Patellofemoral Joint: Difference between revisions
Elvira Muhic (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (65 intermediate revisions by 14 users not shown) | |||
| Line 3: | Line 3: | ||
'''Lead Editors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Lead Editors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Description | |||
== Etiology == | |||
Patellofemoral pain (PFP) is frequent musculoskeletal-related diagnosis with complaints of pain localised to the anterior retripatellar and/or peripatellar area of the knee. Symptoms can be insidious in nature or acutely develop and are worse with lower-limb loading activities (prolonged sitting, squatting, ascending/descending, running or jumping). <ref>Willy, R.W., Hoglund, L.T., Barton, C.J., Bolgla, L.A., Scalzitti, D.A., Logerstedt, D.S., Lynch, A.D., Snyder-Mackler, L., McDonough, C.M., Altman, R. and Beattie, P., 2019. [https://www.jospt.org/doi/10.2519/jospt.2019.0302 Patellofemoral pain: clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association.] ''Journal of Orthopaedic & Sports Physical Therapy'', ''49''(9), pp.CPG1-CPG95.</ref>The specific cause of PFP is not clear.<ref>Shi W, Li Y, Xiong B, Du M. [https://www.frontiersin.org/articles/10.3389/fpubh.2021.643191/full Diagnosis of Patellofemoral Pain Syndrome Based on a Multi-Input Convolutional Neural Network With Data Augmentation]. Frontiers in Public Health. 2021 Feb 11;9:643191.</ref>PFP is thought to precede patellofemoral oseoarthritis (OA).<ref>Hart, H.F., Patterson, B.E., Crossley, K.M., Culvenor, A.G., Khan, M.C., King, M.G. and Sritharan, P., 2022. [https://bjsm.bmj.com/content/56/9/521 May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis.] ''British Journal of Sports Medicine'', ''56''(9), pp.521-530.</ref> | |||
== Description == | |||
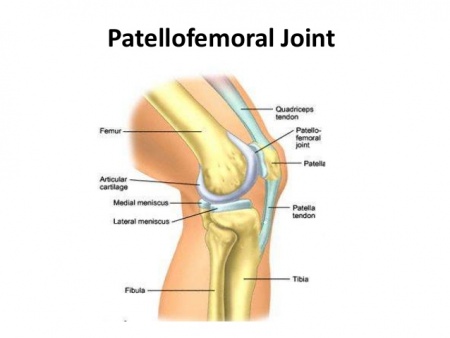
[[Image:PFJ-1-4-20-638.jpg|right|450x400px]] The patellofemoral joint is a unique and complex structure consisting of static elements (bones and ligaments) and dynamic elements (neuromuscular system).<ref name="p2">Kim Y-M, Joo Y-B. Patellofemoral Osteoarthritis. Knee Surgery Related Research. 2012;24(4):193-200. doi:10.5792/ksrr.2012.24.4.193.</ref> The [[Patella|patella]] has a configuration of a triangle with its apex directed inferiorly. Superiorly, it articulates with the trochlea, the distal articulating surface of the [[Femur|femur]], which are the main articulating surfaces of the patellofemoral joint.<ref name="p1">Medscape. Drugs and Diseases. Patellofemoral Joint Syndromes. Available at: http://emedicine.medscape.com/article/90286-overview#showall (accessed 08 august 2016).</ref> | |||
== Anatomy == | == Anatomy == | ||
=== Articulating Surfaces === | === Articulating Surfaces === | ||
'''Patella''' | |||
The patella is a triangular shaped sesamoid bone, the posterior surface of the patella is covered with articular cartilage.<ref name=":0">Neumann DA. Kinesiology of the musculoskeletal system; Foundation for rehabilitation. Mosby & Elsevier. 2010.</ref> | |||
The articular cartilage of the patella is similar to that of other joints in that it contains a solid phase and a fluid phase that is mostly composed of collagen and glycosaminoglycans. The solid phase is somewhat permeable and when the articular surface is under load, the fluid gradually redistributes itself within the solid matrix. Therefore, the pressure within the fluid is strongly associated with the cushioning effect of the articular cartilage and the low friction coefficient of articular surfaces. Any damage to the articular surfaces causes a loss of pressure within the fluid phase, which subsequently results in higher stresses on the collagen fibers and more vulnerability leading to possible breakdown.<ref name="p2" /> | |||
'''Intercondylar groove''' | |||
The patella articulates with the intercondylar groove (trochlear groove). The intercondylar groove lateral facet is more prominent anteriorly and steeper than the medial facet to help stabilize the patella against excessive lateral pull. | |||
=== Ligaments === | |||
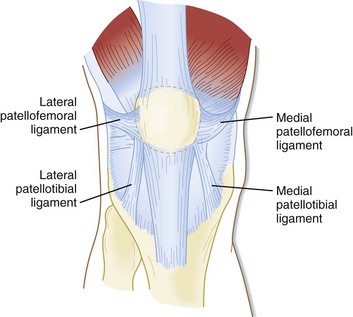
The patellar retinaculum is an important stabilizer of the patellofemoral joint, mainly its medial and lateral components.<ref name="p0">NAVARRO, Marcelo Schmidt et al. Relationship between the lateral patellofemoral ligament and the width of the lateral patellar facet. Acta ortop. bras. [online]. 2010, vol.18, n.1, pp.19-22. ISSN 1413-7852.</ref>[[Image:PFJ-ligaments.jpg|right]] | |||
The | '''The Medial Patellofemoral Ligament (MPFL)''' - originates on the medial femur and has a “sail-shaped” attachment on the patella and quadriceps tendon. Because of its wider attachment than its origin, several authors have promoted the technique of using a double-bundled graft to recreate the anatomy of this complex. Kang and colleagues described two components of MPFL fibers, using the term ''superior-oblique bundle'' and ''inferior-straight bundle''. The clinical significance of this is not yet known, but the authors suggested the bundles may vary in their roles as dynamic versus static stabilizers. Furthermore, length differences between the two bundles or attachment sites, have been described. Mochizuki and colleagues showed the length of the MPFL fibers from the origin to the medial patella was 56.3+/-5.1 mm vs. 70.7+/-4.5 mm to the quadriceps tendon.<ref name="p3">Healio MedBlog. Orthopedics. Business of Orthopedics. BLOG: Update on medial patelofemoral anatomy, implications for reconstruction. Available at: http://www.healio.com/orthopedics/business-of-orthopedics/news/blogs/%7B556829f5-0f97-42a6-9c3f-4f6ffe7aa48e%7D/patellofemoral-update/blog-update-on-medial-patellofemoral-anatomy-implications-for-reconstruction (accesed 10 august 2016).</ref> | ||
= | '''The Lateral Patellofemoral Ligament (LPFL)''' - is an important lateral stabilizer of the patella against medial subluxation or dislocation. Some authors describe the lateral patellofemoral ligament as a palpable thickening of the joint capsule between the patella and femoral epicondyle.<ref name="p9">Borbas P, Koch P, Fucentese S. Lateral Patellofemoral Ligament Reconstruction Using a Free Gracilis Autograft. ORTHOPEDICS. 2014; 37: e665-e668. doi: 10.3928/01477447-20140626-66</ref><br> | ||
=== Muscles === | === Muscles === | ||
The quadriceps muscle is the largest and strongest extensor muscle, consisting of rectus femoris and vastus group (vastus lateralis, vastus intermedius and vastus medialis). | |||
The vastus group produces 80% of the knee extension torque and the rectus femoris produces 20% of the knee extension torque. | |||
The vastus medialis has 2 distinct fiber directions. The vastus medialis longus (VML) attaches at 15 to 18 degrees medial to quadriceps tendon and [[Vastus Medialis Oblique|vastus medialis oblique]] (VMO) attaching at 50 to 55 degrees. The VMO more oblique pull on the patella stabilizes the patella against excessive lateral pull. | |||
Lateral tracking is guided by both the [[Vastus Lateralis|vastus lateralis]] and the iliotibial band. | |||
Patellar motion is further constrained by the patellofemoral ligament, the patellotibial ligament, and the retinaculum.<ref name="p1" /> | |||
{| width="300" border="1" align=" | == Joint Mechanics == | ||
=== Kinematics === | |||
{{#ev:youtube|Q-80Qi5cx9o}}<ref name="p5">Roy Wung. Patellofemoral joint motion and patellar tracking. Available from: https://www.youtube.com/watch?v=Q-80Qi5cx9o (accessed 27 august 2016).</ref> | |||
At full knee extension, the quadriceps muscle is relaxed and the patella is resting on the suprapatellar fat pad. The patella migrates inferiorly as the knee flexes. | |||
At 20-30 degrees of knee flexion the patella moves inferiorly, lying in the shallow part of the intercondylar groove, explaining why lateral patella dislocations occur near this range. The patella contacts the femur with its inferior pole. | |||
At 60-90 degrees knee flexion the patella occupies the intercondylar groove. There is maximum contact between the patella and the intercondylar groove (1/3 of the posterior surface area of the patella). | |||
At 135 degrees of knee flexion (near full knee flexion), the patella contacts the femur with its superior pole and rests below the intercondylar groove.<ref name=":0" /> | |||
=== Kinetics === | |||
<br>The patellofemoral joint is exposed to high compression forces.<ref name=":0" /> | |||
Compression forces at the patellofemoral joint:<ref name="p1" /> | |||
{| class="wikitable sortable" width="300" border="1" align="center" cellpadding="1" cellspacing="1" | |||
|- | |- | ||
! scope="col" | Activity | ! scope="col" | Activity | ||
! scope="col" | Force | ! scope="col" | Force | ||
! scope="col" | %Body Weight | ! scope="col" | %Body Weight | ||
! scope="col" | Pounds of Force | ! scope="col" | Pounds of Force | ||
|- | |- | ||
| Walking | | Walking | ||
| 850 N | | 850 N | ||
| 1/2 x BW | | 1/2 x BW | ||
| 100 Ibs | | 100 Ibs | ||
|- | |- | ||
| Bike | | Bike | ||
| 850 N | | 850 N | ||
| 1/2 x BW | | 1/2 x BW | ||
| 100 Ibs | | 100 Ibs | ||
|- | |- | ||
| Stair Ascend | | Stair Ascend | ||
| 1500 N | | 1500 N | ||
| 3.3 x BW | | 3.3 x BW | ||
| 660 Ibs | | 660 Ibs | ||
|- | |- | ||
| Stair Descend | | Stair Descend | ||
| 4000 N | | 4000 N | ||
| 5 x BW | | 5 x BW | ||
| 1000 Ibs | | 1000 Ibs | ||
|- | |- | ||
| Jogging | | Jogging | ||
| 5000 N | | 5000 N | ||
| 7 x BW | | 7 x BW | ||
| 1400 Ibs | | 1400 Ibs | ||
|- | |- | ||
| Squatting | | Squatting | ||
| 5000 N | | 5000 N | ||
| 7 x BW | | 7 x BW | ||
| 1400 Ibs | | 1400 Ibs | ||
|- | |- | ||
| Deep Squatting | | Deep Squatting | ||
| 15000 | | 15000 | ||
| 20 x BW | | 20 x BW | ||
| 4000 Ibs | | 4000 Ibs | ||
|} | |} | ||
The compression forces of the patellofemoral joint are influenced by the quadriceps muscle force and the knee flexion angle. | |||
The patella acts as a pulley with the quadriceps tendon attaching to it proximally and the patellar tendon attaching to it distally transmitting the forces of the knee extensor mechanism. The resultant of the Quadriceps tendon and patellar tendon forces is directed to the intercondylar groove. | |||
The compression force in the patellofemoral joint increases with increasing knee flexion. This can be explained through the squat exercise, as the person squats deeper the force demand on the quadriceps muscle increases and the angle between the quadriceps tendon and patellar tendon decreases which increase the magnitude of compression force directed to the patella. | |||
At 60-90 degrees of knee flexion there is maximum patellofemoral joint compression forces and also maximum contact area between the patella and the femur, protecting the joint against the high compression forces.<ref name=":0" /> | |||
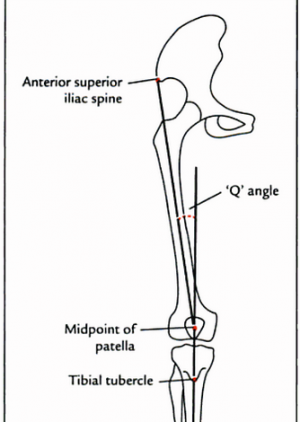
[[File:Q angle 2.png|thumb|Q-angle]] | |||
== Factors affecting lateral tracking of the patella == | |||
When the quadriceps muscle contracts it pulls the patella laterally and posteriorly due to the large cross section area and force potential of the vastus lateralis. The measurement of lateral line of pull of the quadriceps relative to the patella is referred to as [[Q Angle|Q-angle]]. | |||
The Q-angle is formed by 2 lines. One line connecting from the anterior superior iliac spine to the middle of the patella and the other connecting from the middle of the patella to the tibial tuberosity. The average measurement of Q-angle is 13-15. | |||
Also, increased tension in the iliotibial band and lateral patellar retinacular fibers can increase lateral pull on the patella. <ref name=":0" /> | |||
== Factors that oppose the lateral pull of the patella by the Quadriceps == | |||
* The lateral facet of the intercondylar groove is steeper than the media facet, blocking the lateral shift of patella | |||
* The oblique fibers of vastus medialis oblique | |||
* Medial patellofemoral ligament <ref name=":0" /> | |||
== Pathology/Injury == | |||
* [[Patellofemoral Pain Syndrome|Patellofemoral Pain Syndrome]] | |||
* [[Patellar dislocation]] | |||
* [[Patellofemoral Osteoarthritis|Patellofemoral osteoarthritis]] | |||
== Examination == | |||
=== History === | |||
History taking is an essential part of the examination for making a diagnosis.<ref name=":1">Manske RC, Davies GJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5095938/ Examination of the patellofemoral joint. International journal of sports physical therapy.] 2016 Dec;11(6):831.</ref> | |||
=== Physical Examination === | |||
==== Standing ==== | |||
'''Static examination''' | |||
The patient stands barefoot with knees exposed and the two feet slightly apart. First the patient is inspected while standing for symmetry, skin changes, scars, sinuses and soft tissue swelling. | |||
From anterior view, the alignment of the knee is inspected. Genu valgum has increased Q-angle which is associated with lateral patella maltracking and subluxation. The Q-angle should be measured to measure the laterally directed forces across the patella. | |||
The height and the position of the patella should be inspected. A high riding patella (patella alta) is associated with patella sublaxation while a low riding patella (patella baja) is associated with chondromalacia patella. Squinting patella have increased incidence of patellofemoral pain while outfacing patella is associated with habitual sublaxation of the patella. | |||
[[Leg Length Test|Leg Length discrepancy]] assessment can be done by comparing the level of the pelvic on both sides for pelvic tilt. | |||
From side view the knee is inspected for genus recarvatum which may indicate general hyperlaxity, in which the [[beighton score]] is determined. Lack of full knee extension is associated with patellofemoral arthrosis. | |||
The [[Foot and Ankle Assessment-Investigations and Tests|feet posture]] is assessed. Excessive foot pronation is associated with genu valgum and tibia internal rotation.<ref name=":2">Rodríguez-Merchán EC, Liddle AD, editors. [https://books.google.com.eg/books?id=1QiZDwAAQBAJ&pg=PA1&lpg=PA1&dq=examination+of+patellofemoral+joint+luke+jones&source=bl&ots=zbhDSc70Yw&sig=ACfU3U0iBqGFd0iCNNzR-H-YPK_Il5r_vA&hl=en&sa=X&ved=2ahUKEwjWs9TV_t3pAhWk4YUKHSwyBtQQ6AEwDHoECAoQAQ#v=onepage&q=examination%20of%20patellofemoral%20joint%20luke%20jones&f=false Disorders of the Patellofemoral Joint: Diagnosis and Management.] Springer; 2019 May 17.</ref><ref name=":3">Sankineani SR, Karnatzikos G, Chaurasia S, Gobbi A. [https://link.springer.com/chapter/10.1007/978-3-642-54965-6_5 Clinical Examination of the Patellofemoral Joint. InThe Patellofemoral Joint] 2014 (pp. 23-27). Springer, Berlin, Heidelberg.</ref> | |||
'''Dynamic examination''' | |||
The gait examination should be performed ideally barefoot. The patient should be observed anterioly, posteriolrly and laterally. Observe for gait deviations like [[Trendelenburg Gait|trendelenburg gait]], limping gait and quadriceps avoidance gait. Also, the patient is asked to walk on his heels and toes to assess L5 and S1. | |||
= | Next the patient performs double leg squat and any knee malalignments are observed. Knee malalignments can be due to weakness of the quadriceps (especially the vastus medialis), weakness of hip stabilizers (especially the hip abductors and external rotators) and the lack of motor control at the ankle joint. Single leg squat is more sensitive as it imposes higher mechanical demands.<ref name=":2" /> | ||
=== | ==== Sitting ==== | ||
The patient sits in a tripod position with his hands extending backwards to tilt the pelvic posteriorly, decreasing the tension on the hamstrings. | |||
'''Static examination''' | |||
The atrophy of the quadriceps is observed (mainly VMO) and the patella height. | |||
== | The Tubercle Sulcus angle is measured at 90 degrees knee flexion, as at 90 degrees knee flexion the patella is inside the femoral sulcus so the amount of tibial tubercle displacement can be measured in relation to the femoral sulcus. It is measured by drawing a vertical line from the middle of the patella to the tibial tubercle and another vertical line perpendicular to the transpicondylar axis. The normal value for women is less than 8 degrees and less than 5 degrees for men. Increase in the Tubercle Suclus angle is associated with patellofemoral pain and instability.<ref name=":2" /><ref name=":3" /> | ||
'''Dyanamic examination''' | |||
Active and passive range of motion (ROM) are compared to the opposite side. A decrease in the active ROM with full passive extension ROM is known as [[Knee Extension Lag|extension lag]]. A decrease in passive ROM is due to muscles tightness. | |||
Knee creptus during active knee movement is a nonspecific finding, it is found in up to 40% of asymptomatic females and should be considered important when it is new, painful and asymmetrical. | |||
J-sign can be observed by asking the patient to flex and extend his knee to evaluate patellar tracking. J-sign is present when the patella subluxes laterally at terminal knee extension.<ref name=":2" /> | |||
== | ==== Supine ==== | ||
Knee joint effusion is assessed. | |||
The knee is palpated in a systemic manner with the knee flexed 90 degrees palpate the quadriceps tendon, patella, patellar tendon and tibial tuberosity. Next, the medial and lateral fat pads are palpated, medial and lateral retinaculm, medial patekka plica and medial and lateral borders of the patella. | |||
Screening should also be done for knee ligaments, meniscus and other pathological states not related to the extensor mechanism as [[Pes Anserinus Bursitis|pes anserinus bursitis]] and iliotibial band tendinopathy.<ref name=":2" /> | |||
==== Special Tests ==== | |||
'''Patella glide test''' | |||
The patella glide test or apprehension test, tests the integrity of the medial and lateral patella restraints. The test is performed at full knee extension to assess soft tissue restraints only then at 20 degrees knee flexion to assess both bony and soft tissue stability. | |||
The therapist grasps the patella and glides it medially and laterally. The test is positive when there is a sense of dislocation at lateral translation.<ref name=":2" /> | |||
'''The moving patella apprehension test''' | |||
The [[Moving Patellar Apprehension Test|moving patella apprehension test]], tests for lateral patella stability. | |||
The patient is supine and the therapist laterally translates the patella by his thumb then the therapist flexes the knee to 90 degrees then extends it, the test is positive if there are any symptoms indicating lateral patellar instability. The second portion of the test, the therapist translates the patella medially while performing the same steps if there are no symptoms then there is lateral knee instability.<ref name=":1" /> | |||
'''Patella tilt test''' | |||
Tests patella hypomobilty due to contracture in the lateral deep retinaculum, which is contributed by tightness in the ITB, lateral patellofemoral and patelotibial ligaments. | |||
The knee is extended and the therapist pushes the patellar medial surface posteriorly and the lateral surface anteriorly. The patella should tilt 15 degrees on medial and lateral side and should be compared to the uninvolved side.<ref name=":1" /> | |||
'''Compression test''' | |||
Tests for patellofemoral joint degeneration. | |||
The | The patella is compressed as the patient flexes his knee. A positive test is an increase of patient's knee pain. <ref name=":2" /> | ||
'''Clarke’s test''' | |||
Clarke’s test or Patellar grind test, tests for chondromalacia patella. | |||
= | The therapist compresses the patient’s patella into the trochlear while the patient contracts the quadriceps. A positive test is reproduction of the symptoms. However, It is not recommended to be used as it increases the patient’s condition and has high false-positive results.<ref name=":2" /> | ||
Muscles strength should be assessed for the lower limb muscles. | |||
The muscles flexibility is assessed for the hamstrings by the popliteal angle, [[Thomas Test|Thomas test]] for the rectus femoris and iliopsoas and [[Ober's Test|ober’s test]] for the iliotibial band. | |||
= | Finally, the examination is finished when an evaluation of the lumbar, hip and ankle is complete. The neurovascular assessment of the limb is also made. <ref name=":2" /> | ||
== | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |||
| {{#ev:youtube|LgBNuWQMSC8|300}}<ref name="p8">Jason Craig. Examination of the Patellofemoral Joint - Palpation. Available from: https://www.youtube.com/watch?v=LgBNuWQMSC8 (accessed 27 august 2016).</ref> | |||
| {{#ev:youtube|we9COmZ-cig|300}}<ref name="p7">Jason Craig. Patellofemoral Joint Examination - Observations. Available from: https://www.youtube.com/watch?v=we9COmZ-cig (accessed 27 august 2016).</ref> | |||
|} | |||
== References == | == References == | ||
<references /> | |||
[[Category:Anatomy]] | |||
[[Category:Joints]] | |||
[[Category:Knee]] | |||
[[Category:Biomechanics]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Knee - Anatomy]] | |||
[[Category:Knee - Joints]] | |||
Latest revision as of 12:14, 20 November 2023
Original Editor - Elvira Muhic
Lead Editors - Elvira Muhic, Kim Jackson, Lilian Ashraf, WikiSysop, Ahmed Essam, 127.0.0.1, Admin, Rachael Lowe, Evan Thomas, Michelle Lee, Vidya Acharya, Rucha Gadgil, Jess Bell and Robin Tacchetti
Etiology[edit | edit source]
Patellofemoral pain (PFP) is frequent musculoskeletal-related diagnosis with complaints of pain localised to the anterior retripatellar and/or peripatellar area of the knee. Symptoms can be insidious in nature or acutely develop and are worse with lower-limb loading activities (prolonged sitting, squatting, ascending/descending, running or jumping). [1]The specific cause of PFP is not clear.[2]PFP is thought to precede patellofemoral oseoarthritis (OA).[3]
Description[edit | edit source]
The patellofemoral joint is a unique and complex structure consisting of static elements (bones and ligaments) and dynamic elements (neuromuscular system).[4] The patella has a configuration of a triangle with its apex directed inferiorly. Superiorly, it articulates with the trochlea, the distal articulating surface of the femur, which are the main articulating surfaces of the patellofemoral joint.[5]
Anatomy[edit | edit source]
Articulating Surfaces[edit | edit source]
Patella
The patella is a triangular shaped sesamoid bone, the posterior surface of the patella is covered with articular cartilage.[6]
The articular cartilage of the patella is similar to that of other joints in that it contains a solid phase and a fluid phase that is mostly composed of collagen and glycosaminoglycans. The solid phase is somewhat permeable and when the articular surface is under load, the fluid gradually redistributes itself within the solid matrix. Therefore, the pressure within the fluid is strongly associated with the cushioning effect of the articular cartilage and the low friction coefficient of articular surfaces. Any damage to the articular surfaces causes a loss of pressure within the fluid phase, which subsequently results in higher stresses on the collagen fibers and more vulnerability leading to possible breakdown.[4]
Intercondylar groove
The patella articulates with the intercondylar groove (trochlear groove). The intercondylar groove lateral facet is more prominent anteriorly and steeper than the medial facet to help stabilize the patella against excessive lateral pull.
Ligaments[edit | edit source]
The patellar retinaculum is an important stabilizer of the patellofemoral joint, mainly its medial and lateral components.[7]
The Medial Patellofemoral Ligament (MPFL) - originates on the medial femur and has a “sail-shaped” attachment on the patella and quadriceps tendon. Because of its wider attachment than its origin, several authors have promoted the technique of using a double-bundled graft to recreate the anatomy of this complex. Kang and colleagues described two components of MPFL fibers, using the term superior-oblique bundle and inferior-straight bundle. The clinical significance of this is not yet known, but the authors suggested the bundles may vary in their roles as dynamic versus static stabilizers. Furthermore, length differences between the two bundles or attachment sites, have been described. Mochizuki and colleagues showed the length of the MPFL fibers from the origin to the medial patella was 56.3+/-5.1 mm vs. 70.7+/-4.5 mm to the quadriceps tendon.[8]
The Lateral Patellofemoral Ligament (LPFL) - is an important lateral stabilizer of the patella against medial subluxation or dislocation. Some authors describe the lateral patellofemoral ligament as a palpable thickening of the joint capsule between the patella and femoral epicondyle.[9]
Muscles[edit | edit source]
The quadriceps muscle is the largest and strongest extensor muscle, consisting of rectus femoris and vastus group (vastus lateralis, vastus intermedius and vastus medialis).
The vastus group produces 80% of the knee extension torque and the rectus femoris produces 20% of the knee extension torque.
The vastus medialis has 2 distinct fiber directions. The vastus medialis longus (VML) attaches at 15 to 18 degrees medial to quadriceps tendon and vastus medialis oblique (VMO) attaching at 50 to 55 degrees. The VMO more oblique pull on the patella stabilizes the patella against excessive lateral pull.
Lateral tracking is guided by both the vastus lateralis and the iliotibial band.
Patellar motion is further constrained by the patellofemoral ligament, the patellotibial ligament, and the retinaculum.[5]
Joint Mechanics[edit | edit source]
Kinematics[edit | edit source]
At full knee extension, the quadriceps muscle is relaxed and the patella is resting on the suprapatellar fat pad. The patella migrates inferiorly as the knee flexes.
At 20-30 degrees of knee flexion the patella moves inferiorly, lying in the shallow part of the intercondylar groove, explaining why lateral patella dislocations occur near this range. The patella contacts the femur with its inferior pole.
At 60-90 degrees knee flexion the patella occupies the intercondylar groove. There is maximum contact between the patella and the intercondylar groove (1/3 of the posterior surface area of the patella).
At 135 degrees of knee flexion (near full knee flexion), the patella contacts the femur with its superior pole and rests below the intercondylar groove.[6]
Kinetics[edit | edit source]
The patellofemoral joint is exposed to high compression forces.[6]
Compression forces at the patellofemoral joint:[5]
| Activity | Force | %Body Weight | Pounds of Force |
|---|---|---|---|
| Walking | 850 N | 1/2 x BW | 100 Ibs |
| Bike | 850 N | 1/2 x BW | 100 Ibs |
| Stair Ascend | 1500 N | 3.3 x BW | 660 Ibs |
| Stair Descend | 4000 N | 5 x BW | 1000 Ibs |
| Jogging | 5000 N | 7 x BW | 1400 Ibs |
| Squatting | 5000 N | 7 x BW | 1400 Ibs |
| Deep Squatting | 15000 | 20 x BW | 4000 Ibs |
The compression forces of the patellofemoral joint are influenced by the quadriceps muscle force and the knee flexion angle.
The patella acts as a pulley with the quadriceps tendon attaching to it proximally and the patellar tendon attaching to it distally transmitting the forces of the knee extensor mechanism. The resultant of the Quadriceps tendon and patellar tendon forces is directed to the intercondylar groove.
The compression force in the patellofemoral joint increases with increasing knee flexion. This can be explained through the squat exercise, as the person squats deeper the force demand on the quadriceps muscle increases and the angle between the quadriceps tendon and patellar tendon decreases which increase the magnitude of compression force directed to the patella.
At 60-90 degrees of knee flexion there is maximum patellofemoral joint compression forces and also maximum contact area between the patella and the femur, protecting the joint against the high compression forces.[6]
Factors affecting lateral tracking of the patella[edit | edit source]
When the quadriceps muscle contracts it pulls the patella laterally and posteriorly due to the large cross section area and force potential of the vastus lateralis. The measurement of lateral line of pull of the quadriceps relative to the patella is referred to as Q-angle.
The Q-angle is formed by 2 lines. One line connecting from the anterior superior iliac spine to the middle of the patella and the other connecting from the middle of the patella to the tibial tuberosity. The average measurement of Q-angle is 13-15.
Also, increased tension in the iliotibial band and lateral patellar retinacular fibers can increase lateral pull on the patella. [6]
Factors that oppose the lateral pull of the patella by the Quadriceps[edit | edit source]
- The lateral facet of the intercondylar groove is steeper than the media facet, blocking the lateral shift of patella
- The oblique fibers of vastus medialis oblique
- Medial patellofemoral ligament [6]
Pathology/Injury[edit | edit source]
Examination[edit | edit source]
History[edit | edit source]
History taking is an essential part of the examination for making a diagnosis.[11]
Physical Examination[edit | edit source]
Standing[edit | edit source]
Static examination
The patient stands barefoot with knees exposed and the two feet slightly apart. First the patient is inspected while standing for symmetry, skin changes, scars, sinuses and soft tissue swelling.
From anterior view, the alignment of the knee is inspected. Genu valgum has increased Q-angle which is associated with lateral patella maltracking and subluxation. The Q-angle should be measured to measure the laterally directed forces across the patella.
The height and the position of the patella should be inspected. A high riding patella (patella alta) is associated with patella sublaxation while a low riding patella (patella baja) is associated with chondromalacia patella. Squinting patella have increased incidence of patellofemoral pain while outfacing patella is associated with habitual sublaxation of the patella.
Leg Length discrepancy assessment can be done by comparing the level of the pelvic on both sides for pelvic tilt.
From side view the knee is inspected for genus recarvatum which may indicate general hyperlaxity, in which the beighton score is determined. Lack of full knee extension is associated with patellofemoral arthrosis.
The feet posture is assessed. Excessive foot pronation is associated with genu valgum and tibia internal rotation.[12][13]
Dynamic examination
The gait examination should be performed ideally barefoot. The patient should be observed anterioly, posteriolrly and laterally. Observe for gait deviations like trendelenburg gait, limping gait and quadriceps avoidance gait. Also, the patient is asked to walk on his heels and toes to assess L5 and S1.
Next the patient performs double leg squat and any knee malalignments are observed. Knee malalignments can be due to weakness of the quadriceps (especially the vastus medialis), weakness of hip stabilizers (especially the hip abductors and external rotators) and the lack of motor control at the ankle joint. Single leg squat is more sensitive as it imposes higher mechanical demands.[12]
Sitting[edit | edit source]
The patient sits in a tripod position with his hands extending backwards to tilt the pelvic posteriorly, decreasing the tension on the hamstrings.
Static examination
The atrophy of the quadriceps is observed (mainly VMO) and the patella height.
The Tubercle Sulcus angle is measured at 90 degrees knee flexion, as at 90 degrees knee flexion the patella is inside the femoral sulcus so the amount of tibial tubercle displacement can be measured in relation to the femoral sulcus. It is measured by drawing a vertical line from the middle of the patella to the tibial tubercle and another vertical line perpendicular to the transpicondylar axis. The normal value for women is less than 8 degrees and less than 5 degrees for men. Increase in the Tubercle Suclus angle is associated with patellofemoral pain and instability.[12][13]
Dyanamic examination
Active and passive range of motion (ROM) are compared to the opposite side. A decrease in the active ROM with full passive extension ROM is known as extension lag. A decrease in passive ROM is due to muscles tightness.
Knee creptus during active knee movement is a nonspecific finding, it is found in up to 40% of asymptomatic females and should be considered important when it is new, painful and asymmetrical.
J-sign can be observed by asking the patient to flex and extend his knee to evaluate patellar tracking. J-sign is present when the patella subluxes laterally at terminal knee extension.[12]
Supine[edit | edit source]
Knee joint effusion is assessed.
The knee is palpated in a systemic manner with the knee flexed 90 degrees palpate the quadriceps tendon, patella, patellar tendon and tibial tuberosity. Next, the medial and lateral fat pads are palpated, medial and lateral retinaculm, medial patekka plica and medial and lateral borders of the patella.
Screening should also be done for knee ligaments, meniscus and other pathological states not related to the extensor mechanism as pes anserinus bursitis and iliotibial band tendinopathy.[12]
Special Tests[edit | edit source]
Patella glide test
The patella glide test or apprehension test, tests the integrity of the medial and lateral patella restraints. The test is performed at full knee extension to assess soft tissue restraints only then at 20 degrees knee flexion to assess both bony and soft tissue stability.
The therapist grasps the patella and glides it medially and laterally. The test is positive when there is a sense of dislocation at lateral translation.[12]
The moving patella apprehension test
The moving patella apprehension test, tests for lateral patella stability.
The patient is supine and the therapist laterally translates the patella by his thumb then the therapist flexes the knee to 90 degrees then extends it, the test is positive if there are any symptoms indicating lateral patellar instability. The second portion of the test, the therapist translates the patella medially while performing the same steps if there are no symptoms then there is lateral knee instability.[11]
Patella tilt test
Tests patella hypomobilty due to contracture in the lateral deep retinaculum, which is contributed by tightness in the ITB, lateral patellofemoral and patelotibial ligaments.
The knee is extended and the therapist pushes the patellar medial surface posteriorly and the lateral surface anteriorly. The patella should tilt 15 degrees on medial and lateral side and should be compared to the uninvolved side.[11]
Compression test
Tests for patellofemoral joint degeneration.
The patella is compressed as the patient flexes his knee. A positive test is an increase of patient's knee pain. [12]
Clarke’s test
Clarke’s test or Patellar grind test, tests for chondromalacia patella.
The therapist compresses the patient’s patella into the trochlear while the patient contracts the quadriceps. A positive test is reproduction of the symptoms. However, It is not recommended to be used as it increases the patient’s condition and has high false-positive results.[12]
Muscles strength should be assessed for the lower limb muscles.
The muscles flexibility is assessed for the hamstrings by the popliteal angle, Thomas test for the rectus femoris and iliopsoas and ober’s test for the iliotibial band.
Finally, the examination is finished when an evaluation of the lumbar, hip and ankle is complete. The neurovascular assessment of the limb is also made. [12]
| [14] | [15] |
References[edit | edit source]
- ↑ Willy, R.W., Hoglund, L.T., Barton, C.J., Bolgla, L.A., Scalzitti, D.A., Logerstedt, D.S., Lynch, A.D., Snyder-Mackler, L., McDonough, C.M., Altman, R. and Beattie, P., 2019. Patellofemoral pain: clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. Journal of Orthopaedic & Sports Physical Therapy, 49(9), pp.CPG1-CPG95.
- ↑ Shi W, Li Y, Xiong B, Du M. Diagnosis of Patellofemoral Pain Syndrome Based on a Multi-Input Convolutional Neural Network With Data Augmentation. Frontiers in Public Health. 2021 Feb 11;9:643191.
- ↑ Hart, H.F., Patterson, B.E., Crossley, K.M., Culvenor, A.G., Khan, M.C., King, M.G. and Sritharan, P., 2022. May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis. British Journal of Sports Medicine, 56(9), pp.521-530.
- ↑ 4.0 4.1 Kim Y-M, Joo Y-B. Patellofemoral Osteoarthritis. Knee Surgery Related Research. 2012;24(4):193-200. doi:10.5792/ksrr.2012.24.4.193.
- ↑ 5.0 5.1 5.2 Medscape. Drugs and Diseases. Patellofemoral Joint Syndromes. Available at: http://emedicine.medscape.com/article/90286-overview#showall (accessed 08 august 2016).
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Neumann DA. Kinesiology of the musculoskeletal system; Foundation for rehabilitation. Mosby & Elsevier. 2010.
- ↑ NAVARRO, Marcelo Schmidt et al. Relationship between the lateral patellofemoral ligament and the width of the lateral patellar facet. Acta ortop. bras. [online]. 2010, vol.18, n.1, pp.19-22. ISSN 1413-7852.
- ↑ Healio MedBlog. Orthopedics. Business of Orthopedics. BLOG: Update on medial patelofemoral anatomy, implications for reconstruction. Available at: http://www.healio.com/orthopedics/business-of-orthopedics/news/blogs/%7B556829f5-0f97-42a6-9c3f-4f6ffe7aa48e%7D/patellofemoral-update/blog-update-on-medial-patellofemoral-anatomy-implications-for-reconstruction (accesed 10 august 2016).
- ↑ Borbas P, Koch P, Fucentese S. Lateral Patellofemoral Ligament Reconstruction Using a Free Gracilis Autograft. ORTHOPEDICS. 2014; 37: e665-e668. doi: 10.3928/01477447-20140626-66
- ↑ Roy Wung. Patellofemoral joint motion and patellar tracking. Available from: https://www.youtube.com/watch?v=Q-80Qi5cx9o (accessed 27 august 2016).
- ↑ 11.0 11.1 11.2 Manske RC, Davies GJ. Examination of the patellofemoral joint. International journal of sports physical therapy. 2016 Dec;11(6):831.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 Rodríguez-Merchán EC, Liddle AD, editors. Disorders of the Patellofemoral Joint: Diagnosis and Management. Springer; 2019 May 17.
- ↑ 13.0 13.1 Sankineani SR, Karnatzikos G, Chaurasia S, Gobbi A. Clinical Examination of the Patellofemoral Joint. InThe Patellofemoral Joint 2014 (pp. 23-27). Springer, Berlin, Heidelberg.
- ↑ Jason Craig. Examination of the Patellofemoral Joint - Palpation. Available from: https://www.youtube.com/watch?v=LgBNuWQMSC8 (accessed 27 august 2016).
- ↑ Jason Craig. Patellofemoral Joint Examination - Observations. Available from: https://www.youtube.com/watch?v=we9COmZ-cig (accessed 27 august 2016).