]
- Focal dystonia.
- Flexor tendon/sheath tumour.
- Sesamoid bone anomalies.
- Post-traumatic tendon entrapment on the metacarpal head.
Complaints of pain at the MCP joint could be associated with any of the following:[1]
- DeQuervain's (for trigger thumb only)
- Ulnar collateral ligament injury / Gamekeeper's thumb[6]
- MCP joint sprain
- Extensor apparatus injury
- MCP joint osteoarthritis[6]
Diagnosis of the trigger finger is based on the patient's signs and symptoms.
- Ultrasound is used to measure the affected sheath's thickness and compare it with an unaffected sheath. The degree of thickening seen on ultrasound is correlated with symptom severity.[8] Injection of lidocaine into the flexor sheath to relieve the pain and allow joint movement, can also help in the diagnosis.[1]
Read these documents on differential diagnosis:
- Trigger Digits: Principles, Management, and Complications
- Disorders of the Hand: A Case Study Approach
Outcome Measures[edit | edit source]
- Numeric Pain Rating Scale
- Grip Strength (Jamar dynameter)[7]
- DASH Outcome Measure
- Stages of Stenosing Tenosynovitis (SST)[7]
- 1 = Normal
- 2 = A painful palpable nodule
- 3 = Triggering
- 4 = The proximal interphalangeal (PIP) joint locks into flexion and is unlocked with active PIP joint extension
- 5 = The PIP joint locks and is unlocked with a passive PIP joint extension
- 6 = The PIP joint remains locked in a flexed position
- Participant Perceived Improvement in Symptoms Rating Scale[7]
- 1 = Resolved
- 2 = Improved, but not completely resolved
- 3 = Not resolved
- 4 = Resolved but triggering at the distal interphalangeal/proximal interphalangeal joint(s)
- 5 = Resolved at ten weeks versus six weeks
- Open & Close Hand 10 Times[7] - Patient is to actively make ten fists. The number of triggering events in ten active full fists is then scored out of 10. If the patient’s finger remains locked at any time, the test is completed, and an automatic score of 10/10 is recorded[7]
Examination[edit | edit source]
History[edit | edit source]
Ask the patient-specific questions to understand more about the nature of their symptoms that would help you in the diagnosis of their condition, such as:
- Recent trauma[1]
- Job-related repetitive movements
- Locking or snapping while flexing or extending the affected digit[9]
- Radiating pain to the palm or digits[9]
Past Medical History[edit | edit source]
- Diabetic individuals are four times more likely to develop trigger finger[9]
- Disorders which cause connective tissue changes such as RA and Gout are also associated with trigger finger[7]
Observation[edit | edit source]
- A digit locked in flexion
- Bony proliferative changes in the sub-adjacent PIP joint[10]
Palpation[edit | edit source]
- Painful nodule in the palmar MCP secondary to intratendinous swelling[1]
Range of Movement[edit | edit source]
- Loss of motion, particularly in extension
Manual Muscle Testing[edit | edit source]
- Flexor Digitorum Profundus
- Flexor Digitorum Superficialis
- Grip strength using the Jamar Dynameter[7]
Note: If the finger is locked, testing may not be possible.
Joint Accessory Mobility[edit | edit source]
- PIP, MCP, Distal interphalangeal (DIP) joint, and carpometacarpal (CMC) joint of all affected digits[1]
- Surrounding tissues
- Wrist joint
Special Tests[edit | edit source]
Management[edit | edit source]
The chronic symptoms associated with trigger fingers make conservative treatment difficult and often frustrating. Still, conservative care (listed below in Physical Therapy Management) is always recommended as a treatment plan before surgical intervention.[10]
Non-operative Management[edit | edit source]
Corticosteroid Injection[edit | edit source]
Corticosteroid use is effective in reducing pain and frequency of triggering. Different types of steroids can be injected into the affected tendon: triamcinolone, dexamethasone or methylprednisolone and their choice can significantly affect the clinical outcome: [11]
- triamcinolone: patients required additional injections
- methylprednisolone: patients had surgical release performed earlier and more frequently.
The goal of the injection is to reduce the inflammation and pressure on the tendon for better gliding through the flexor pulleys. Application by a primary care provider can be an effective and safe alternative to surgical therapy. Patient satisfaction, safety, and functional improvement are characteristics of steroidal injections compared to surgical treatment.[12] Surgery is associated with higher costs, long absence from work, and possible surgical complications. Studies have also shown that the combination of corticosteroid injections with lidocaine is significantly more effective than lidocaine alone.[13]
Possible Side effects[12]
- Flaring at the injection site
- Local infections
- Tendon ruptures
- Allergic reactions
- Atrophy of subcutaneous fat tissue
Contraindications[12]
- Under 18 years old
- Any prior treatment or surgery to the area within the last six months
- Possible traumatic or neoplastic origin of symptoms
Physical Therapy Management[edit | edit source]
As with all upper extremity disorders, proximal segments must be screened. Also, because posture can contribute to distal problems, it should be addressed to provide the patient with optimal outcomes.[14]
Patient Education
Since the trigger finger is an overuse injury, education is critical. Education should be given on:
Splinting
The first step in treatment is to stop doing activities that aggravate the condition. Splinting is one of the best ways to limit motion. Most authors agree that splinting intends to alter the biomechanics of the flexor tendons while encouraging maximal differential tendon glide. However, authors disagree on which joints to include in the splint and the degree of joint positioning.[7] There are various ways to splint a patient, but, ultimately, it will depend on what provides the patient with the most relief. Splints are usually worn for 6-10 weeks[16]. Some authors recommended positioning the MCP joint at 0 degrees and allowing full DIP joint movement[4]. It should be noted that splinting yields lower success rates in patients with severe triggering or longstanding duration of symptoms.[1]
Two major types of splinting most recently studied:
- Splinting at the DIP joint. This showed to have a resolution in 50% of the patient’s symptoms[1]
- Splinting at the MCP joint with 15 degrees of flexion. This showed a resolution of the patient’s symptoms of 92.9%.[7]
- Night splinting of the affected finger for 6 to 9 weeks has been shown to augment the patient's compliance over continuous splinting. 55% of patients with grade 1 and 2 Trigger Finger demonstrated the resolution of symptoms for less than three months when wearing a night splint for six weeks.[17]
Exercises
Three exercises are recommended in the management of trigger fingers particularly following surgical release[4]:
- Digit blocking: patient blocks the MCP joint and allows the PIP joints to bend. This exercise could be done with all fingers simultaneously or individually. The same activity could be repeated at the DIP joint. Repetition and frequency are advised according to the level of stiffness and pain
- Tendon gliding: check the video below for the sequence of movement
- Active range of motion: Finger abduction and adduction are recommended to strengthen the interossei and the lumbricals
Other modalities
Modalities such as heat/ice, ultrasound, electric stimulation, massage, stretching, and joint motion (active and passive) can have some positive effects on the trigger finger. It is thought that heat can help by providing increased blood flow and extensibility to the tendon. Stretching after applying heat can provide more extensibility with plastic deformation. Joint movement and mobilisations increase joint and soft tissue mobility via slow, passive therapeutic traction and translational gliding.[15][19]
Although the evidence is lacking, some documented cases and studies of improvement with various combinations of these techniques exist:
- 74 patients were treated with ten sessions of wax therapy, ultrasound, stretching muscle exercises and massage. At three months, 68.8 per cent of patients reported no pain or triggering. Of this 68.8 per cent of patients, none had pain or triggering at six months[15]
- 60 trigger thumbs in 48 children were treated daily with passive exercises of their affected thumb by their mother. This resulted in a cure rate of 80 per cent for stage 2 and 25 per cent for stage 3 thumbs after an average of 62 months[20]
Extracorporeal Shockwave Therapy
Recently, extracorporeal shock wave therapy (ESWT) has been advanced as a possible alternative to surgery for treating musculoskeletal disorders in patients recalcitrant to traditional conservative treatment.
Yildirim and colleagues carried out a prospective randomized controlled clinical trial to determine the efficacy of ESWT in the treatment of trigger finger versus corticosteroid injection.[21] Patients were followed up at one, three and six months. They found that three sessions of ESWT treatment could be as effective as a corticosteroid injection for improving symptom severity and functional status in patients with a grade 2, according to the Quinnell classification. For three sessions, patients in the ESWT group received 1000 shocks at an energy flux density of 2.1 bar (frequency 15 Hz). There was a one-week break between each session.[21] They found that ESWT and corticosteroid groups statistically significantly improved all outcomes after treatment.[21]
It is believed that ESWT induces the repair of inflamed tissues by tissue regeneration and stimulates nitric oxide synthase, leading to the suppression of ongoing inflammation in the soft tissues. There is also mild evidence that one of these mechanisms may benefit the thickening of the flexor tendon and its sheath. This may enable the obstruction in the trigger finger to be overcome.[22] Vahdatpour et al. [23] suggests that extracorporeal shock wave therapy can help with pain reduction, the severity of triggering, and the functional impact of triggering, lasting until the 18th week after the intervention. [23]
In general, it is recommended to use extracorporeal shock wave therapy in terms of a non-invasive intervention with no significant complications for patients with trigger finger.ESWT offers an alternative for people who reject corticosteroid injections because of potential complications, who are allergic to local anaesthetics or who have an intense fear of injections ('needle phobia').[24]
Operative Management[edit | edit source]
Open Surgical Technique[edit | edit source]
When conservative treatment fails, surgery is indicated.[2] Open surgery combined with effective rehabilitation allows a rapid and significant improvement in hand function with a low complication risk.[2] This technique, considered to be the gold standard,[25] is performed by making a longitudinal incision in the palmar crease over the metacarpophalangeal joint of the involved digit and followed by the release of the flexor digitorum superficialis and profundus tendons. This procedure lasts 2-7 minutes and has an average time of discomfort (45 days) post-op. An advantage to this technique is that it allows the pulley to be visualised and therefore has less risk of damage to the digital nerves than endoscopic techniques.
Endoscopic Surgical Technique[edit | edit source]
This technique is performed by making two incisions: one at the palmar crease over the metacarpophalangeal and the other at the volar crease of the finger. An endoscope is then introduced to cut the pulley releasing the flexor tendons. This procedure lasts two to nine minutes and has a shorter average time of discomfort (23 days) post-op. Other advantages are the absence of scars and scar-related problems and shorter post-op rehabilitation.
The endoscopic release offers complete visualization while minimizing soft tissue damage and incomplete or excessive release. [26] However, the popularity of this technique is limited due to a steep learning curve and the cost of the instruments.[27]
Percutaneous Release[edit | edit source]
This technique can be performed with or without imaging. Non-image-guided (blind) percutaneous release is performed by using anatomical landmarks to avoid injury to the tendons and neurovascular structures. The recovery time is shorter than open surgery, but the chance for damage to the digital nerves is higher, especially to digits 1, 2, and 5. A new technique using ultrasound-guided helps identify the tendons and neurovascular structures, preventing potential complications with a non-image-guided percutaneous release. It also compares favourably with surgical procedures.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Makkouk AH, Oetgen ME, Swigart CR, Dodds SD. Trigger finger: aetiology, evaluation, and treatment. Current Reviews in Musculoskeletal Medicine. 2008 Jun 1;1(2):92-6.
- ↑ 2.0 2.1 2.2 Deskur A, Deskur Z. Surgical Treatment and Rehabilitation of Trigger Thumb and Finger. Central European Journal of Sport Sciences and Medicine. 2017;17(1):61-6.
- ↑ 3.0 3.1 3.2 3.3 Andreu JL, Oton T, Silvia-Fernandez L, Sanz J. Hand pain other than carpal tunnel syndrome (CTS): The role of occupational factors. Best Practice and Research Clinical Rheumatology. 2011;25:31–42.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Szmiga L. Trigger Finger. Plus Course 2020
- ↑ Bianchi S, Gitto S, Draghi F. Ultrasound Features of Trigger Finger: Review of the Literature. Journal of Ultrasound in Medicine. 2019 Dec;38(12):3141-54.
- ↑ 6.0 6.1 6.2 6.3 Schöffl VR, Schöffl I. Finger pain in rock climbers: reaching the right differential diagnosis and therapy. J Sports Med Phys Fitness. 2007;47:70-78.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Colbourn J, Heath N, Manary S, Pacifico D. Effectiveness of splinting for the treatment of trigger finger. Journal of Hand Therapy.2008; 21(4):36-343.
- ↑ Matthews A, Smith K, Read L, Nicholas J, Schmidt E. Trigger finger: An overview of the treatment options. Journal of the American Academy of PAs. 2019 Jan 1;32(1):17-21.
- ↑ 9.0 9.1 9.2 Tendon trouble in hand: de Quervain's tenosynovitis and trigger finger. Harvard Women's Health Watch.2010:4-5.
- ↑ 10.0 10.1 Howitt S. The conservative treatment of trigger thumb using Graston techniques and active release technique. JCCA. 206;50(4):249-254.
- ↑ Roberts JM, Behar BJ, Siddique LM, Brgoch MS, Taylor KF. Choice of corticosteroid solution and outcome after injection for trigger finger. Hand. 2021 May;16(3):321-5.
- ↑ 12.0 12.1 12.2 Peters-Veluthamaningal C, Winters JC, Groenier KH et al. Corticosteroid injections effective for trigger finger in adults in general practice: a double-blinded randomised placebo-controlled trial. Annals of the Rheumatic Diseases. 2008;67;1262-1266.
- ↑ Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for adult trigger finger. Cochrane Database Syst Rev. 2009; (1): CD005617.
- ↑ Yung E, Asavasopon S, Godges J. Screening for the head, neck, and shoulder pathology in patients with upper extremity signs and symptoms. Journal Of Hand Therapy [serial online]. April 2010;23(2):173-186. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed November 23, 2011.
- ↑ 15.0 15.1 15.2 Salim, N., S. Abdullah, J. Sapuan, and N. H. M. Haflah.The outcome of corticosteroid injection versus physiotherapy in treating mild trigger fingers. Journal of Hand Surgery (European Volume) 0th ser. 0.0 (2011): 1-8. November 19, 2011.
- ↑ Lunsford D, Valdes K, Hengy S. Conservative management of trigger finger: A systematic review. Journal of Hand Therapy. 2019 Apr 1;32(2):212-21.
- ↑ Merry SP, O’Grady JS, Boswell CL. Trigger finger? Just shoot!. Journal of Primary Care & Community Health. 2020 Jul;11:2150132720943345.
- ↑ Tendon Glide Exercises | Ability Rehabilitation . Available from:https://www.youtube.com/watch?v=favZefGkiHk[last accessed 2/12/2020]
- ↑ Ferrara PE, Codazza S, Maccauro G, Zirio G, Ferriero G, Ronconi G. Physical therapies for the conservative treatment of the trigger finger: a narrative review. Orthop Rev (Pavia). 2020 Jun 26;12(Suppl 1):8680.
- ↑ Watanabe, H., Yoshiki Hamada, Tadahito Toshima, and Koki Nagasawa. Conservative treatment for trigger thumb in children. Archives of Orthopaedic and Trauma Surgery. 2001;121(7):388-90.
- ↑ 21.0 21.1 21.2 Yildirim P, Gultekin A, Yildirim A, Karahan AY, Tok F. Extracorporeal shock wave therapy versus corticosteroid injection in the treatment of trigger finger: a randomized controlled study. J Hand Surg Eur Vol. 2016 Nov;41(9):977-983.
- ↑ Seok H, Kim SH. The effectiveness of extracorporeal shock wave therapy vs. local steroid injection for management of carpal tunnel syndrome: a randomized controlled trial. Am J Phys Med Rehabil. 2013 Apr;92(4):327-34.
- ↑ 23.0 23.1 Vahdatpour B, Momeni F, Tahmasebi A, Taheri P. The Effect of Extracorporeal Shock Wave Therapy in the Treatment of Patients with Trigger Finger. Open Access J Sports Med. 2020 Mar 9;11:85-91.
- ↑ Akhtar S, Bradley MJ, Quinton DN, Burke FD. Management and referral for trigger finger/thumb. BMJ. 2005 Jul 2;331(7507):30-3.
- ↑ Rajeswaran G., Lee J.C., Eckersley R., et al. Ultrasound-guided percutaneous release of the annular pulley in trigger digit. European Society of Radiology. 2009;19:2232-2237.
- ↑ Brown AM, DellaMaggiora RJ, Tsai EY, Kulber DA. Endoscopic Retrograde Approach for Trigger Finger Release: A Cadaver Study. Plast Reconstr Surg Glob Open. 2020 Dec 21;8(12):e3294.
- ↑ Pegoli L, Cavalli E, Cortese P, Parolo C, Pajardi G. A comparison of endoscopic and open trigger finger release. Hand Surg. 2008;13(3):147-51.