Trendelenburg Sign: Difference between revisions
No edit summary |
No edit summary |
||
| (62 intermediate revisions by 16 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Tyler Shultz|Tyler Shultz]], [[User:Lesley Dumitresco|Lesley Dumitresco]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]]. | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
The Trendelenburg sign is a quick physical examination that can assist the therapist in assessing for any hip dysfunction.<ref name=":0">Hardcastle PH, Nade SY. [https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.67B5.4055873 The significance of the Trendelenburg test.] The Journal of bone and joint surgery. British volume. 1985 Nov;67(5):741-6.</ref>This is often referred to as the Trendelenburg test but should not be confused with the [[Brodie–Trendelenburg Test|Brodie–Trendelenburg test]] which is used to determine the competency of the valves in the superficial and deep veins of patients with [[Varicose Veins|varicose veins]]. | |||
== | A positive Trendelenburg sign usually indicates weakness in the hip abductor muscles: [[Gluteus Medius|gluteus medius]] and [[Gluteus Minimus|gluteus minimus]].<ref name=":0" /> These findings can be associated with various hip abnormalities such as congenital hip dislocation, rheumatic arthritis, [[Hip Disability and Osteoarthritis Outcome Score|osteoarthritis]].<ref name=":0" /><ref name=":2" /> | ||
[[File:Trendelenburg gait.jpg|center|thumb|406x406px|Positive and negative Trendelenburg sign]] | |||
A positive test is one in which the pelvis drops on the contralateral side during a single-leg stand on the affected side. This can also be identified during [[Gait Cycle|gait]]: compensation occurs by side flexing the trunk towards the involved side during the stance phase on the affected extremity.<ref>[[Trendelenburg Gait]]</ref> | |||
== | == Clinically relevant anatomy == | ||
[[Gluteus Medius|Gluteus medius]] and [[Gluteus Minimus|minimus]] are the primary abductors of the hip. When fully weight bearing they act to abduct the femur away from the mid-line of the body and provide stability of the hip and pelvis.<ref>Palastanga N, Soames R. Anatomy and Human Movement: Structure and Function. 6th ed. London, United Kingdom: Churchill Livingstone; 2012.</ref> | |||
== Purpose == | |||
= | The purpose of the Trendelenburg Test is to identify the weakness of the hip abductors.<ref name=":0" /> | ||
Besides the identification of weakness in the hip abductors of the standing leg, the Trendelenburg sign can be used to assess other mechanical, neurological or spinal disorders, such as the Congenital dislocation of the hip or hip subluxation.<ref name=":0" /><ref name=":2" /><ref>Rang M. Anthology of orthopaedics. Edinburgh. E&S Livingstone, 1966; 139-43.</ref><ref name=":3">Windhager RE, Pongracz NI, Schonecker WO, Kotz RA. [https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.73B6.1955430 Chiari osteotomy for congenital dislocation and subluxation of the hip. Results after 20 to 34 years follow-up]. The Journal of bone and joint surgery. British volume. 1991 Nov;73(6):890-5.</ref> | |||
== | == Technique == | ||
{{#ev:youtube|mA3enWJ53Kc}} | |||
The patient is asked to stand on one leg for 30 seconds without leaning to one side the patient can hold onto something if balance is an issue. The therapist observes the patient to see if the pelvis stays level during the single-leg stance. A positive Trendelenburg Test is indicated if during unilateral weight bearing the pelvis drops toward the unsupported side<ref name=":4">Dutton M. Orthopaedic: Examination, evaluation, and intervention. 2nd ed. New York: The McGraw-Hill Companies, Inc; 2008.</ref><ref name=":0" />. | |||
<br> | |||
== Clinical relevance == | |||
Several dysfunctions can produce a positive Trendelenburg Test:<ref name=":4" /> | |||
== | *Weakness of gluteus medius<ref name=":0" /> | ||
*Hip instability and subluxation<ref name=":3" /> | |||
*Hip osteoarthritis <ref name=":1">Youdas JW, Madson TJ, Hollman JH. [https://www.tandfonline.com/doi/abs/10.3109/09593980902750857?src=recsys&journalCode=iptp20 Usefulness of the Trendelenburg test for identification of patients with hip joint osteoarthritis]. Physiotherapy theory and practice. 2010 Jan 1;26(3):184-94.</ref> | |||
*Initially post [[Total Hip Replacement]]<ref>Odak S, Ivory J. [https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620x.95b3.31098 Management of abductor mechanism deficiency following total hip replacement]. The bone & joint journal. 2013 Mar;95(3):343-7.</ref> | |||
*Superior Gluteal Nerve Palsy | |||
*Lower back pain<ref>Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. [https://www.sciencedirect.com/science/article/pii/S0161475407000735 Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising]. Journal of manipulative and physiological therapeutics. 2007 May 1;30(4):270-8.</ref> | |||
*[[Legg-Calve-Perthes Disease|Legg-Calvé-Perthes Disease]]<ref name=":2">Macnicol MF, Makris D. [https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620x.73b5.1894678 Distal transfer of the greater trochanter.] The Journal of bone and joint surgery. British volume. 1991 Sep;73(5):838-41.</ref> | |||
*Congenital hip dislocation<ref name=":2" /> | |||
= | |||
= | |||
= | |||
= | |||
== | |||
< | |||
[[ | |||
< | |||
</ | |||
A [[Trendelenburg Gait|Trendelenburg gait]] can also be observed caused by abductor insufficiency and is characterized by: | |||
*Pelvic drop in the swing phase | |||
*Trunk side flexion towards the stance limb | |||
*Hip adduction during the stance phase. | |||
== Clinical bottom line == | |||
< | The Trendelenburg sign alone cannot diagnose hip conditions such as osteoarthritis or hip instability<ref name=":1" />. It has been shown to be more effective when part of a battery of tests such as hand dynamometry and observation to help assess hip abductor strength<ref>Grimaldi A. [https://www.sciencedirect.com/science/article/pii/S1356689X10001499 Assessing lateral stability of the hip and pelvis]. Manual therapy. 2011 Feb 1;16(1):26-32.</ref>. It is a quick, easy test that can help identify functional weakness in a standing position. | ||
== See Also == | |||
<div>[[Trendelenburg_Gait]]<br> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Special_Tests]] | ||
[[Category:Pelvis - Assessment and Examination]] | |||
[[Category:Hip]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Muscles]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Athlete Assessment]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Older People/Geriatrics - Assessment and Examination]] | |||
[[Category:Hip - Assessment and Examination]] | |||
[[Category:Assessment]] | |||
[[Category:Hip - Special Tests]] | |||
Latest revision as of 13:18, 13 September 2023
Original Editor - Tyler Shultz, Lesley Dumitresco as part of the Vrije Universiteit Brussel's Evidence-based Practice project.
Top Contributors - Didzis Rozenbergs, Admin, Kim Jackson, Abbey Wright, Rachael Lowe, Tyler Shultz, Evelyne Bahire, WikiSysop, Dumitresco Lesley, Evan Thomas, Siobhán Cullen, Joanne Garvey, Uchechukwu Chukwuemeka, Wanda van Niekerk, 127.0.0.1, Lauren Lopez, Pinar Kisacik, Tony Lowe and Elaine Lonnemann
Definition/Description[edit | edit source]
The Trendelenburg sign is a quick physical examination that can assist the therapist in assessing for any hip dysfunction.[1]This is often referred to as the Trendelenburg test but should not be confused with the Brodie–Trendelenburg test which is used to determine the competency of the valves in the superficial and deep veins of patients with varicose veins.
A positive Trendelenburg sign usually indicates weakness in the hip abductor muscles: gluteus medius and gluteus minimus.[1] These findings can be associated with various hip abnormalities such as congenital hip dislocation, rheumatic arthritis, osteoarthritis.[1][2]
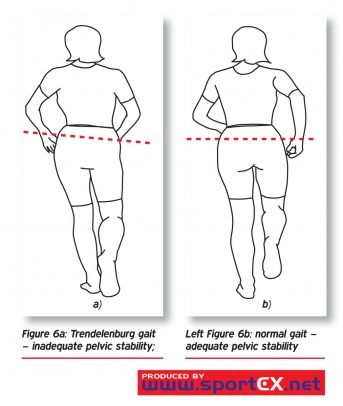
A positive test is one in which the pelvis drops on the contralateral side during a single-leg stand on the affected side. This can also be identified during gait: compensation occurs by side flexing the trunk towards the involved side during the stance phase on the affected extremity.[3]
Clinically relevant anatomy[edit | edit source]
Gluteus medius and minimus are the primary abductors of the hip. When fully weight bearing they act to abduct the femur away from the mid-line of the body and provide stability of the hip and pelvis.[4]
Purpose[edit | edit source]
The purpose of the Trendelenburg Test is to identify the weakness of the hip abductors.[1]
Besides the identification of weakness in the hip abductors of the standing leg, the Trendelenburg sign can be used to assess other mechanical, neurological or spinal disorders, such as the Congenital dislocation of the hip or hip subluxation.[1][2][5][6]
Technique[edit | edit source]
The patient is asked to stand on one leg for 30 seconds without leaning to one side the patient can hold onto something if balance is an issue. The therapist observes the patient to see if the pelvis stays level during the single-leg stance. A positive Trendelenburg Test is indicated if during unilateral weight bearing the pelvis drops toward the unsupported side[7][1].
Clinical relevance[edit | edit source]
Several dysfunctions can produce a positive Trendelenburg Test:[7]
- Weakness of gluteus medius[1]
- Hip instability and subluxation[6]
- Hip osteoarthritis [8]
- Initially post Total Hip Replacement[9]
- Superior Gluteal Nerve Palsy
- Lower back pain[10]
- Legg-Calvé-Perthes Disease[2]
- Congenital hip dislocation[2]
A Trendelenburg gait can also be observed caused by abductor insufficiency and is characterized by:
- Pelvic drop in the swing phase
- Trunk side flexion towards the stance limb
- Hip adduction during the stance phase.
Clinical bottom line[edit | edit source]
The Trendelenburg sign alone cannot diagnose hip conditions such as osteoarthritis or hip instability[8]. It has been shown to be more effective when part of a battery of tests such as hand dynamometry and observation to help assess hip abductor strength[11]. It is a quick, easy test that can help identify functional weakness in a standing position.
See Also[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Hardcastle PH, Nade SY. The significance of the Trendelenburg test. The Journal of bone and joint surgery. British volume. 1985 Nov;67(5):741-6.
- ↑ 2.0 2.1 2.2 2.3 Macnicol MF, Makris D. Distal transfer of the greater trochanter. The Journal of bone and joint surgery. British volume. 1991 Sep;73(5):838-41.
- ↑ Trendelenburg Gait
- ↑ Palastanga N, Soames R. Anatomy and Human Movement: Structure and Function. 6th ed. London, United Kingdom: Churchill Livingstone; 2012.
- ↑ Rang M. Anthology of orthopaedics. Edinburgh. E&S Livingstone, 1966; 139-43.
- ↑ 6.0 6.1 Windhager RE, Pongracz NI, Schonecker WO, Kotz RA. Chiari osteotomy for congenital dislocation and subluxation of the hip. Results after 20 to 34 years follow-up. The Journal of bone and joint surgery. British volume. 1991 Nov;73(6):890-5.
- ↑ 7.0 7.1 Dutton M. Orthopaedic: Examination, evaluation, and intervention. 2nd ed. New York: The McGraw-Hill Companies, Inc; 2008.
- ↑ 8.0 8.1 Youdas JW, Madson TJ, Hollman JH. Usefulness of the Trendelenburg test for identification of patients with hip joint osteoarthritis. Physiotherapy theory and practice. 2010 Jan 1;26(3):184-94.
- ↑ Odak S, Ivory J. Management of abductor mechanism deficiency following total hip replacement. The bone & joint journal. 2013 Mar;95(3):343-7.
- ↑ Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising. Journal of manipulative and physiological therapeutics. 2007 May 1;30(4):270-8.
- ↑ Grimaldi A. Assessing lateral stability of the hip and pelvis. Manual therapy. 2011 Feb 1;16(1):26-32.