Calf Strain: Difference between revisions
No edit summary |
(In the paragraph about muscle testing, I make a reinforcement, adding the use of a force platform.) |
||
| (95 intermediate revisions by 15 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox">'''Original Editor '''- [[User:Kim De Maeght|Kim De Maeght]]- [[User:Bettina Vansintjan|Bettina Vansintjan]]- [[User:Maite Van Roozendael|Maite Van Roozendael]]- [[User:Rewan Aloush|Rewan Aloush]]- [[User:Lenka Pé|Lenka Pé]] | ||
'''Original | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Description == | ||
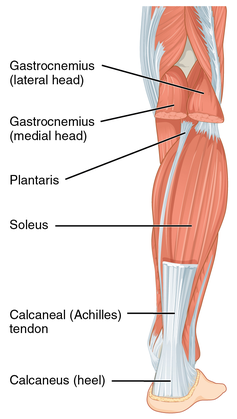
[[File:Posterior leg muscles gastrocnemius soleus plantaris.png|thumb|420x420px|Muscles of the calf complex<ref>Wikimedia Commons contributors, "File:1123 Muscles of the Leg that Move the Foot and Toes b.png," Wikimedia Commons, the free media repository, <nowiki>https://commons.wikimedia.org/w/index.php?title=File:1123_Muscles_of_the_Leg_that_Move_the_Foot_and_Toes_b.png&oldid=276846515</nowiki> (accessed July 25, 2018).</ref>]] | |||
The lower leg is a vital biomechanical element during locomotion, especially during movements that need explosive power and endurance.<ref name=":1">Green B, Pizzari T. [https://bjsm.bmj.com/content/51/16/1189 Calf muscle strain injuries in sport: a systematic review of risk factors for injur]y. British journal of sports medicine. 2017 Aug 1;51(16):1189-94.</ref><ref>Abe T , Fukashiro S , Harada Y , et al . [https://www.jstage.jst.go.jp/article/jpa/20/2/20_2_141/_pdf Relationship between sprint performance and muscle fascicle length in female sprinters]. J Physiol Anthropol Appl Human Sci 2001;20:141–7.</ref> The calf complex is an essential component during locomotive activities and weight-bearing. Injuries to this area impact various sporting disciplines and athletic populations.<ref name=":1" /> Calf muscle strain injuries (CMSI) occur commonly in sports involving high-speed running or increased volumes of running load, acceleration and deceleration as well as during fatiguing conditions of play or performance.<ref name=":1" /><ref name=":3">Bengtsson H, Ekstrand J, Hägglund M. [https://bjsm.bmj.com/content/47/12/743 Muscle injury rates in professional football increase with fixture congestion: an 11-year follow-up of the UEFA Champions League injury study]. British journal of sports medicine. 2013 Aug 1;47(12):743-7.</ref> | |||
< | |||
== | |||
Calf strain | |||
< | |||
Calf strain is a common muscle injury and if not managed appropriately there is a risk of re-injury and prolonged recovery. Muscle strains commonly occur in the medial head of the [[gastrocnemius]] or close to the musculotendinous junction. The gastrocnemius muscle is more susceptible to injury as it is a biarthrodial muscle extending over the knee and ankle. Sudden bursts of acceleration can precipitate injury as well as a sudden eccentric overstretch of the muscle involved.<ref name=":2">Brukner P, Khan K. Clinical sports medicine.3rd ed. Sydney: McGraw Hill, 2006.</ref> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
The "calf" refers to the muscles on the posterior aspect of the lower leg. | |||
<span | <span>It is composed of three muscles:</span> | ||
# <span>[[gastrocnemius]] - <span>in conjunction with [[soleus]], provides primarily plantarflexion of the ankle joint and flexion at the knee joint.</span></span><ref name=":0">Palastanga N, Field D, Soames R. Anatomy and human movement: structure and function. 5th Ed.Edinurgh: Elsevier,2006.</ref><span><ref name="drie">Dixon JB. [https://www.unboundmedicine.com/medline/citation/19468870/Gastrocnemius_vs__soleus_strain:_how_to_differentiate_and_deal_with_calf_muscle_injuries_ Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries]. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):74-7. </ref> <span>Plantarflexion provides the propelling force during gait. Although it spans over two joints, gastrocnemius is not able to exert its maximum power on both joints simultaneously. If the knee is flexed, gastrocnemius cannot produce maximum power at the ankle joint and vice versa.</span></span><ref name=":0" /> | |||
< | # <span>[[soleus]] - <span>is located beneath the gastrocnemius muscle in the superficial posterior compartment of the lower leg.</span></span><span> <span>Its main function is plantar flexion of the ankle and stabilising the tibia on the calcaneus limiting forward sway.</span> <ref name="drie" /></span> | ||
# <span>[[plantaris]] - <span>is located in the posterosuperficial compartment of the calf. </span>Functionally, plantaris is not a major contributor and acts with gastrocnemius as both a flexor of the knee and a plantarflexor of the ankle</span><ref name="p7">Spina AA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1978447/ The plantaris muscle: anatomy, injury, imaging, and treatment]. The Journal of the Canadian Chiropractic Association. 2007 Jul;51(3):158.</ref> | |||
< | |||
<span | |||
< | |||
<span | |||
</span> | |||
<span>These muscles come together to form the [[Achilles Tendon|achilles tendon]] and all three muscles insert into the [[calcaneus]].</span> | |||
== Epidemiology/Etiology == | == Epidemiology/Etiology == | ||
<span | <span>[[Muscle Injuries|Muscle strains]] most commonly occur in bi-articular muscles such as the [[hamstrings]], [[Rectus Femoris|rectus femoris]] and [[gastrocnemius]]. Therefore when we refer to "calf strain" we are often referring to a gastrocnemius strain.</span> | ||
<span | <span>During sporting activities such as sprinting, these long, bi-articular muscles have to cope with high internal forces and rapid changes in muscle length and mode of contraction leading to a higher risk of strain.</span> | ||
< | <span>Despite this, calf muscle strains have also been reported to occur during slow-lengthening muscle actions such as those performed by ballet dancers, but also during common daily activities.<ref name="vijf">Pull MR, Ranson C. [https://www.researchgate.net/publication/246837143_Eccentric_muscle_actions_Implications_for_injury_prevention_and_rehabilitation Eccentric muscle actions: Implications for injury prevention and rehabilitation.] Physical Therapy in Sport. 2007 May 1;8(2):88-97.</ref> </span> | ||
< | Various sports such as rugby, football, tennis, athletics and dancing are impacted by calf muscle strain injuries. In football, 92% of injuries are muscular injuries, 13% of these are calf injuries.<ref name=":3" /> In Australian rules football CMSI represented one of the highest soft tissue injury incidences (3.00 per club per year) and there was a 16% recurrence rate.<ref name=":1" /> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
It is important to | <span>It is important to differentiate between muscle strains within the calf complex in order to formulate a correct prognosis, an appropriate treatment program and prevention of recurrent injury. <ref>Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77. doi:10.1007/s12178-009-9045-8. [L1b]</ref><span> | ||
< | <span>Calf strains are most commonly found in the medial head of the gastrocnemius. <ref name="drie" /> A sudden pain is felt in the calf, and the patient often reports an audible or palpable "pop" in the medial aspect of the posterior calf, or they have a feeling as though someone has kicked them in the back of the leg. Substantial pain and swelling usually develop during the following 24 hours. <ref name="p3">Kwak H-S, Han Y-M, Lee S-Y, Kim K-N, Chung GH. Diagnosis and Follow-up US Evaluation of Ruptures of the Medial Head of the Gastrocnemius (“Tennis Leg”). Korean Journal of Radiology. 2006;7(3):193-198.</ref> Strains in the gastrocnemius are also referred to as a “tennis leg” as the classic presentation was a middle-aged tennis player who suddenly extended the knee. <ref name="drie" /> | ||
== | === Gastrocnemius strain === | ||
<span><span><span>Gastrocnemius is considered at high risk for strains because it crosses two joints (the knee and ankle) and has a high density of type two fast-twitch muscle fibers.<ref name="drie" /> A tear of the medial head of the gastrocnemius muscle is due to an eccentric force being applied to the muscle when the knee is extended and the ankle is dorsiflexed. The gastrocnemius muscle attempts to contract in the already lengthened state leading to tear of the muscle.<ref>Watura C, Harries W. [https://pubmed.ncbi.nlm.nih.gov/21687013/ Isolated tear of the tendon to the medial head of gastrocnemius presenting as a painless lump in the calf.] Case Reports. 2009 Jan 1;2009:bcr0120091468.</ref> </span> | |||
<span>Symptoms of gastrocnemius strain can include subjective reports of sudden sharp pain or tearing sensation at the back of the lower leg, often in the medial belly of the gastrocnemius or at the musculotendinous junction.<ref name=":2" /> | |||
<span><span>On objective assessment there will be<ref name=":2" />: | |||
* <span><span>Tenderness to touch at the point of injury | |||
* <span><span>Swelling | |||
* <span><span>Bruising may appear within hours or days | |||
* <span><span>Stretching of the muscle will reproduce pain | |||
* <span><span>Pain on resisted plantarflexion | |||
=== Soleus strain === | |||
<span>The soleus muscle is injured while the knee is in flexion. Strains of the proximal medial musculotendinous junction are the most common type of soleus muscle injuries. Unlike gastrocnemius, soleus is considered low risk for injury. It crosses only the ankle and is largely comprised of type one slow-twitch muscle fibres. Soleus strains also tend to be less dramatic in clinical presentation and more subacute when compared to injuries of gastrocnemius.<ref name="drie" /></span> This condition frequently occurs in the middle-aged, poorly conditioned and/or physically active patient. <ref name="twee">Flecca D, Tomei A, Ravazzolo N, Martinelli M, Giovagnorio F. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3553076/ US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg)]. Journal of ultrasound. 2007 Dec 1;10(4):194-8.</ref> | |||
The presentation will likely be similar to gastrocnemuis strain however the pain may be slightly more distal and feel deeper subjectively. Injury of the soleus muscle may be under-reported due to a misdiagnosis of thrombophlebitis or lumping of soleus strains with strains of the gastrocnemius. <ref name="drie" /> A soleus strain causes pain when activating the calf muscle or when applying pressure on the Achilles tendon approximately 4 cm above the insertion point on the heel bone or higher up in the calf muscle. Stretching the tendon and walking on tip-toe will also aggravate pain. <ref name="p2">Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.</ref> | |||
=== Plantaris strains === | |||
Plantaris is considered largely vestigial and rarely involved in calf strains, although it crosses both the knee and the ankle joint as well. <ref name="drie" /> Rupture of the plantaris muscle may occur at the myotendinous junction with or without an associated hematoma or partial tear of the medial head of the gastrocnemius muscle or soleus. <ref name="p7" /> Injury to the plantaris muscle can present with similar clinical features as those of the gastrocnemius and soleus muscle. <ref name="p0">Meininger, Alexander K., and Jason L. Koh. "Evaluation of the injured runner." Clinics in sports medicine 31.2 (2012): 203-215.</ref> | |||
<span>Depending on the extent of the injury, the individual may be able to continue exercising although they will have some discomfort and/or tightness during or after activity. Where injuries are more severe, the exact mechanism of injury is easier to recall and/or the individual may be unable to walk due to severe pain. | |||
< | == Grading of calf strains<ref name=":2" /> == | ||
<span>Muscle strains are graded from I to III, with grade III being the most severe. Treatment and rehabilitation depends on the severity of the muscle strain. | |||
{| border="1" cellpadding="2" | |||
|---- | |||
! scope="col" width="width:20em;" |Grade | |||
! scope="col" width="width:20em;" |Symptoms | |||
!Signs | |||
!Average time to return to sport | |||
|- | |||
|I | |||
|Sharp pain at the time of activity or after | |||
May have a feeling of tightness | |||
May be able to continue activity, without pain or with | |||
mild discomfort | |||
Post activity tightness and/or aching | |||
|Pain on unilateral calf raise or hop | |||
|10 - 12 days | |||
|- | |||
|II | |||
|Sharp pain at the time of activity in calf | |||
Unable to continue activity | |||
Significant pain with walking afterwards | |||
May have swelling in muscle | |||
Mild to moderate bruising may be present | |||
|Pain with active plantarflexion | |||
Pain and weakness with resisted | |||
plantarflexion | |||
Loss of dorsiflexion | |||
Bilateral calf raise pain | |||
|16 - 21 days | |||
|- | |||
|III | |||
|Severe and immediate pain in the calf, often at | |||
musculotendinous junction | |||
Unable to continue with activity | |||
May present with considerable bruising and swelling | |||
within hours of injury | |||
|Inability to contract calf muscle | |||
May have palpable defect | |||
Thomson's test positive | |||
|6 months after surgery | |||
|---- | |||
|} | |||
== Differential Diagnosis == | |||
* <span>[[Medial Tibial Stress Syndrome|Medial tibial stress syndrome]] (shin splints) | |||
* <span>[[Achilles Tendinopathy|Achilles tendinopathy]] | |||
* <span>[[Plantar Fasciitis|Plantar fasciopathy]] | |||
* <span>muscles strains and/or joint sprains due to reduced ROM of the ankle. <ref name="zestien">Knight CA., et al. (juni 2001). “Effect of Superficial Heat, Deep Heat, and Active Exercise Warm-up on the Extensibility of the Plantar Flexors.” Physical Therapy, Vol 81 (6), pp. 1206-1214. </ref> | |||
* <span>Other lower leg injuries related to sports with the same symptoms and treatment as a calf strain are discussed below. | |||
* <span>Chronic [[Compartment Syndrome of the Lower Leg|exertional compartment syndrome]] (CECS). <ref name="p9">Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.</ref> CECS begins with mild pain during periods of training and can disappear after training. In the latter stages, pain presents earlier, becoming more painful and of a greater duration forcing a halt in activity. Common complaints are; cramps, paraesthesia, numbness and weakness in the lower leg. CECS is caused by the increased intramuscular blood flow during exercise so compartmental pressure arises, capillaries become compressed and ischemia develops. | |||
* <span>Popliteal Artery Entrapment Syndrome (PAES). An abnormal relationship between the popliteal artery and the surrounding myofascial structures. Functional PAES is caused by muscle contraction, often active plantarflexion of the ankle that compresses the artery between the muscle and underlying bone. <ref name="p8">Stager, Andrew, and Douglas Clement. "Popliteal artery entrapment syndrome." Sports Medicine 28.1 (1999): 61-70.</ref> | |||
* [[Baker's Cyst|Baker's cyst]] | |||
== Assessment == | |||
* Subjective assessment and thorough history should be taken at the initial assessment point | |||
* Objective assessment:<ref name=":5">Marc Roig Pull and Craig Ranson, Eccentric muscle actions: Implications for injury prevention and rehabilitation, Physical Therapy in Sport 8 (2007), no. 2, 88 – 97.</ref><ref name=":6">Dixon JB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2697334/ Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries]. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):74-7. </ref> | |||
** Observation of the foot and ankle in standing and supine | |||
** Ankle AROM | |||
** Ankle PROM | |||
** Palpation of the calf and replication of symptoms | |||
** Resisted strength testing of the foot and ankle complex | |||
** [[Thompson Test|Thompson test]]: to rule out Achilles tendon rupture | |||
** Knee AROM and resisted testing | |||
*{{#ev:youtube|v=kDU1J1kCMhk}}<ref>prohealthsys. Gastrocnemius Muscle Test Vizniak. Available from: https://www.youtube.com/watch?v=kDU1J1kCMhk last accessed [19.09.2017]</ref> | |||
* Imaging: | |||
** [[Ultrasound Scans|Ultrasound]] (US) is considered to be the gold standard. It can also be used to evaluate the degree and extent of the muscular lesion and to exclude other pathologies such as ruptured Baker's cyst and deep vein thrombosis. <ref name="twee" /> | |||
A calf muscle tear is a most common in sports which require quick acceleration and changes in direction such as running, volleyball and tennis, Muscle strains are graded I to III. The more severe the strain, the longer the recovery time. Typical symptoms are stiffness, discoloration and bruising around the strained muscle. <ref name="p2" /> | |||
<br>'''Grade I:''' A first degree or mild injury is the most common and the most minor. A sharp pain is felt at the time of injury or pain with activity. There is little to no loss of strength and range-of-motion with muscle fibre disruption of less than 10%. A return to sport would be expected within 1 to 3 weeks. <ref name="p1">Nsitem V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3845475/ Diagnosis and rehabilitation of gastrocnemius muscle tear: a case report.] The Journal of the Canadian Chiropractic Association. 2013 Dec;57(4):327.</ref> | |||
'''Grade II:''' A second degree or moderate injury is a partial muscle tear halting activity. There is a clear loss of strength and range of motion. <ref name="p1" /> with marked pain, swelling and often bruising. Muscle fibre disruption between 10 and 50%. 3 to 6 weeks is a usual recovery period for a return to full activity. <ref name="p2" /> | |||
'''Grade III:''' A third degree or severe injury results in a complete rupture of the muscle and is often concomitant with a hematoma. <ref name="p1" /> Pain, swelling, tenderness and bruising are usually present. Recovery is highly individualised and can take months before you are fully recovered for a full return to activity. <ref name="p2" /> | |||
'''Rupture:''' is usually associated with the presence of fluid collection between the soleus muscle and the medial head of the gastrocnemius. This can occur with or without haemorrhage. The measurement of fluid collection informs about the extent of the lesion. The degree of the lesion (partial or complete rupture) can be defined by the distance between the two muscles. Axial US scans are the most useful for differentiating between partial and complete rupture, as it is possible to depict the whole muscle belly in one single image. <ref name="twee" /> | |||
[[Thompson Test|<nowiki/>]] | |||
== Medical Management == | == Medical Management == | ||
Calf strains rarely require surgery | Calf strains rarely require surgery however may be necessary in a complete rupture. | ||
Conservative management includes: | |||
# [[Soft Tissue Injuries|Soft tissue injury management]] | |||
# Steroid injection<ref name="p5">Pedret C, Rodas G, Balius R, Capdevila L, Bossy M, Vernooij RW, Alomar X. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622332/ Return to play after soleus muscle injuries.] Orthopaedic journal of sports medicine. 2015 Jul 22;3(7):2325967115595802. </ref> | |||
# Physiotherapy | |||
# If a heamatoma is present, its removal as quickly as possible is essential, otherwise, complications may occur such as myositis ossificans. | |||
# In the case of a more severe injury, a temporary heel pad to shorten the calf muscle to reduce tension in the muscle whilst it heals may be useful. It may be advisable to put heel pads in both shoes, however, to avoid creating a gait imbalance. | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
The | The principal treatment of a calf strain consists of rest and allowing adequate healing time, but in severe cases, surgery is necessary. | ||
Conservative treatment includes gentle passive stretching, isometric then moving onto concentric exercises.<ref name="p5" /> In the latter stages, massage and electrotherapy can be used.<ref name="p7" /> | |||
Initial treatment aims: | |||
* to limit bleeding | |||
* pain | |||
* prevent complications.<ref name="drie" /> | |||
Soft tissue injury management protocols should be started as soon as the injury occurs. [[Peace and Love Principle|PEACE and LOVE]] principles should be applied.<ref>Dubois B, Esculier JF. [https://pubmed.ncbi.nlm.nih.gov/31377722/ Soft-tissue injuries simply need PEACE and LOVE.]</ref> | |||
Other physiotherapy modalities can be used such as: | |||
* Tape or a compressive wrap can be applied and the leg elevated where possible. <ref name="p5" /> | |||
* If major bleeding has occurred, the use of NSAIDs has to be carefully controlled as they have an anti-platelet effect which can increase bleeding, just as the premature application of heat and massage also can. <ref name="drie" /> | |||
* Gentle passive [[stretching]] exercises without pain to maintain range of motion in the plantarflexors. <ref name="p6">Bartholdy C, Zangger G, Hansen L, Ginnerup‐Nielsen E, Bliddal H, Henriksen M. [https://pubmed.ncbi.nlm.nih.gov/26032407/ Local and systemic changes in pain sensitivity after 4 weeks of calf muscle stretching in a nonpainful population: A randomized trial]. Pain Practice. 2016 Jul;16(6):696-703. </ref> In the latter stages, once inflammation has resolved, applying superficial heat simultaneously with a low load static stretch improves the flexibility of muscles.<ref name="p5" /> | |||
* Isotonic exercises for the antagonists tibialis anterior, and the peronei are recommended as well as light exercises for the injured muscle. Gentle movements, within pain limitations, in the first few days following injury will help to promote healing,<ref name="p5" /> | |||
* Shoes with a low heel are recommended to encourage improved heel-toe gait.<ref name="p6" /> | |||
* When the calf muscles can be fully extended pain free, a switch can be made from gentle passive stretching to active stretches, in both a flexed knee position (soleus) and a straightened knee position (gastrocnemius).<ref name="p5" /> | |||
* Gradual loading/strengthening exercises of the calf muscles should be given in order to have a full recovery. The sooner loading exercises are commenced the more rapidly recovery will be. | |||
* Return to sport and specific plyometric exercises should be commenced before full return to sport. | |||
Strains may cause long-lasting pain, despite adequate early treatment. Treatment outcome is successful when: pain is resolved, the calf muscle can be fully extended, strength is back to normal, knee and ankle ROM are normal and when excessive tenderness has disappeared.<ref name="p5" /> | |||
{{#ev:youtube|v=XibsfBav_04}}<ref>AskDoctorJo. Calf pain or strain stretches & exercises. Available from: https://www.youtube.com/watch?v=XibsfBav_04 Last accessed [29.09.2017]</ref> | |||
== Outcome Measures == | |||
*'''[[Lower Extremity Functional Scale (LEFS)|LEFS]]''': Lower Extremity Functional Scale | |||
*'''[[Visual Analogue Scale|VAS]]''': Visual Analogue Scale | |||
*'''[[Numeric Pain Rating Scale|NPRS]]''': Numeric Pain Rating Scale | |||
*'''[[Muscle Strength Testing|Muscle Strength testing]]:''' Regarding muscle strength testing it's important to do it in the most objective way possible. An option for this is using a force platform for the isometric muscle assessment of gastrocnemius and soleus. The differentiation is if you assess strength seated or standing position. In this assessment, we can obtain Maximum Force and the rate of force development ( this last one can be at 150ms or 300 ms). <ref>Mattiussi, A. M., Shaw, J., Cohen, D. D., Price, P., Brown, D. D., Pedlar, C., & Tallent, J. (2022). Reliability, variability, and minimal detectable change of bilateral and unilateral lower extremity isometric force tests. ''Journal of Sport and Exercise Science''.</ref> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Pain in the calf muscle is often due to a strain however there are other conditions which could cause similar symptoms, including deep vein thrombosis and | Pain in the calf muscle is often due to a strain, however, there are other conditions which could cause similar symptoms, including [[Deep Vein Thrombosis|deep vein thrombosis]] and [[Achilles Tendinopathy|achilles tendinopathy]] or [[Achilles Rupture|rupture]]. Healing time is hugely variable depending on the severity of the strain and individual response to treatment. | ||
Conservative management consisting of a graded exercise program usually has the desired outcome for grade I an II strains, but in the case of rupture, surgery is required. Strength and conditioning exercises are essential to re-load the tissues and promote return to activity. | |||
== References == | |||
== References | |||
<references /><br> | <references /><br> | ||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Muscle strain]] | |||
Latest revision as of 21:33, 12 April 2023
Top Contributors - De Maeght Kim, Lynn Leemans, Wanda van Niekerk, Carlos Areia, Abbey Wright, Scott Cornish, Rewan Aloush, Admin, Maite Van Roozendael, Bettina Vansintjan, Yelena Gesthuizen, Sally Ngo, Rachael Lowe, Vidya Acharya, Jan Matthijs, Samuel Adedigba, Esraa Mohamed Abdullzaher, 127.0.0.1, Kim Jackson, Naomi O'Reilly, Ian Carlo Juanico, WikiSysop, Janne Vandenborre and Tony Lowe
Description[edit | edit source]
The lower leg is a vital biomechanical element during locomotion, especially during movements that need explosive power and endurance.[2][3] The calf complex is an essential component during locomotive activities and weight-bearing. Injuries to this area impact various sporting disciplines and athletic populations.[2] Calf muscle strain injuries (CMSI) occur commonly in sports involving high-speed running or increased volumes of running load, acceleration and deceleration as well as during fatiguing conditions of play or performance.[2][4]
Calf strain is a common muscle injury and if not managed appropriately there is a risk of re-injury and prolonged recovery. Muscle strains commonly occur in the medial head of the gastrocnemius or close to the musculotendinous junction. The gastrocnemius muscle is more susceptible to injury as it is a biarthrodial muscle extending over the knee and ankle. Sudden bursts of acceleration can precipitate injury as well as a sudden eccentric overstretch of the muscle involved.[5]
Clinically Relevant Anatomy[edit | edit source]
The "calf" refers to the muscles on the posterior aspect of the lower leg.
It is composed of three muscles:
- gastrocnemius - in conjunction with soleus, provides primarily plantarflexion of the ankle joint and flexion at the knee joint.[6][7] Plantarflexion provides the propelling force during gait. Although it spans over two joints, gastrocnemius is not able to exert its maximum power on both joints simultaneously. If the knee is flexed, gastrocnemius cannot produce maximum power at the ankle joint and vice versa.[6]
- soleus - is located beneath the gastrocnemius muscle in the superficial posterior compartment of the lower leg. Its main function is plantar flexion of the ankle and stabilising the tibia on the calcaneus limiting forward sway. [7]
- plantaris - is located in the posterosuperficial compartment of the calf. Functionally, plantaris is not a major contributor and acts with gastrocnemius as both a flexor of the knee and a plantarflexor of the ankle[8]
These muscles come together to form the achilles tendon and all three muscles insert into the calcaneus.
Epidemiology/Etiology[edit | edit source]
Muscle strains most commonly occur in bi-articular muscles such as the hamstrings, rectus femoris and gastrocnemius. Therefore when we refer to "calf strain" we are often referring to a gastrocnemius strain.
During sporting activities such as sprinting, these long, bi-articular muscles have to cope with high internal forces and rapid changes in muscle length and mode of contraction leading to a higher risk of strain.
Despite this, calf muscle strains have also been reported to occur during slow-lengthening muscle actions such as those performed by ballet dancers, but also during common daily activities.[9]
Various sports such as rugby, football, tennis, athletics and dancing are impacted by calf muscle strain injuries. In football, 92% of injuries are muscular injuries, 13% of these are calf injuries.[4] In Australian rules football CMSI represented one of the highest soft tissue injury incidences (3.00 per club per year) and there was a 16% recurrence rate.[2]
Characteristics/Clinical Presentation[edit | edit source]
It is important to differentiate between muscle strains within the calf complex in order to formulate a correct prognosis, an appropriate treatment program and prevention of recurrent injury. [10]
Calf strains are most commonly found in the medial head of the gastrocnemius. [7] A sudden pain is felt in the calf, and the patient often reports an audible or palpable "pop" in the medial aspect of the posterior calf, or they have a feeling as though someone has kicked them in the back of the leg. Substantial pain and swelling usually develop during the following 24 hours. [11] Strains in the gastrocnemius are also referred to as a “tennis leg” as the classic presentation was a middle-aged tennis player who suddenly extended the knee. [7]
Gastrocnemius strain[edit | edit source]
Gastrocnemius is considered at high risk for strains because it crosses two joints (the knee and ankle) and has a high density of type two fast-twitch muscle fibers.[7] A tear of the medial head of the gastrocnemius muscle is due to an eccentric force being applied to the muscle when the knee is extended and the ankle is dorsiflexed. The gastrocnemius muscle attempts to contract in the already lengthened state leading to tear of the muscle.[12]
Symptoms of gastrocnemius strain can include subjective reports of sudden sharp pain or tearing sensation at the back of the lower leg, often in the medial belly of the gastrocnemius or at the musculotendinous junction.[5]
On objective assessment there will be[5]:
- Tenderness to touch at the point of injury
- Swelling
- Bruising may appear within hours or days
- Stretching of the muscle will reproduce pain
- Pain on resisted plantarflexion
Soleus strain[edit | edit source]
The soleus muscle is injured while the knee is in flexion. Strains of the proximal medial musculotendinous junction are the most common type of soleus muscle injuries. Unlike gastrocnemius, soleus is considered low risk for injury. It crosses only the ankle and is largely comprised of type one slow-twitch muscle fibres. Soleus strains also tend to be less dramatic in clinical presentation and more subacute when compared to injuries of gastrocnemius.[7] This condition frequently occurs in the middle-aged, poorly conditioned and/or physically active patient. [13]
The presentation will likely be similar to gastrocnemuis strain however the pain may be slightly more distal and feel deeper subjectively. Injury of the soleus muscle may be under-reported due to a misdiagnosis of thrombophlebitis or lumping of soleus strains with strains of the gastrocnemius. [7] A soleus strain causes pain when activating the calf muscle or when applying pressure on the Achilles tendon approximately 4 cm above the insertion point on the heel bone or higher up in the calf muscle. Stretching the tendon and walking on tip-toe will also aggravate pain. [14]
Plantaris strains[edit | edit source]
Plantaris is considered largely vestigial and rarely involved in calf strains, although it crosses both the knee and the ankle joint as well. [7] Rupture of the plantaris muscle may occur at the myotendinous junction with or without an associated hematoma or partial tear of the medial head of the gastrocnemius muscle or soleus. [8] Injury to the plantaris muscle can present with similar clinical features as those of the gastrocnemius and soleus muscle. [15]
Depending on the extent of the injury, the individual may be able to continue exercising although they will have some discomfort and/or tightness during or after activity. Where injuries are more severe, the exact mechanism of injury is easier to recall and/or the individual may be unable to walk due to severe pain.
Grading of calf strains[5][edit | edit source]
Muscle strains are graded from I to III, with grade III being the most severe. Treatment and rehabilitation depends on the severity of the muscle strain.
| Grade | Symptoms | Signs | Average time to return to sport |
|---|---|---|---|
| I | Sharp pain at the time of activity or after
May have a feeling of tightness May be able to continue activity, without pain or with mild discomfort Post activity tightness and/or aching |
Pain on unilateral calf raise or hop | 10 - 12 days |
| II | Sharp pain at the time of activity in calf
Unable to continue activity Significant pain with walking afterwards May have swelling in muscle Mild to moderate bruising may be present |
Pain with active plantarflexion
Pain and weakness with resisted plantarflexion Loss of dorsiflexion Bilateral calf raise pain |
16 - 21 days |
| III | Severe and immediate pain in the calf, often at
musculotendinous junction Unable to continue with activity May present with considerable bruising and swelling within hours of injury |
Inability to contract calf muscle
May have palpable defect Thomson's test positive |
6 months after surgery |
Differential Diagnosis[edit | edit source]
- Medial tibial stress syndrome (shin splints)
- Achilles tendinopathy
- Plantar fasciopathy
- muscles strains and/or joint sprains due to reduced ROM of the ankle. [16]
- Other lower leg injuries related to sports with the same symptoms and treatment as a calf strain are discussed below.
- Chronic exertional compartment syndrome (CECS). [17] CECS begins with mild pain during periods of training and can disappear after training. In the latter stages, pain presents earlier, becoming more painful and of a greater duration forcing a halt in activity. Common complaints are; cramps, paraesthesia, numbness and weakness in the lower leg. CECS is caused by the increased intramuscular blood flow during exercise so compartmental pressure arises, capillaries become compressed and ischemia develops.
- Popliteal Artery Entrapment Syndrome (PAES). An abnormal relationship between the popliteal artery and the surrounding myofascial structures. Functional PAES is caused by muscle contraction, often active plantarflexion of the ankle that compresses the artery between the muscle and underlying bone. [18]
- Baker's cyst
Assessment[edit | edit source]
- Subjective assessment and thorough history should be taken at the initial assessment point
- Objective assessment:[19][20]
- Observation of the foot and ankle in standing and supine
- Ankle AROM
- Ankle PROM
- Palpation of the calf and replication of symptoms
- Resisted strength testing of the foot and ankle complex
- Thompson test: to rule out Achilles tendon rupture
- Knee AROM and resisted testing
- [21]
- Imaging:
- Ultrasound (US) is considered to be the gold standard. It can also be used to evaluate the degree and extent of the muscular lesion and to exclude other pathologies such as ruptured Baker's cyst and deep vein thrombosis. [13]
A calf muscle tear is a most common in sports which require quick acceleration and changes in direction such as running, volleyball and tennis, Muscle strains are graded I to III. The more severe the strain, the longer the recovery time. Typical symptoms are stiffness, discoloration and bruising around the strained muscle. [14]
Grade I: A first degree or mild injury is the most common and the most minor. A sharp pain is felt at the time of injury or pain with activity. There is little to no loss of strength and range-of-motion with muscle fibre disruption of less than 10%. A return to sport would be expected within 1 to 3 weeks. [22]
Grade II: A second degree or moderate injury is a partial muscle tear halting activity. There is a clear loss of strength and range of motion. [22] with marked pain, swelling and often bruising. Muscle fibre disruption between 10 and 50%. 3 to 6 weeks is a usual recovery period for a return to full activity. [14]
Grade III: A third degree or severe injury results in a complete rupture of the muscle and is often concomitant with a hematoma. [22] Pain, swelling, tenderness and bruising are usually present. Recovery is highly individualised and can take months before you are fully recovered for a full return to activity. [14]
Rupture: is usually associated with the presence of fluid collection between the soleus muscle and the medial head of the gastrocnemius. This can occur with or without haemorrhage. The measurement of fluid collection informs about the extent of the lesion. The degree of the lesion (partial or complete rupture) can be defined by the distance between the two muscles. Axial US scans are the most useful for differentiating between partial and complete rupture, as it is possible to depict the whole muscle belly in one single image. [13]
Medical Management[edit | edit source]
Calf strains rarely require surgery however may be necessary in a complete rupture.
Conservative management includes:
- Soft tissue injury management
- Steroid injection[23]
- Physiotherapy
- If a heamatoma is present, its removal as quickly as possible is essential, otherwise, complications may occur such as myositis ossificans.
- In the case of a more severe injury, a temporary heel pad to shorten the calf muscle to reduce tension in the muscle whilst it heals may be useful. It may be advisable to put heel pads in both shoes, however, to avoid creating a gait imbalance.
Physical Therapy Management[edit | edit source]
The principal treatment of a calf strain consists of rest and allowing adequate healing time, but in severe cases, surgery is necessary.
Conservative treatment includes gentle passive stretching, isometric then moving onto concentric exercises.[23] In the latter stages, massage and electrotherapy can be used.[8]
Initial treatment aims:
- to limit bleeding
- pain
- prevent complications.[7]
Soft tissue injury management protocols should be started as soon as the injury occurs. PEACE and LOVE principles should be applied.[24]
Other physiotherapy modalities can be used such as:
- Tape or a compressive wrap can be applied and the leg elevated where possible. [23]
- If major bleeding has occurred, the use of NSAIDs has to be carefully controlled as they have an anti-platelet effect which can increase bleeding, just as the premature application of heat and massage also can. [7]
- Gentle passive stretching exercises without pain to maintain range of motion in the plantarflexors. [25] In the latter stages, once inflammation has resolved, applying superficial heat simultaneously with a low load static stretch improves the flexibility of muscles.[23]
- Isotonic exercises for the antagonists tibialis anterior, and the peronei are recommended as well as light exercises for the injured muscle. Gentle movements, within pain limitations, in the first few days following injury will help to promote healing,[23]
- Shoes with a low heel are recommended to encourage improved heel-toe gait.[25]
- When the calf muscles can be fully extended pain free, a switch can be made from gentle passive stretching to active stretches, in both a flexed knee position (soleus) and a straightened knee position (gastrocnemius).[23]
- Gradual loading/strengthening exercises of the calf muscles should be given in order to have a full recovery. The sooner loading exercises are commenced the more rapidly recovery will be.
- Return to sport and specific plyometric exercises should be commenced before full return to sport.
Strains may cause long-lasting pain, despite adequate early treatment. Treatment outcome is successful when: pain is resolved, the calf muscle can be fully extended, strength is back to normal, knee and ankle ROM are normal and when excessive tenderness has disappeared.[23]
Outcome Measures[edit | edit source]
- LEFS: Lower Extremity Functional Scale
- VAS: Visual Analogue Scale
- NPRS: Numeric Pain Rating Scale
- Muscle Strength testing: Regarding muscle strength testing it's important to do it in the most objective way possible. An option for this is using a force platform for the isometric muscle assessment of gastrocnemius and soleus. The differentiation is if you assess strength seated or standing position. In this assessment, we can obtain Maximum Force and the rate of force development ( this last one can be at 150ms or 300 ms). [27]
Clinical Bottom Line[edit | edit source]
Pain in the calf muscle is often due to a strain, however, there are other conditions which could cause similar symptoms, including deep vein thrombosis and achilles tendinopathy or rupture. Healing time is hugely variable depending on the severity of the strain and individual response to treatment.
Conservative management consisting of a graded exercise program usually has the desired outcome for grade I an II strains, but in the case of rupture, surgery is required. Strength and conditioning exercises are essential to re-load the tissues and promote return to activity.
References[edit | edit source]
- ↑ Wikimedia Commons contributors, "File:1123 Muscles of the Leg that Move the Foot and Toes b.png," Wikimedia Commons, the free media repository, https://commons.wikimedia.org/w/index.php?title=File:1123_Muscles_of_the_Leg_that_Move_the_Foot_and_Toes_b.png&oldid=276846515 (accessed July 25, 2018).
- ↑ 2.0 2.1 2.2 2.3 Green B, Pizzari T. Calf muscle strain injuries in sport: a systematic review of risk factors for injury. British journal of sports medicine. 2017 Aug 1;51(16):1189-94.
- ↑ Abe T , Fukashiro S , Harada Y , et al . Relationship between sprint performance and muscle fascicle length in female sprinters. J Physiol Anthropol Appl Human Sci 2001;20:141–7.
- ↑ 4.0 4.1 Bengtsson H, Ekstrand J, Hägglund M. Muscle injury rates in professional football increase with fixture congestion: an 11-year follow-up of the UEFA Champions League injury study. British journal of sports medicine. 2013 Aug 1;47(12):743-7.
- ↑ 5.0 5.1 5.2 5.3 Brukner P, Khan K. Clinical sports medicine.3rd ed. Sydney: McGraw Hill, 2006.
- ↑ 6.0 6.1 Palastanga N, Field D, Soames R. Anatomy and human movement: structure and function. 5th Ed.Edinurgh: Elsevier,2006.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Dixon JB. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):74-7.
- ↑ 8.0 8.1 8.2 Spina AA. The plantaris muscle: anatomy, injury, imaging, and treatment. The Journal of the Canadian Chiropractic Association. 2007 Jul;51(3):158.
- ↑ Pull MR, Ranson C. Eccentric muscle actions: Implications for injury prevention and rehabilitation. Physical Therapy in Sport. 2007 May 1;8(2):88-97.
- ↑ Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77. doi:10.1007/s12178-009-9045-8. [L1b]
- ↑ Kwak H-S, Han Y-M, Lee S-Y, Kim K-N, Chung GH. Diagnosis and Follow-up US Evaluation of Ruptures of the Medial Head of the Gastrocnemius (“Tennis Leg”). Korean Journal of Radiology. 2006;7(3):193-198.
- ↑ Watura C, Harries W. Isolated tear of the tendon to the medial head of gastrocnemius presenting as a painless lump in the calf. Case Reports. 2009 Jan 1;2009:bcr0120091468.
- ↑ 13.0 13.1 13.2 Flecca D, Tomei A, Ravazzolo N, Martinelli M, Giovagnorio F. US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg). Journal of ultrasound. 2007 Dec 1;10(4):194-8.
- ↑ 14.0 14.1 14.2 14.3 Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.
- ↑ Meininger, Alexander K., and Jason L. Koh. "Evaluation of the injured runner." Clinics in sports medicine 31.2 (2012): 203-215.
- ↑ Knight CA., et al. (juni 2001). “Effect of Superficial Heat, Deep Heat, and Active Exercise Warm-up on the Extensibility of the Plantar Flexors.” Physical Therapy, Vol 81 (6), pp. 1206-1214.
- ↑ Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.
- ↑ Stager, Andrew, and Douglas Clement. "Popliteal artery entrapment syndrome." Sports Medicine 28.1 (1999): 61-70.
- ↑ Marc Roig Pull and Craig Ranson, Eccentric muscle actions: Implications for injury prevention and rehabilitation, Physical Therapy in Sport 8 (2007), no. 2, 88 – 97.
- ↑ Dixon JB. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):74-7.
- ↑ prohealthsys. Gastrocnemius Muscle Test Vizniak. Available from: https://www.youtube.com/watch?v=kDU1J1kCMhk last accessed [19.09.2017]
- ↑ 22.0 22.1 22.2 Nsitem V. Diagnosis and rehabilitation of gastrocnemius muscle tear: a case report. The Journal of the Canadian Chiropractic Association. 2013 Dec;57(4):327.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 Pedret C, Rodas G, Balius R, Capdevila L, Bossy M, Vernooij RW, Alomar X. Return to play after soleus muscle injuries. Orthopaedic journal of sports medicine. 2015 Jul 22;3(7):2325967115595802.
- ↑ Dubois B, Esculier JF. Soft-tissue injuries simply need PEACE and LOVE.
- ↑ 25.0 25.1 Bartholdy C, Zangger G, Hansen L, Ginnerup‐Nielsen E, Bliddal H, Henriksen M. Local and systemic changes in pain sensitivity after 4 weeks of calf muscle stretching in a nonpainful population: A randomized trial. Pain Practice. 2016 Jul;16(6):696-703.
- ↑ AskDoctorJo. Calf pain or strain stretches & exercises. Available from: https://www.youtube.com/watch?v=XibsfBav_04 Last accessed [29.09.2017]
- ↑ Mattiussi, A. M., Shaw, J., Cohen, D. D., Price, P., Brown, D. D., Pedlar, C., & Tallent, J. (2022). Reliability, variability, and minimal detectable change of bilateral and unilateral lower extremity isometric force tests. Journal of Sport and Exercise Science.






