Neurological Physiotherapy in Private Practice: Difference between revisions
Sonja Murphy (talk | contribs) No edit summary |
Rucha Gadgil (talk | contribs) No edit summary |
||
| (199 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
< | <div class="editorbox"> '''Original Editor '''- [[User:Sonja Murphy|Sonja Murphy]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
==Introduction== | |||
Neurological Physiotherapy is a specialist area of physiotherapy focused on the treatment of individuals with neurological conditions. Neurological disorders affect the functioning of the [[Brain Anatomy|brain]], [[Spinal cord anatomy|spinal cord]], and nerves. [[Stroke]], [[Multiple Sclerosis (MS)]], [[Spinal Cord Injury]] and [[Parkinson's|Parkinson’s]] are common neurological conditions. It also includes conditions of the peripheral nervous system such as [[Guillain-Barre Syndrome|Guillain Barre Syndrome]]. | |||
Neurological conditions can have a devastating impact on the lives of the patients, family and friends. Disturbances in the travelling of messages between the brain and the body can result in the loss of movement, sensation, coordination, and balance. Other aspects of bodily function, such as perception, speech, memory, cognition, and behaviour may also be affected. Therefore, it is important that neurological physiotherapists work in close partnership with other members of the multidisciplinary team including speech and language therapists, occupational therapist, dieticians, nurses, and doctors. | |||
< | Effective communication between patient, family members, and the multidisciplinary team is critical to positive healthcare outcomes following a neurological disorder <ref name="Neurological Physiotherapy">Franz S, Muser J, Thielhorn U, Wallesch CW, Behrens J. Inter-professional communication and interaction in the neurological rehabilitation team: a literature review. ''Disabil Rehabil''. 2020;42(11):1607-1615. doi:10.1080/09638288.2018.1528634</ref>. | ||
== The Role of a Neurological Physiotherapist == | |||
Neurological physiotherapists are experienced and trained to treat neurological conditions with the aim to provide interventions which assist an individual to regain or maintain their maximum movement and functional independence. This is achieved by aiding in the development of new pathways through repetition and exercise, i.e., [[neuroplasticity]]. | |||
== Treatment Interventions == | |||
< | A number of treatment approaches are used, often incorporating a selection of the following as appropriate <ref name="Neurological Physiotherapy" /> | ||
*Stretching | |||
*Strengthening | |||
*[[Balance Training|Balance]] re-education | |||
*[[Gait training|Gait]] re-education | |||
*Joint mobilization | |||
*[[Electrical Stimulation - Its role in upper limb recovery post-stroke|Electrical]] stimulation | |||
*Postural exercise | |||
*[[Spasticity]] management | |||
*Advice/Education on lifestyle, fatigue management, and exercise | |||
==Prevalence of Neurological Conditions== | |||
The Neurological Alliance <ref name="Neuro Numbers">Neurological Alliance. Neuro numbers. 2019. https://www.neural.org.uk/wp-content/uploads/2021/04/neuro-numbers-2019-1.pdf</ref> reported the total number of neurological cases in England to be 16.5 million with a further 1 million cases in Scotland reported in the NHS QIS Clinical Standards on Neurological Health Services <ref name="NHS QIS">National Health Service Quality Improvement Scotland., 2009. Neurological health services: Clinical standards.</ref>. | |||
[[Image:Prevalence of neurological conditions.jpg|left|500px|Neurological Conditions cases.]] | |||
<br> | <br> | ||
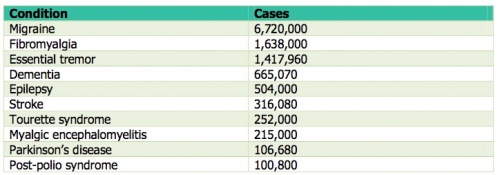
< | This table<ref name="Neurological Conditions cases">The Neurological Alliance., 2015.The invisible patients: revealing the state of neurology services [online]. London: The Neurological Alliance. pp. 1-69. https://www.neural.org.uk/assets/pdfs/2015-01-invisible-patients.pdf</ref>represents the most common neurological conditions in England. | ||
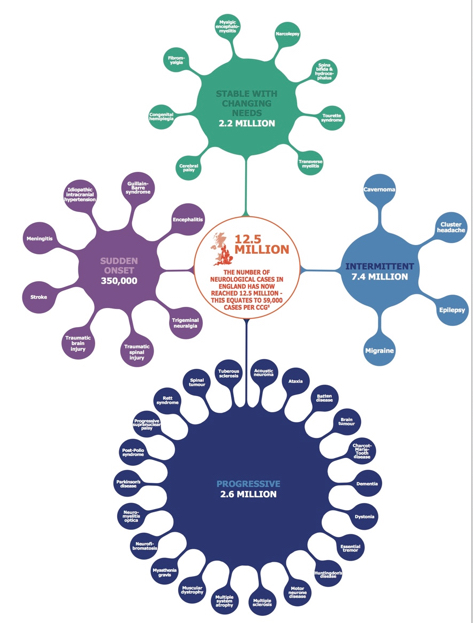
< | The image<ref name="Neuro Numbers" /> below illustrates the number of neurological conditions and the distribution of cases between progressive, intermittent, stable with changing needs, and sudden onset. | ||
[[Image:Colourful splats.jpg|700x700px]] | |||
==Public Perceptions of Neurological Conditions== | |||
[[ | A study conducted by Ryder et al. revealed that 45% of the UK population feared being impacted by a neurological condition the most, compared to 36% who feared getting cancer. The study highlighted the beliefs of the public with regards to neurological conditions, showing that 26% of the public felt that “nothing much can be done” for people with neurological conditions <ref name="Sue Ryder">Sue Ryder., 2016. Public fear getting a neurological condition [online].[viewed 31 October 2016]. Available from: http://www.sueryder.org/media-centre/news/2016/june/public%20fear%20getting%20a%20neurological%20disorder</ref>. The Neurological Alliance conducted a [http://www.neural.org.uk/store/assets/files/495/original/Invisible_patients_-_revealing_the_state_of_neurology_services_final_14_January_2015_.pdf neurological patient experience survey] in 2014 <ref name="Neurological Conditions cases" />. <br> | ||
[[Image:Neurological patient experience survey profile.jpg|left|400x400px]] | |||
[[Image:Neurological conditions in the survey.jpg|right|500x400px]]Figure 1 illustrates the population responding to this survey<br> | [[Image:Neurological conditions in the survey.jpg|right|500x400px]]Figure 1 illustrates the population responding to this survey<br> | ||
| Line 87: | Line 50: | ||
<br> | <br> | ||
Figure 2 indicates the neurological conditions represented in the survey.<br> | |||
Figure 2 indicates the neurological conditions represented in the survey. | |||
<br> | |||
<br> | <br> | ||
<br> | <br>The survey stated that 58.1% (n=3402) of NHS England respondents (n=6916) have experienced difficulty accessing the service/treatment they require, 39.8% (n= 2357) of respondents had a 12-month waiting period from the time of observation of the first symptom to seeing a neurologist specialist, 31.5% of respondents (n=2140) had 5 or more GP visits related to the health problems experienced due to their condition prior to being referred to a neurological specialist, and 71.5% (n=4603) of respondents were not provided with a care plan to help manage their condition. <ref name="Neurological Conditions cases" /> | ||
The survey stated that 58.1% (n=3402) of NHS England respondents (n=6916) have experienced difficulty accessing the service/treatment they require, 39.8% (n= 2357) of respondents had a 12-month waiting period from the time of observation of the first symptom to seeing a neurologist specialist, 31.5% of respondents (n=2140) had 5 or more GP visits related to the health problems experienced due to their condition prior to being referred to a neurological specialist, and 71.5% (n=4603) of respondents were not provided with a care plan to help manage their condition | |||
===Public Health Services=== | |||
< | The Scottish Stroke Care Audit 2015 <ref name="Scottish stroke care audit">National Health Service Scotland, 2015. Scottish stroke care audit: public summary of 2015 national report [online]. Edinburgh: ISD Scotland Publications. pp. 1-37. [viewed 1 November 2016]. Available from: http://www.strokeaudit.scot.nhs.uk/Downloads/2015_report/SSCA-summary-2015-web.pdf</ref> identified clear standards for stroke services in Scottish hospitals to achieve. Standard one states that at least 90% of stroke patients should be admitted to the stroke unit on the day they arrive or the day after. | ||
== | A large systemic review of organised stroke unit care showed evidence to indicate that stroke patients have better clinical outcomes in terms of independence, survival, and returning home. Stroke Unit care can decrease the risk of death and disability following a stroke. Admission to a stroke unit is the optimum choice of treatment, however, it is not always feasible due to Scotland’s geographically scattered population. Suspected stroke patients can often present to rural, remote hospitals which lack a stroke physician. Smaller hospitals may have generic rehabilitation services rather than an organised stroke unit. Research favours a stroke-specific ward over a general medical ward or mixed rehabilitation ward, with fewer patient deaths and fewer patients remaining dependent.<ref name="SIGN">Scottish Intercollegiate Guidelines Network., 2010. Management of patients with stroke: Rehabilitation, prevention and management of complications, and discharge planning. Edinburgh:SIGN.</ref> | ||
=== Do Patients Get Enough Therapy in Hospital? === | |||
< | Rehabilitation is evidence-based medicine utilised “to reach and maintain optimal functioning in physical, intellectual, psychological and/or social domains, according to the World Health Organisation<ref name="International Classification of Functioning, Disability and Health:">World Health Organization, 2001. International Classification of Functioning, Disability and Health: ICF. World Health Organization.</ref>. | ||
< | It has been recognised that many patients in stroke units feel they do not receive enough therapy during their hospital stay. The SSNAP <ref name="How good is stroke care?:first SSNAP annual report" /> reported that physiotherapy is required by 85% of stroke patients. Despite this, patients who need physiotherapy only receive 32 minutes on average on just over 50% of their days in hospital. This is one of the NHS's downfalls as patients should be obtaining the equivalent of 45 minutes of physiotherapy per day for 5 days a week. These are the opinions of stroke survivors regarding the care they received in the UK by the NHS in 2013-2014, highlighting some key areas of concern<ref name="How good is stroke care?:first SSNAP annual report" />.<br> | ||
[[Image: | [[Image:Quote 4.jpg|225x225px]][[Image:Quote 6.jpg|250x250px]][[Image:Quote 5.jpg|225x225px]] | ||
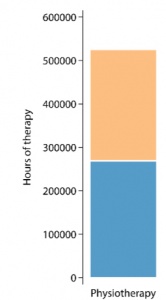
<div>This graph <ref name="How good is stroke care?:first SSNAP annual report">Royal College of Physicians., 2014. How good is stroke care?:first SSNAP annual report [online]. London: SSNAP. pp. 1-39. https://www.hqip.org.uk/wp-content/uploads/2019/06/Ref-142-SSNAP-Annual-Report-FINAL.pdf</ref> shows the number of hours of physiotherapy given throughout the year, April 2013- March 2014 in comparison to the target number of hours which would have been given if each patient who needed physiotherapy received 45 minutes, 5 days a week during their as an inpatient. | |||
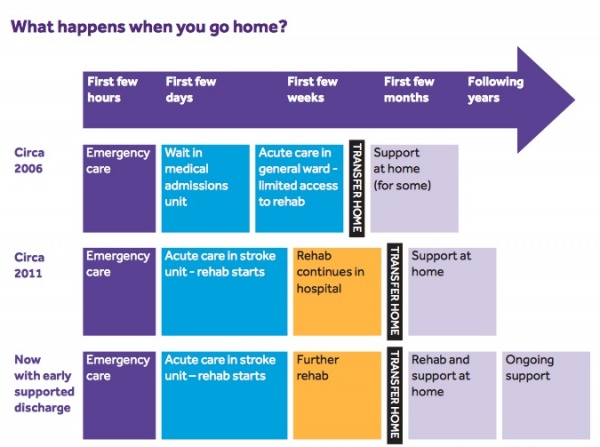
[[Image:Target hours of physio.jpg|300x300px|right]]The NHS does not have sufficient resources to provide long-term physiotherapy treatment for stroke survivors. Instead, the focus is placed on the initial period following a stroke. Pressure can be felt by patients within the hospital setting to reach targets fast in order to reach their recovery potential within a specified timeframe and some patients are led to believe that after 6 months, recovery stops. It is essential to know that stroke can potentially be a deteriorating condition as patients who do not continue treatment may become stiffer and less mobile. Also due to pressures on hospital beds, patients may get an early supported discharge with the continuation of treatment at home <ref name="Scottish stroke statistics">National Health Service Scotland., 2016. Scottish stroke statistics [online]. [viewed 1 November 2016]. Available from: https://www.isdscotland.org/Health-Topics/Stroke/Publications/2016-01-26/2016-01-26-Stroke-Report.pdf</ref>, as shown in the illustration below. However, treatment at home may be delayed, reduced in intensity, and hence hinder recovery. <br> | |||
=== Discharge Planning === | |||
Early supported discharge can lead to better outcomes for patients, studies show that certain areas in the UK where this service is unavailable, leaving patients isolated with limited therapy at home. | |||
< | [[Image:What happens when you go home.jpg|600x600px]] | ||
=== Private Practice for Stroke Care === | |||
<div> | |||
Hospital care for stroke is not the only option available. For those who need ongoing care, there is an option to continue care and treatment in private practice. This option can be of benefit to numerous people to eliminate pressures related to timescales and improve accessibility to therapy. Patients can receive a higher volume and frequency of therapy which is critical, especially in the early stages post-stroke. Evidence shows that spontaneous recovery tends to occur mostly within the first 3 months <ref name="Getting neurorehabilitation right: what can be learned from animal models?">Krakauer JW, Carmichael ST, Corbett D, Wittenberg GF. Getting neurorehabilitation right: what can be learned from animal models?. Neurorehabilitation and neural repair. 2012 Oct;26(8):923-31.</ref>. Motor impairment is the focus for stroke rehabilitation of physiotherapists <ref name="Motor recovery after stroke: a systematic review.">Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. The Lancet Neurology. 2009 Aug 1;8(8):741-54.</ref>. In the first 30 days following a stroke, the largest improvement in motor recovery occurs. However, significant progress is still seen up to 90 days’ post-stroke in patients with more severe deficits. <ref name="Measurement of motor recovery after stroke. Outcome assessment and sample size requirements">Duncan PW, Goldstein LB, Matchar D, Divine GW, Feussner J. [http://stroke.ahajournals.org/content/23/8/1084.long Measurement of motor recovery after stroke. Outcome assessment and sample size requirements.] Stroke. 1992 Aug;23(8):1084-9.[viewed 3 November 2016].</ref> <ref name="Similar motor recovery of upper and lower extremities after stroke">Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB. [http://stroke.ahajournals.org/content/25/6/1181 Similar motor recovery of upper and lower extremities after stroke]. Stroke. 1994 Jun;25(6):1181-8.viewed 3 November 2016]. Available from: </ref> <ref name="Management of adult stroke rehabilitation care: a clinical practice guideline">Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, Katz RC, Lamberty K, Reker D. [http://stroke.ahajournals.org/content/36/9/e100.full Management of adult stroke rehabilitation care: a clinical practice guideline.] Stroke. 2005 Sep 1;36(9):e100-43. [viewed 3 November 2016] Available from: </ref> Private neurological physiotherapy services in the UK have experienced significant improvements in the functioning levels of patients with a stroke beyond the first 6 months. Neurological physiotherapists re-educate the brain and body through movement that allows further progression in rehabilitation to be achieved. <ref name="Neurological physiotherapy for long term strokes">Heads Up Neuro Rehab Ltd., 2016. [http://headsup.co.uk/neurological-physiotherapy-for-long-term-strokes/ Neurological physiotherapy for long term strokes] [online].[viewed 2 November 2016] Available from: </ref><div> | |||
=== NHS Parkinson's Care === | |||
<div> | |||
Parkinson’s is the second most common neurological condition in the UK. The NHS Lothian Neurological Care Improvement Plan 2014-2017 states that medical care alone is insufficient for this disease. In spite of this, patients with Parkinson’s frequently have no access to allied health professionals. The Edinburgh Parkinson’s Assessment Clinic (EPAC) is led by therapists to provide people diagnosed with Parkinson’s access to advice from a physiotherapist. However, the EPAC offers all newly diagnosed patients of parkinsonism a once-off assessment by a physiotherapist to provide education on self-management. | |||
< | Physiotherapy aimed at rehabilitating patients with Parkinson's focuses on posture, upper limb function, transfers, balance, physical capacity, and gait. Supporting evidence in recent years for the inclusion of physiotherapy in the care of Parkinson’s has increased <ref name="Physical therapy in Parkinson's: evolution and future challenges">Keus SH, Munneke M, Nijkrake MJ, Kwakkel G, Bloem BR. Physical therapy in Parkinson's disease: evolution and future challenges. Movement disorders. 2009 Jan 15;24(1):1-4.</ref>. Management guidelines such as the [https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0008867/pdf/PubMedHealth_PMH0008867.pdf National Collaborating Centre for Chronic Conditions: National clinical guidelines for diagnosis and management in primary and secondary care of Parkinson's] <ref name="Parkinson’s disease: national clinical guideline for diagnosis and management in primary and secondary care">Collaborating Centre for Chronic Conditions (Great Britain). 2006. [https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0008867/pdf/PubMedHealth_PMH0008867.pdf Parkinson's disease: national clinical guideline for diagnosis and management in primary and secondary care]. </ref> and the [http://onlinelibrary.wiley.com/store/10.1002/mds.21244/asset/21244_ftp.pdf?v=1&t=iv143vsw&s=93baac2479c4103cb2114bcf8151168c0f24ca54 Royal Dutch Society of Physical Therapy's practice recommendations ]<ref name="vidence-based analysis of physical therapy in Parkinson’s disease with recommendations for practice and research.">Keus SH, Bloem BR, Hendriks EJ, Bredero‐Cohen AB, Munneke M, Practice Recommendations Development Group. [http://onlinelibrary.wiley.com/store/10.1002/mds.21244/asset/21244_ftp.pdf?v=1&t=iv143vsw&s=93baac2479c4103cb2114bcf8151168c0f24ca54 Evidence‐based analysis of physical therapy in Parkinson's disease with recommendations for practice and research]. Movement disorders. 2007 Mar 15;22(4):451-60. </ref> have supported physiotherapy, leading to an increase in the number of referrals to physiotherapy. A systemic review and meta-analysis completed by Tomlinson et al. 2012 <ref name="Physiotherapy intervention in Parkinson’s disease: systematic review and meta-analysis">Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, Shah L, Sackley C, Deane KH, Wheatley K, Ives N. [http://www.bmj.com/content/bmj/345/bmj.e5004.full.pdf Physiotherapy intervention in Parkinson’s disease: systematic review and meta-analysis]. BMJ. 2012 Aug 6;345:e5004. </ref> showed that physiotherapy resulted in significant outcomes for gait speed, balance, and the unified Parkinson’s disease rating scale. | ||
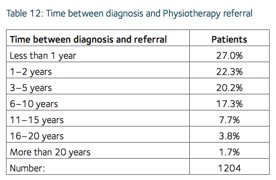
However, the 2015 UK Parkinson’s Audit <ref name="Parkinson’s Audit Summary Report">UK Parkinson's Excellence Network., 2015. 2015 UK Parkinson’s Audit Summary Report [online]. London:UK Parkinson's. pp. 1-43. [https://www.parkinsons.org.uk/sites/default/files/2017-11/audit2015_summaryreport.pdf</ref> showed that only 50% of patients with Parkinson's are referred to a physiotherapist within two years of diagnosis, as shown in the table below. | |||
[[Image:Time between diagnosis and physiotherapy referral.jpg|400x400px]] | |||
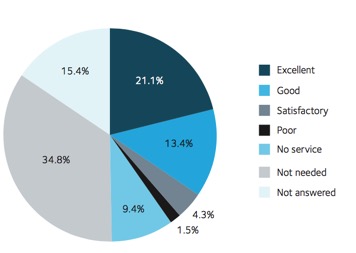
This Patient Reported Experience Measure (PREM) collected the views from patients with Parkinson's and their carers regarding their Parkinson's service. There were a total of 5,835 people with and carers for Parkinson's who responded to the questionnaire. The pie chart below represents the quality of physiotherapy service offered <ref name="Parkinson’s Audit Summary Report" />. [[Image:Pie chart.jpg|center|500x500px]] | |||
<div> | |||
< | ===The ParkinsonNet model=== | ||
<div> | |||
Bloem and Munneke <ref name="Revolutionising management of chronic disease: the ParkinsonNet approach">Bloem BR, Munneke M. Revolutionising management of chronic disease: the ParkinsonNet approach. Bmj. 2014 Mar 19;348:g1838. </ref> recognised that Parkinson's is a condition where patients require long term support to manage, hence described the benefits of a model of integrated care incorporating a network of specialists. ParkinsonNet is a scheme established in the Netherlands to tackle problems such as inadequate interdisciplinary collaboration and communication, lack of specific training and expertise in PD, treatment focus on the suppression of symptoms via drugs, and that referrals to allied health professionals such as physiotherapy being arbitrary. This model developed regional networks of inspiring, motivated, specialist health professionals to whom patients are referred for treatment long term <ref name="Revolutionising management of chronic disease: the ParkinsonNet approach" />. Parkinson’s UK and the Parkinson’s service have been advocating the ParkinsonNet model, however as highlighted by the NHS Lothian Neurological Care Improvement Plan 2014-2017 <ref name="Lothian Improvement Plan">National Health Service Lothian., 2015. Lothian neurological care improvement plan 2014 to 2017. https://org.nhslothian.scot/strategies/wp-content/uploads/sites/33/2023/05/QualityStrategy5YearPlan.pdf</ref>, this model has yet to be established in Scotland. In 2014, the Chair of the Lothian Parkinson’s Service Advisory Group, Dr Conor Maguire sought approval for the appointment of a Specialist Parkinson’s Physiotherapist to lead the development of a multidisciplinary model such as ParkinsonNet to help decrease geographical inequalities and standardise the provision of multidisciplinary care within Lothian. This process is ongoing currently <ref name="Lothian Improvement Plan" />, meaning the patients with Parkinson's in Scotland are not receiving the benefits of this model. | |||
=== How Private Physiotherapy Can Aid in the Treatment of PD === | |||
<div> | |||
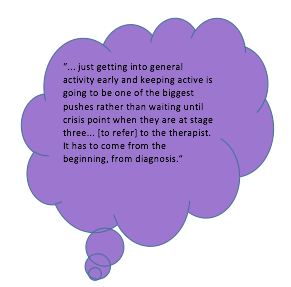
Due to the long waiting period between diagnosis and referral to physiotherapy, as highlighted in table 12 above, private physiotherapy can aid in reducing shortfalls in early therapeutic and preventative interventions. | |||
[[Image: | [[Image:Speech bubble.jpg|right|400x400px]]Bhanu Ramaswamy, a consultant physiotherapist in Derbyshire, shared the significance of early referral to physiotherapy in the treatment of Parkinson's to help avoid complications such as falls. She reiterated the importance of early intervention stating: <ref name="Please mind the gap:Parkinson’s disease services today">All Party Parliamentary Group for Parkinson's Disease., 2009. Please mind the gap:Parkinson’s disease services today. pp. 1-40. https://www.parkinsons.org.uk/sites/default/files/2017-07/cs2762_appg_inquiry_into_mental_health_questions_0.pdf</ref> | ||
Private physiotherapy can provide early intervention to delay the decline in a patient’s conditions and help maintain or improve a patient’s quality of life, confidence, and mobility. A person with Parkinson's responded to the APPG’s enquiry by saying <ref name="Please mind the gap:Parkinson’s disease services today" />: | |||
< | Private neurological physiotherapy can ensure that patients receive early intervention following diagnosis, allowing patients to benefit from a preventative approach to care<ref name="Please mind the gap:Parkinson’s disease services today" />. | ||
==Overall Benefits of Private Physiotherapy for Neurological Conditions== | |||
[[ | Private UK neurological physiotherapy clinics in London provide specialist physiotherapy for neurological conditions such as [[Stroke]], [[Parkinson's|Parkinson’s]], [[Overview of Traumatic Brain Injury|Traumatic Brain Injury]], [[Multiple Sclerosis (MS)]], and [[Spinal Cord Injury]]. | ||
At such clinics, the majority of clients attend x3 sessions a week, addressing issues proactively to prevent long term complications from developing. For progressive neurological conditions such as PD, the clinic aims to provide treatment and advice at each stage of the condition. A major benefit to private physiotherapy is on the achievement of a client’s short term goals, focus shifts immediately to long-term maintenance and progression through a combination of neuro physiotherapy and the use of FES machines, neuro pilates, personal training, and massage therapy. | |||
Many private clinics purchase state-of-the-art equipment. With longer and more frequent treatment sessions privately, patients can really experience benefits using advanced, up-to-date technology. The role of a private physiotherapist is to help a client reflect on important outcomes from a functional perspective to quality of life using careful documentation and involving family members. It is clear that private physiotherapy for neurological conditions plays a pivotal role in helping clients achieve a threshold level of mobility and gain confidence and competence with exercise in order to support the transition to a local leisure club or community-based activity groups. | |||
Receiving regular physiotherapy not only improves patients physically, but also psychologically, building patient and family members confidence, positivity, hope, and belief. The video<ref name="Youtube video">Challenge Center., 2015. Challenge center video 2014 [online video]. California: Challenge Center. [viewed 3 November 2016]. Available from: https://www.youtube.com/watch?v=TDGETLa4Bm8</ref> below describes the physical and psychological benefits private physiotherapy brings to the lives of people with a neurological condition and their family members.<br> {{#ev:youtube|TDGETLa4Bm8|700}} | |||
==References == | |||
<references /> | <references /> | ||
[[Category:Neurology]] | |||
[[Category:Rehabilitation]] | |||
Latest revision as of 23:10, 31 October 2023
Introduction[edit | edit source]
Neurological Physiotherapy is a specialist area of physiotherapy focused on the treatment of individuals with neurological conditions. Neurological disorders affect the functioning of the brain, spinal cord, and nerves. Stroke, Multiple Sclerosis (MS), Spinal Cord Injury and Parkinson’s are common neurological conditions. It also includes conditions of the peripheral nervous system such as Guillain Barre Syndrome.
Neurological conditions can have a devastating impact on the lives of the patients, family and friends. Disturbances in the travelling of messages between the brain and the body can result in the loss of movement, sensation, coordination, and balance. Other aspects of bodily function, such as perception, speech, memory, cognition, and behaviour may also be affected. Therefore, it is important that neurological physiotherapists work in close partnership with other members of the multidisciplinary team including speech and language therapists, occupational therapist, dieticians, nurses, and doctors.
Effective communication between patient, family members, and the multidisciplinary team is critical to positive healthcare outcomes following a neurological disorder [1].
The Role of a Neurological Physiotherapist[edit | edit source]
Neurological physiotherapists are experienced and trained to treat neurological conditions with the aim to provide interventions which assist an individual to regain or maintain their maximum movement and functional independence. This is achieved by aiding in the development of new pathways through repetition and exercise, i.e., neuroplasticity.
Treatment Interventions[edit | edit source]
A number of treatment approaches are used, often incorporating a selection of the following as appropriate [1]
- Stretching
- Strengthening
- Balance re-education
- Gait re-education
- Joint mobilization
- Electrical stimulation
- Postural exercise
- Spasticity management
- Advice/Education on lifestyle, fatigue management, and exercise
Prevalence of Neurological Conditions[edit | edit source]
The Neurological Alliance [2] reported the total number of neurological cases in England to be 16.5 million with a further 1 million cases in Scotland reported in the NHS QIS Clinical Standards on Neurological Health Services [3].
This table[4]represents the most common neurological conditions in England.
The image[2] below illustrates the number of neurological conditions and the distribution of cases between progressive, intermittent, stable with changing needs, and sudden onset.
Public Perceptions of Neurological Conditions[edit | edit source]
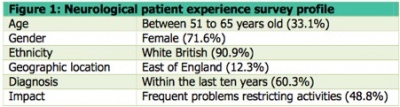
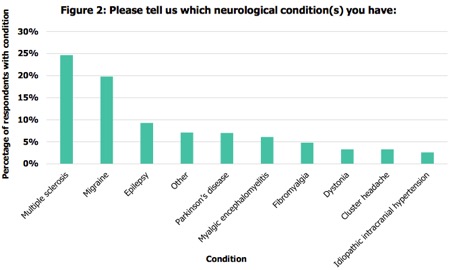
A study conducted by Ryder et al. revealed that 45% of the UK population feared being impacted by a neurological condition the most, compared to 36% who feared getting cancer. The study highlighted the beliefs of the public with regards to neurological conditions, showing that 26% of the public felt that “nothing much can be done” for people with neurological conditions [5]. The Neurological Alliance conducted a neurological patient experience survey in 2014 [4].
Figure 1 illustrates the population responding to this survey
Figure 2 indicates the neurological conditions represented in the survey.
The survey stated that 58.1% (n=3402) of NHS England respondents (n=6916) have experienced difficulty accessing the service/treatment they require, 39.8% (n= 2357) of respondents had a 12-month waiting period from the time of observation of the first symptom to seeing a neurologist specialist, 31.5% of respondents (n=2140) had 5 or more GP visits related to the health problems experienced due to their condition prior to being referred to a neurological specialist, and 71.5% (n=4603) of respondents were not provided with a care plan to help manage their condition. [4]
Public Health Services[edit | edit source]
The Scottish Stroke Care Audit 2015 [6] identified clear standards for stroke services in Scottish hospitals to achieve. Standard one states that at least 90% of stroke patients should be admitted to the stroke unit on the day they arrive or the day after.
A large systemic review of organised stroke unit care showed evidence to indicate that stroke patients have better clinical outcomes in terms of independence, survival, and returning home. Stroke Unit care can decrease the risk of death and disability following a stroke. Admission to a stroke unit is the optimum choice of treatment, however, it is not always feasible due to Scotland’s geographically scattered population. Suspected stroke patients can often present to rural, remote hospitals which lack a stroke physician. Smaller hospitals may have generic rehabilitation services rather than an organised stroke unit. Research favours a stroke-specific ward over a general medical ward or mixed rehabilitation ward, with fewer patient deaths and fewer patients remaining dependent.[7]
Do Patients Get Enough Therapy in Hospital?[edit | edit source]
Rehabilitation is evidence-based medicine utilised “to reach and maintain optimal functioning in physical, intellectual, psychological and/or social domains, according to the World Health Organisation[8].
It has been recognised that many patients in stroke units feel they do not receive enough therapy during their hospital stay. The SSNAP [9] reported that physiotherapy is required by 85% of stroke patients. Despite this, patients who need physiotherapy only receive 32 minutes on average on just over 50% of their days in hospital. This is one of the NHS's downfalls as patients should be obtaining the equivalent of 45 minutes of physiotherapy per day for 5 days a week. These are the opinions of stroke survivors regarding the care they received in the UK by the NHS in 2013-2014, highlighting some key areas of concern[9].
Discharge Planning[edit | edit source]
Early supported discharge can lead to better outcomes for patients, studies show that certain areas in the UK where this service is unavailable, leaving patients isolated with limited therapy at home.
Private Practice for Stroke Care[edit | edit source]
NHS Parkinson's Care[edit | edit source]
Parkinson’s is the second most common neurological condition in the UK. The NHS Lothian Neurological Care Improvement Plan 2014-2017 states that medical care alone is insufficient for this disease. In spite of this, patients with Parkinson’s frequently have no access to allied health professionals. The Edinburgh Parkinson’s Assessment Clinic (EPAC) is led by therapists to provide people diagnosed with Parkinson’s access to advice from a physiotherapist. However, the EPAC offers all newly diagnosed patients of parkinsonism a once-off assessment by a physiotherapist to provide education on self-management.
Physiotherapy aimed at rehabilitating patients with Parkinson's focuses on posture, upper limb function, transfers, balance, physical capacity, and gait. Supporting evidence in recent years for the inclusion of physiotherapy in the care of Parkinson’s has increased [17]. Management guidelines such as the National Collaborating Centre for Chronic Conditions: National clinical guidelines for diagnosis and management in primary and secondary care of Parkinson's [18] and the Royal Dutch Society of Physical Therapy's practice recommendations [19] have supported physiotherapy, leading to an increase in the number of referrals to physiotherapy. A systemic review and meta-analysis completed by Tomlinson et al. 2012 [20] showed that physiotherapy resulted in significant outcomes for gait speed, balance, and the unified Parkinson’s disease rating scale.
However, the 2015 UK Parkinson’s Audit [21] showed that only 50% of patients with Parkinson's are referred to a physiotherapist within two years of diagnosis, as shown in the table below.
This Patient Reported Experience Measure (PREM) collected the views from patients with Parkinson's and their carers regarding their Parkinson's service. There were a total of 5,835 people with and carers for Parkinson's who responded to the questionnaire. The pie chart below represents the quality of physiotherapy service offered [21].The ParkinsonNet model[edit | edit source]
Bloem and Munneke [22] recognised that Parkinson's is a condition where patients require long term support to manage, hence described the benefits of a model of integrated care incorporating a network of specialists. ParkinsonNet is a scheme established in the Netherlands to tackle problems such as inadequate interdisciplinary collaboration and communication, lack of specific training and expertise in PD, treatment focus on the suppression of symptoms via drugs, and that referrals to allied health professionals such as physiotherapy being arbitrary. This model developed regional networks of inspiring, motivated, specialist health professionals to whom patients are referred for treatment long term [22]. Parkinson’s UK and the Parkinson’s service have been advocating the ParkinsonNet model, however as highlighted by the NHS Lothian Neurological Care Improvement Plan 2014-2017 [23], this model has yet to be established in Scotland. In 2014, the Chair of the Lothian Parkinson’s Service Advisory Group, Dr Conor Maguire sought approval for the appointment of a Specialist Parkinson’s Physiotherapist to lead the development of a multidisciplinary model such as ParkinsonNet to help decrease geographical inequalities and standardise the provision of multidisciplinary care within Lothian. This process is ongoing currently [23], meaning the patients with Parkinson's in Scotland are not receiving the benefits of this model.
How Private Physiotherapy Can Aid in the Treatment of PD[edit | edit source]
Due to the long waiting period between diagnosis and referral to physiotherapy, as highlighted in table 12 above, private physiotherapy can aid in reducing shortfalls in early therapeutic and preventative interventions.
Bhanu Ramaswamy, a consultant physiotherapist in Derbyshire, shared the significance of early referral to physiotherapy in the treatment of Parkinson's to help avoid complications such as falls. She reiterated the importance of early intervention stating: [24]Private physiotherapy can provide early intervention to delay the decline in a patient’s conditions and help maintain or improve a patient’s quality of life, confidence, and mobility. A person with Parkinson's responded to the APPG’s enquiry by saying [24]:
Private neurological physiotherapy can ensure that patients receive early intervention following diagnosis, allowing patients to benefit from a preventative approach to care[24].
Overall Benefits of Private Physiotherapy for Neurological Conditions[edit | edit source]
Private UK neurological physiotherapy clinics in London provide specialist physiotherapy for neurological conditions such as Stroke, Parkinson’s, Traumatic Brain Injury, Multiple Sclerosis (MS), and Spinal Cord Injury.
At such clinics, the majority of clients attend x3 sessions a week, addressing issues proactively to prevent long term complications from developing. For progressive neurological conditions such as PD, the clinic aims to provide treatment and advice at each stage of the condition. A major benefit to private physiotherapy is on the achievement of a client’s short term goals, focus shifts immediately to long-term maintenance and progression through a combination of neuro physiotherapy and the use of FES machines, neuro pilates, personal training, and massage therapy.
Many private clinics purchase state-of-the-art equipment. With longer and more frequent treatment sessions privately, patients can really experience benefits using advanced, up-to-date technology. The role of a private physiotherapist is to help a client reflect on important outcomes from a functional perspective to quality of life using careful documentation and involving family members. It is clear that private physiotherapy for neurological conditions plays a pivotal role in helping clients achieve a threshold level of mobility and gain confidence and competence with exercise in order to support the transition to a local leisure club or community-based activity groups.
Receiving regular physiotherapy not only improves patients physically, but also psychologically, building patient and family members confidence, positivity, hope, and belief. The video[25] below describes the physical and psychological benefits private physiotherapy brings to the lives of people with a neurological condition and their family members.References[edit | edit source]
- ↑ 1.0 1.1 Franz S, Muser J, Thielhorn U, Wallesch CW, Behrens J. Inter-professional communication and interaction in the neurological rehabilitation team: a literature review. Disabil Rehabil. 2020;42(11):1607-1615. doi:10.1080/09638288.2018.1528634
- ↑ 2.0 2.1 Neurological Alliance. Neuro numbers. 2019. https://www.neural.org.uk/wp-content/uploads/2021/04/neuro-numbers-2019-1.pdf
- ↑ National Health Service Quality Improvement Scotland., 2009. Neurological health services: Clinical standards.
- ↑ 4.0 4.1 4.2 The Neurological Alliance., 2015.The invisible patients: revealing the state of neurology services [online]. London: The Neurological Alliance. pp. 1-69. https://www.neural.org.uk/assets/pdfs/2015-01-invisible-patients.pdf
- ↑ Sue Ryder., 2016. Public fear getting a neurological condition [online].[viewed 31 October 2016]. Available from: http://www.sueryder.org/media-centre/news/2016/june/public%20fear%20getting%20a%20neurological%20disorder
- ↑ National Health Service Scotland, 2015. Scottish stroke care audit: public summary of 2015 national report [online]. Edinburgh: ISD Scotland Publications. pp. 1-37. [viewed 1 November 2016]. Available from: http://www.strokeaudit.scot.nhs.uk/Downloads/2015_report/SSCA-summary-2015-web.pdf
- ↑ Scottish Intercollegiate Guidelines Network., 2010. Management of patients with stroke: Rehabilitation, prevention and management of complications, and discharge planning. Edinburgh:SIGN.
- ↑ World Health Organization, 2001. International Classification of Functioning, Disability and Health: ICF. World Health Organization.
- ↑ 9.0 9.1 9.2 Royal College of Physicians., 2014. How good is stroke care?:first SSNAP annual report [online]. London: SSNAP. pp. 1-39. https://www.hqip.org.uk/wp-content/uploads/2019/06/Ref-142-SSNAP-Annual-Report-FINAL.pdf
- ↑ National Health Service Scotland., 2016. Scottish stroke statistics [online]. [viewed 1 November 2016]. Available from: https://www.isdscotland.org/Health-Topics/Stroke/Publications/2016-01-26/2016-01-26-Stroke-Report.pdf
- ↑ Krakauer JW, Carmichael ST, Corbett D, Wittenberg GF. Getting neurorehabilitation right: what can be learned from animal models?. Neurorehabilitation and neural repair. 2012 Oct;26(8):923-31.
- ↑ Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. The Lancet Neurology. 2009 Aug 1;8(8):741-54.
- ↑ Duncan PW, Goldstein LB, Matchar D, Divine GW, Feussner J. Measurement of motor recovery after stroke. Outcome assessment and sample size requirements. Stroke. 1992 Aug;23(8):1084-9.[viewed 3 November 2016].
- ↑ Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB. Similar motor recovery of upper and lower extremities after stroke. Stroke. 1994 Jun;25(6):1181-8.viewed 3 November 2016]. Available from:
- ↑ Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, Katz RC, Lamberty K, Reker D. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke. 2005 Sep 1;36(9):e100-43. [viewed 3 November 2016] Available from:
- ↑ Heads Up Neuro Rehab Ltd., 2016. Neurological physiotherapy for long term strokes [online].[viewed 2 November 2016] Available from:
- ↑ Keus SH, Munneke M, Nijkrake MJ, Kwakkel G, Bloem BR. Physical therapy in Parkinson's disease: evolution and future challenges. Movement disorders. 2009 Jan 15;24(1):1-4.
- ↑ Collaborating Centre for Chronic Conditions (Great Britain). 2006. Parkinson's disease: national clinical guideline for diagnosis and management in primary and secondary care.
- ↑ Keus SH, Bloem BR, Hendriks EJ, Bredero‐Cohen AB, Munneke M, Practice Recommendations Development Group. Evidence‐based analysis of physical therapy in Parkinson's disease with recommendations for practice and research. Movement disorders. 2007 Mar 15;22(4):451-60.
- ↑ Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, Shah L, Sackley C, Deane KH, Wheatley K, Ives N. Physiotherapy intervention in Parkinson’s disease: systematic review and meta-analysis. BMJ. 2012 Aug 6;345:e5004.
- ↑ 21.0 21.1 UK Parkinson's Excellence Network., 2015. 2015 UK Parkinson’s Audit Summary Report [online]. London:UK Parkinson's. pp. 1-43. [https://www.parkinsons.org.uk/sites/default/files/2017-11/audit2015_summaryreport.pdf
- ↑ 22.0 22.1 Bloem BR, Munneke M. Revolutionising management of chronic disease: the ParkinsonNet approach. Bmj. 2014 Mar 19;348:g1838.
- ↑ 23.0 23.1 National Health Service Lothian., 2015. Lothian neurological care improvement plan 2014 to 2017. https://org.nhslothian.scot/strategies/wp-content/uploads/sites/33/2023/05/QualityStrategy5YearPlan.pdf
- ↑ 24.0 24.1 24.2 All Party Parliamentary Group for Parkinson's Disease., 2009. Please mind the gap:Parkinson’s disease services today. pp. 1-40. https://www.parkinsons.org.uk/sites/default/files/2017-07/cs2762_appg_inquiry_into_mental_health_questions_0.pdf
- ↑ Challenge Center., 2015. Challenge center video 2014 [online video]. California: Challenge Center. [viewed 3 November 2016]. Available from: https://www.youtube.com/watch?v=TDGETLa4Bm8