Depression: Difference between revisions
mNo edit summary |
No edit summary |
||
| (170 intermediate revisions by 17 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [ | '''Original Editors ''' - [[User:Nadine Risman|Nadine Risman]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Lead Editors''' - | '''Lead Editors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
Depression | [[Image:Depression 2.jpg|right|150px]]Depression causes a persistent feeling of sadness and disinterest, clinical features being sadness, emptiness, and/or irritable mood. These features alongside body and mind changes can seriously affect functional capabilities, and can lead to suicide<ref name=":0">WHO [https://www.who.int/news-room/fact-sheets/detail/depression Depression] Available: https://www.who.int/news-room/fact-sheets/detail/depression (accessed 12.9.2021)</ref>. Due to false perceptions, nearly 60% of people with depression do not seek medical help. The outcomes for patients with depression are cautious, with the condition having frequent relapses and remissions, leading to a poor [[Quality of Life|quality of life]].<ref name=":1">Chand SP, Arif H. Depression. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK430847/ (Accessed, 12/9/2021). | ||
</ref> | |||
== | This short video provides an overview of what depression actually is including discussion of symptoms, causes, and treatment. | ||
{{#ev:youtube|v=fWFuQR_Wt4M|300}}<ref>Therapist Aid. What is Depression?. Available from: https://www.youtube.com/watch?v=fWFuQR_Wt4M [last accessed 22,1,2023]</ref> | |||
== Etiology == | |||
The etiology of major depression involves many factors, with both genetic, social, lifestyle and environmental factors all playing a role.<ref name=":1" /><ref>Better health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/depression Depression] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/depression (accessed 12.9.2021)</ref> | |||
* First-degree relatives of depressed individuals are about 3 times as likely to develop depression as the general population; however, depression can occur in people without family histories of depression. | |||
* [[Neurodegenerative Disease|Neurodegenerative]] diseases (especially [[Alzheimer's Disease|Alzheimer disease]] and [[Parkinson's|Parkinson disease]]), [[stroke]], [[Multiple Sclerosis (MS)|multiple sclerosis]], seizure disorders, [[Oncology|cancer]], macular degeneration, and [[Chronic Pain and the Brain|chronic pain]] have been associated with higher rates of depression. | |||
* Life events and hassles operate as triggers for the development of depression. | |||
* Environmental factors may make some people more vulnerable to depression, for example continuous exposure to violence, neglect, abuse or poverty.<ref name=":2">American Psychiatric Association [https://www.psychiatry.org/patients-families/depression/what-is-depression Depression] Available: https://www.psychiatry.org/patients-families/depression/what-is-depression<nowiki/>(accessed 12.9.2021)</ref> | |||
* Traumatic events eg death or loss of a loved one, lack of social support, caregiver burden, financial problems, interpersonal difficulties<ref name=":1" />. | |||
== Epidemiology == | |||
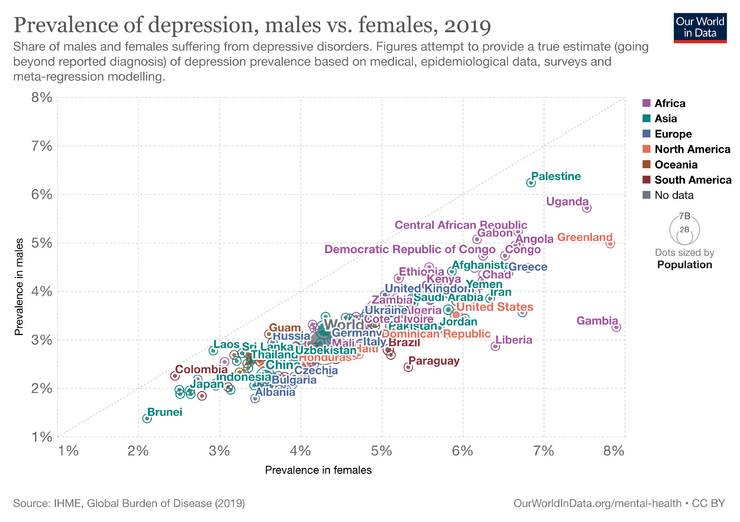
Depression is a common illness worldwide, with more than 264 million people affected.<ref name=":0" /> Twelve-month prevalence of major depressive disorder is approximately 7%, with marked differences by age group. | |||
== | * Prevalence in 18- to 29-year-old individuals is threefold higher than the prevalence in individuals aged 60 years or older. | ||
* Females experience 1.5- to 3-fold higher rates than males beginning in early adolescence.<ref name=":1" /> | |||
* Close to 800 000 people die due to suicide every year. Suicide is the second leading cause of death in 15-29-year-olds<ref name=":0" /> | |||
[[File:Prevalence-of-depression-males-vs-females (1).png|center|frameless|740x740px]] | |||
== Symptoms == | |||
Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems and can decrease the persons ability to function at work and at home. | |||
Depression symptoms can vary from mild to severe and can include: | |||
* Feeling sad or having a depressed mood | |||
* Loss of interest or pleasure in activities once enjoyed | |||
* Changes in appetite — weight loss or gain unrelated to dieting | |||
* Trouble [[Sleep Deprivation and Sleep Disorders|sleeping]] or sleeping too much | |||
* Loss of energy or increased fatigue | |||
* Increase in purposeless [[Physical Activity|physical activity]] (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech (these actions must be severe enough to be observable by others) | |||
* Feeling worthless or guilty | |||
* Difficulty thinking, concentrating or making decisions | |||
* Thoughts of death or suicide | |||
Symptoms must last at least two weeks and must represent a change in your previous level of functioning for a diagnosis of depression<ref name=":2" />. | |||
== | === Classification === | ||
[[File:Depression diagram.png|right|frameless|549x549px]] | |||
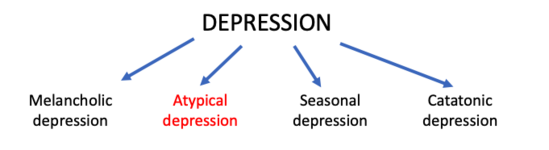
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into: | |||
* Disruptive mood dysregulation disorder | |||
* Major depressive disorder | |||
* Persistent depressive disorder (dysthymia) | |||
* Premenstrual dysphoric disorder | |||
* Depressive disorder due to another medical condition | |||
The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function.<ref name=":1" /> | |||
== | == Treatment == | ||
[[File:Meditation.png|alt=|right|frameless|320x320px]] | |||
Health-care providers should keep in mind the possible adverse effects associated with antidepressant medication, the ability to deliver either intervention (in terms of expertise, and/or treatment availability), and individual preferences. | |||
Treatment can be widely classified into: | |||
# Pharmacological treatment | |||
* Antidepressant medication such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs). | |||
* Antidepressants can be an effective form of treatment for moderate-severe depression but are not the first line of treatment for cases of mild depression. | |||
* They should not be used for treating depression in children and are not the first line of treatment in adolescents, among whom they should be used with extra caution.<ref name=":0" /> | |||
2. Non-pharmacological treatment/ pyschosocial therapy | |||
* are effective in mild depression without antidepressant. | |||
* used side by side with antidepressant in case of moderate and severe depression. | |||
* It includes: | |||
a. Cognitive behavior therapy(CBT) | |||
b. Problem solving therapy (PST) | |||
c. Exercise | |||
d. Socialization | |||
== Outcome Measures == | |||
See [[:Category:Mental Health - Outcome Measures|Category:Mental Health - Outcome Measures]] | |||
== Physical Therapy Management == | |||
One of the biggest things a physical therapist can do for their patients is to be aware of the signs and symptoms of depression and some of the common disorders associated with depression. If the therapist is sensitive to the signs and symptoms of depression they can document it in the plan of care and then notify the physician so the patient can get the appropriate medical treatment, if necessary. Also, because patients with depression may be emotionally unstable, recognizing the signs and symptoms of depression can help you approach different situations and then redirect the patient toward other activities, instructions or more positive topics of conversation. | |||
Physiotherapy management of depression involves a holistic approach that combines physical activity and exercise with psychological support.<ref name=":3">Probst M. Physiotherapy and mental health. Clinical physical therapy. 2017 May 31;230:59-68.</ref> Physical activity has been shown to positively affect mood and mental well-being by increasing the release of endorphins, which are natural mood-boosting chemicals in the brain.<ref>Drannan JD. ''The relationship between physical exercise and job performance: the mediating effects of subjective health and good mood'' (Doctoral dissertation, Bangkok University).</ref> Physical activity can be an effective complementary treatment for individuals with depression.<ref name=":3" /> The American College of Sports Medicine recommends that adults engage in at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days. <ref>Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081.</ref>Additionally, it is important to choose enjoyable and sustainable activities for long-term adherence, such as walking, cycling, swimming, or dancing. Physiotherapists can also incorporate exercise and physical activity into their treatment plans as studies have shown that regular exercise can help alleviate symptoms of depression and improve overall mental health.<ref>Zhao JL, Jiang WT, Wang X, Cai ZD, Liu ZH, Liu GR. Exercise, brain plasticity, and depression. CNS neuroscience & therapeutics. 2020 Sep;26(9):885-95.</ref> Additionally, physiotherapists may use relaxation exercises, breathing exercises, and mindfulness-based interventions to help individuals manage stress and improve their mental health. These interventions can be tailored to the individual's specific needs.<ref name=":3" /> | |||
In addition, physiotherapist can also provide emotional support and encouragement to their patients with depression, which can help improve their overall mental health and well-being. By creating a positive and supportive environment, physical therapists can help their patients feel more comfortable and motivated to continue with their treatment plan. Thus, by promoting a healthy lifestyle, physical therapists can help their patients physically and mentally. | |||
The video looks at evidence on how much exercise is required to get started in order to observe the beneficial effects of exercise in people with depression: | |||
{{#ev:youtube|v=QevFo8wsXZ4|300}} | |||
See [[The Role of Exercise in Preventing and Treating Depression]] | |||
Physical therapists can implement other strategies into their practice to further improve the effects of therapy beyond the benefits of exercise. Research has determined that a further decrease in depression symptoms can be obtained in the clinic by utilizing principles from the following: | |||
*[[Mindfulness]]<ref name="p2">Goodman CC, Fuller KS. The Psychological Spiritual Impact on Health Care. In: 3rd ed: Pathology Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009: 110-115.</ref> | |||
*[[Cognitive Behavioural Therapy]] <ref name="p3">Centers for Disease Control and Prevention. Anxiety and Depression. CDC Features. March 13, 2009. Available at: http://www.cdc.gov/Features /dsBRFSS Depression Anxiety/. Accessed on March 2, 2010.</ref><ref name="p4">Goodman CC, Snyder TK. Pain Types and Viscerogenic Pain Patterns. In: 4th ed: Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis: Saunders Elsevier; 2007: 153-157.</ref> | |||
*Norwegian Psychomotor Physical Therapy <ref name="p5">Jacobsen LN, Lassen IS, Friis P, Videbech P, Licht RW. Bodily symptoms in moderate and severe depression. Nordic Journal of Psychiatry. 2006;60(4):294–8.</ref> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Differential Diagnosis include: | |||
[ | * [[Anaemia]] | ||
* [[Myalgic Encephalomyelitis or Chronic Fatigue Syndrome|Chronic Fatigue syndrome]] | |||
* Dissociative disorders | |||
* Illness anxiety disorders | |||
* Hypoglycemia | |||
* [[Schizophrenia]] | |||
* Somatic symptom disorders<ref name=":1" /> | |||
== References == | == References == | ||
<references /> | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Global Health]] | |||
[[Category:Interventions]] | |||
[[Category: | [[Category:Mental_Health]] | ||
[[Category:Mental Health - Conditions]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Older People/Geriatrics - Conditions]] | |||
[[Category:Non Communicable Diseases]] | |||
Latest revision as of 13:23, 4 August 2023
Original Editors - Nadine Risman from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Nadine Risman, Tessa Larimer, Admin, Lucinda hampton, Kim Jackson, Laura Ritchie, Tolulope Adeniji, Kirenga Bamurange Liliane, Simisola Ajeyalemi, Vidya Acharya, Manisha Shrestha, Elaine Lonnemann, WikiSysop, Amanda Ager, Lauren Lopez, 127.0.0.1, Wendy Walker and Evan Thomas
Introduction[edit | edit source]
Depression causes a persistent feeling of sadness and disinterest, clinical features being sadness, emptiness, and/or irritable mood. These features alongside body and mind changes can seriously affect functional capabilities, and can lead to suicide[1]. Due to false perceptions, nearly 60% of people with depression do not seek medical help. The outcomes for patients with depression are cautious, with the condition having frequent relapses and remissions, leading to a poor quality of life.[2]
This short video provides an overview of what depression actually is including discussion of symptoms, causes, and treatment.
Etiology[edit | edit source]
The etiology of major depression involves many factors, with both genetic, social, lifestyle and environmental factors all playing a role.[2][4]
- First-degree relatives of depressed individuals are about 3 times as likely to develop depression as the general population; however, depression can occur in people without family histories of depression.
- Neurodegenerative diseases (especially Alzheimer disease and Parkinson disease), stroke, multiple sclerosis, seizure disorders, cancer, macular degeneration, and chronic pain have been associated with higher rates of depression.
- Life events and hassles operate as triggers for the development of depression.
- Environmental factors may make some people more vulnerable to depression, for example continuous exposure to violence, neglect, abuse or poverty.[5]
- Traumatic events eg death or loss of a loved one, lack of social support, caregiver burden, financial problems, interpersonal difficulties[2].
Epidemiology[edit | edit source]
Depression is a common illness worldwide, with more than 264 million people affected.[1] Twelve-month prevalence of major depressive disorder is approximately 7%, with marked differences by age group.
- Prevalence in 18- to 29-year-old individuals is threefold higher than the prevalence in individuals aged 60 years or older.
- Females experience 1.5- to 3-fold higher rates than males beginning in early adolescence.[2]
- Close to 800 000 people die due to suicide every year. Suicide is the second leading cause of death in 15-29-year-olds[1]
Symptoms[edit | edit source]
Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems and can decrease the persons ability to function at work and at home.
Depression symptoms can vary from mild to severe and can include:
- Feeling sad or having a depressed mood
- Loss of interest or pleasure in activities once enjoyed
- Changes in appetite — weight loss or gain unrelated to dieting
- Trouble sleeping or sleeping too much
- Loss of energy or increased fatigue
- Increase in purposeless physical activity (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech (these actions must be severe enough to be observable by others)
- Feeling worthless or guilty
- Difficulty thinking, concentrating or making decisions
- Thoughts of death or suicide
Symptoms must last at least two weeks and must represent a change in your previous level of functioning for a diagnosis of depression[5].
Classification[edit | edit source]
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into:
- Disruptive mood dysregulation disorder
- Major depressive disorder
- Persistent depressive disorder (dysthymia)
- Premenstrual dysphoric disorder
- Depressive disorder due to another medical condition
The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function.[2]
Treatment[edit | edit source]
Health-care providers should keep in mind the possible adverse effects associated with antidepressant medication, the ability to deliver either intervention (in terms of expertise, and/or treatment availability), and individual preferences.
Treatment can be widely classified into:
- Pharmacological treatment
- Antidepressant medication such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs).
- Antidepressants can be an effective form of treatment for moderate-severe depression but are not the first line of treatment for cases of mild depression.
- They should not be used for treating depression in children and are not the first line of treatment in adolescents, among whom they should be used with extra caution.[1]
2. Non-pharmacological treatment/ pyschosocial therapy
- are effective in mild depression without antidepressant.
- used side by side with antidepressant in case of moderate and severe depression.
- It includes:
a. Cognitive behavior therapy(CBT)
b. Problem solving therapy (PST)
c. Exercise
d. Socialization
Outcome Measures[edit | edit source]
See Category:Mental Health - Outcome Measures
Physical Therapy Management[edit | edit source]
One of the biggest things a physical therapist can do for their patients is to be aware of the signs and symptoms of depression and some of the common disorders associated with depression. If the therapist is sensitive to the signs and symptoms of depression they can document it in the plan of care and then notify the physician so the patient can get the appropriate medical treatment, if necessary. Also, because patients with depression may be emotionally unstable, recognizing the signs and symptoms of depression can help you approach different situations and then redirect the patient toward other activities, instructions or more positive topics of conversation.
Physiotherapy management of depression involves a holistic approach that combines physical activity and exercise with psychological support.[6] Physical activity has been shown to positively affect mood and mental well-being by increasing the release of endorphins, which are natural mood-boosting chemicals in the brain.[7] Physical activity can be an effective complementary treatment for individuals with depression.[6] The American College of Sports Medicine recommends that adults engage in at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days. [8]Additionally, it is important to choose enjoyable and sustainable activities for long-term adherence, such as walking, cycling, swimming, or dancing. Physiotherapists can also incorporate exercise and physical activity into their treatment plans as studies have shown that regular exercise can help alleviate symptoms of depression and improve overall mental health.[9] Additionally, physiotherapists may use relaxation exercises, breathing exercises, and mindfulness-based interventions to help individuals manage stress and improve their mental health. These interventions can be tailored to the individual's specific needs.[6]
In addition, physiotherapist can also provide emotional support and encouragement to their patients with depression, which can help improve their overall mental health and well-being. By creating a positive and supportive environment, physical therapists can help their patients feel more comfortable and motivated to continue with their treatment plan. Thus, by promoting a healthy lifestyle, physical therapists can help their patients physically and mentally.
The video looks at evidence on how much exercise is required to get started in order to observe the beneficial effects of exercise in people with depression:
See The Role of Exercise in Preventing and Treating Depression
Physical therapists can implement other strategies into their practice to further improve the effects of therapy beyond the benefits of exercise. Research has determined that a further decrease in depression symptoms can be obtained in the clinic by utilizing principles from the following:
- Mindfulness[10]
- Cognitive Behavioural Therapy [11][12]
- Norwegian Psychomotor Physical Therapy [13]
Differential Diagnosis[edit | edit source]
Differential Diagnosis include:
- Anaemia
- Chronic Fatigue syndrome
- Dissociative disorders
- Illness anxiety disorders
- Hypoglycemia
- Schizophrenia
- Somatic symptom disorders[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 WHO Depression Available: https://www.who.int/news-room/fact-sheets/detail/depression (accessed 12.9.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Chand SP, Arif H. Depression. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK430847/ (Accessed, 12/9/2021).
- ↑ Therapist Aid. What is Depression?. Available from: https://www.youtube.com/watch?v=fWFuQR_Wt4M [last accessed 22,1,2023]
- ↑ Better health Depression Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/depression (accessed 12.9.2021)
- ↑ 5.0 5.1 American Psychiatric Association Depression Available: https://www.psychiatry.org/patients-families/depression/what-is-depression(accessed 12.9.2021)
- ↑ 6.0 6.1 6.2 Probst M. Physiotherapy and mental health. Clinical physical therapy. 2017 May 31;230:59-68.
- ↑ Drannan JD. The relationship between physical exercise and job performance: the mediating effects of subjective health and good mood (Doctoral dissertation, Bangkok University).
- ↑ Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081.
- ↑ Zhao JL, Jiang WT, Wang X, Cai ZD, Liu ZH, Liu GR. Exercise, brain plasticity, and depression. CNS neuroscience & therapeutics. 2020 Sep;26(9):885-95.
- ↑ Goodman CC, Fuller KS. The Psychological Spiritual Impact on Health Care. In: 3rd ed: Pathology Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009: 110-115.
- ↑ Centers for Disease Control and Prevention. Anxiety and Depression. CDC Features. March 13, 2009. Available at: http://www.cdc.gov/Features /dsBRFSS Depression Anxiety/. Accessed on March 2, 2010.
- ↑ Goodman CC, Snyder TK. Pain Types and Viscerogenic Pain Patterns. In: 4th ed: Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis: Saunders Elsevier; 2007: 153-157.
- ↑ Jacobsen LN, Lassen IS, Friis P, Videbech P, Licht RW. Bodily symptoms in moderate and severe depression. Nordic Journal of Psychiatry. 2006;60(4):294–8.