NSAID Gastropathy: Difference between revisions
Amanda Huber (talk | contribs) mNo edit summary |
(page link update) |
||
| (41 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Amanda Huber & Emily Sipe | '''Original Editors '''- Amanda Huber & Emily Sipe[[Pathophysiology of Complex Patient Problems| from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
<nowiki/>[[File:Gastropathy.jpeg|right|frameless]]Nonsteroidal anti-inflammatory drugs ([[NSAIDs]]) are the most highly prescribed drugs in the world. Their analgesic, anti-inflammatory, and antipyretic actions may be beneficial; however, they are associated with severe side effects including gastrointestinal injury and peptic ulceration. Though several approaches for limiting these side effects have been adopted, like the use of COX-2 specific drugs, co-medication of acid suppressants like proton pump inhibitors and prostaglandin analogs, these alternatives have limitations in terms of efficacy and cardiovascular effects side effects.<ref name=":0">Sinha M, Gautam L, Shukla PK, Kaur P, Sharma S, Singh TP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3610380/ Current perspectives in NSAID-induced gastropathy. Mediators of inflammation]. 2013 Oct;2013.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3610380/<nowiki/>(accessed 1.11.2021)</ref> | |||
== Current Therapies for Prevention of Gastric Damage == | |||
Several approaches have been adopted for addressing the prevention and cure of the possible side-effects produced by the NSAIDs in the gut. | |||
* Some of these strategies are routinely prescribed to the patients administering NSAIDs. | |||
* Presently, the most common protective strategies adopted are: combination therapy of NSAIDs with gastroprotective agents and; use of selective COX-2 inhibitors.<ref name=":0" /> | |||
==== | == Gastrointestinal Effects == | ||
[[File:GI normal.jpeg|right|frameless]] | |||
The use of NSAIDs is associated with gastrointestinal toxicity, affecting both upper gastrointestinal tract (peptic ulcer disease) and lower gastrointestinal tract (NSAID-induced enteropathy). NSAIDs use has been associated with an increased risk of clinical relapse in inflammatory bowel disease patients. <ref>Hijos-Mallada G, Sostres C, Gomollón F. [https://pubmed.ncbi.nlm.nih.gov/34157367/ NSAIDs, gastrointestinal toxicity and Inflammatory Bowel Disease]. Gastroenterologia y Hepatologia. 2021 Jun 19.Available: https://pubmed.ncbi.nlm.nih.gov/34157367/<nowiki/>(accessed 1.11.2021)</ref> | |||
* Some 10%-50% of patients are unable to tolerate NSAID treatment because of side effects, including abdominal pain, diarrhea, and upset stomach. | |||
* Approximately 15% of patients on long-term NSAID treatment develop a peptic ulcer (ulceration of the stomach or duodenum). | |||
* Even though many of these patients with ulcers do not have symptoms and are unaware of their ulcers, they are at risk of developing serious ulcer complications such as bleeding or perforation of the stomach<ref name=":0" />.<br> | |||
== How do they effect the Gut == | |||
NSAIDs work by stopping the production of prostaglandins (which promote [[Inflammation Acute and Chronic|inflammation]], pain, and fever), they do this do this by blocking cyclooxygenases (COX) enzymes. These [[enzymes]] produce prostaglandins, yet they also protect your stomach and intestinal lining. This is why NSAIDs can damage your gut. <ref name=":1">AMD [https://www.amymyersmd.com/article/nsaids-harm-gut/ 6 Reasons NSAIDs Are Harmful To Your Gut] Available: https://www.amymyersmd.com/article/nsaids-harm-gut/<nowiki/>(accessed 1.11.21)</ref> | |||
Examples of NSAIDS Impact on Gut Health | |||
1. Bacterial Imbalance: Recent research suggest that changes in the [[Gut Brain Axis (GBA)|gut microbiome]] balance are brought on by these medications. Studies show that the combination of medications you ingest are reflected in the types of bacteria that populate your gut. Scientists believe that each type of NSAID can affect different [[Bacterial Infections|bacteria]] in the gut, causing a different imbalance depending on which one you take. Because each person’s gut microbiome is unique, the effects may vary significantly from one person to another. | |||
2. Digestive Discomfort: The most commonly reported side effects of NSAID use are gastrointestinal symptoms, including gas, feeling bloated, stomach pain, constipation and diarrhea because they disrupt the enzymes that protect your gut lining. One study showed that diarrhea due to NSAID use could last for up to six days after their use. | |||
3. Heartburn/[[Gastroesophageal Reflux Disease|GERD]] | |||
4. [[Peptic Ulcers|Gastrointestinal Ulcers]] and Bleeding: approximately 15% of patients who take NSAIDs long-term develop a peptic ulcer. The risk of bleeding ulcers doubles if you take aspirin with other NSAIDs. | |||
5. Leaky Gut: NSAIDS not only cause leaky gut, they can be one of the greatest barriers to recovering from it because they increase your intestinal permeability, which means they make leaky gut worse. | |||
6. Acute Colitis and [[Autoimmune Disorders|Autoimmune Disease]]: NSAIDs may also set off a chain reaction that leads to conditions such as ulcerative colitis and Crohn’s disease. NSAIDs are associated with hospitalizations for severe colitis in patients with inflammatory bowel disease (IBD), and relapses of IBD. This is due to the inflammation that they cause, as well as the leaky gut, which can let through food particles that are so similar to your body’s own cells that your immune system attacks your body<ref name=":1" />. | |||
== Characteristics/Clinical Presentation == | |||
Up to 50% of NSAID induced gastropathy is asymptomatic. <ref name="Roth">Roth S. Coming to terms with nonsteroidal anti-inflammatory drug gastropathy. Drugs(2012, May 7), 72(7): 873-879.</ref> | |||
#Mild dyspepsia | #Mild dyspepsia | ||
| Line 72: | Line 53: | ||
#Exacerbation of existing colon disease | #Exacerbation of existing colon disease | ||
<ref name="Gigante" /><ref name="Roth" /><ref name="Lanza" /> | <ref name="Gigante">Gigante A, Tagarro I. Non-steroidal anti-inflammatory drugs and gastroprotection with proton pump inhibitors: a focus on ketoprofen/omeprazole. Clinical Drug Investigation. (2012, Apr 1),32(4): 221-233.</ref><ref name="Roth" /><ref name="Lanza">Lanza F. A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. The American Journal Of Gastroenterology. (1998, Nov), 93(11): 2037-2046.</ref> | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
* [[Osteoarthritis]] | |||
* [[Rheumatoid Arthritis]] | |||
* [[Ankylosing Spondylitis]] | |||
* Other musculoskeletal conditions | |||
* [[Cardiovascular Disease|Cardiovascular]] Complications | |||
== Systemic Involvement == | == Systemic Involvement == | ||
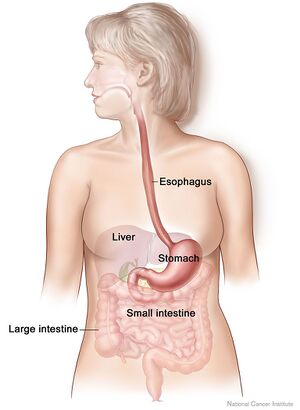
The effects of NSAIDs can occur throughout the GI tract from the esophagus to the colon | The effects of NSAIDs can occur throughout the GI tract from the esophagus to the colon. A potential complication of ulcers left untreated is that the ulcer can perforate through the stomach mucosa and cause infection to spread or the ulcer can erode stomach arteries creating a life-threatening bleed. In addition to effects on the GI system, NSAIDs also affect the renal and cardiovascular systems<ref name="Goodman">Goodman, CC, Snyder, TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis: Saunders Elsevier, 2007.</ref>. | ||
== Management == | |||
One of the difficulties of NSAID gastropathy is that its course is asymptomatic 50% of the time<ref name="Roth" />. Therefore, it is essential that health care professionals assess each patient's risk factors and recommend either discontinued use of an NSAID or inclusion an accompanying cytoprotectant agent in those patients considered high risk. A preventative approach of discontinued NSAID use is recommended over treating the gastropathy<ref name="Roth" />. | One of the difficulties of NSAID gastropathy is that its course is asymptomatic 50% of the time<ref name="Roth" />. Therefore, it is essential that health care professionals assess each patient's risk factors and recommend either discontinued use of an NSAID or inclusion an accompanying cytoprotectant agent in those patients considered high risk. A preventative approach of discontinued NSAID use is recommended over treating the gastropathy<ref name="Roth" />. | ||
If long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) leads to reactive gastropathy, it may be recommend that the client stops taking NSAIDs, take a lower dose, or take a different medicine for pain. It may also be recommend to take a PPI (protein pump inhibitors) along with NSAIDs to prevent or treat reactive gastropathy and its possible complications. | |||
== Physical Therapy Management == | |||
Many of the patients seen in physical therapy will be taking NSAIDs for their disorder. PTs must be aware of risk factors, clinical signs and systems (and be aware the patient may be asymptomatic but still have NSAID induced gastropathy), and they must take a detailed patient history including medication questions concerning multiple NSAIDs, prescription drugs combined with NSAIDs, and changes to medications. Any patient who presents with new onset of back or shoulder pain, who takes NSAIDs, and who presents with signs and symptoms of a peptic ulcer must be referred to the MD.<ref name="Goodman" /> | |||
Risk Factors for NSAID gastropathy (should serve as a red [[The Flag System|flag]]). The incidence of mortality and morbidity from NSAID use is high among the aging population and taking a detailed patient history is essential. | |||
*Age > [[Older People - An Introduction|65 years]] | |||
*History of peptic ulcer or GI disease | |||
*[[Smoking Cessation and Brief Intervention|Smoking]], [[Alcoholism|alcohol]] use | |||
*Oral [[Corticosteroid Medication|corticosteroid]] use | |||
*Anticoagulation or use of other anticoagulants. | |||
*[[Kidney|Renal]] complications in clients with [[hypertension]] or [[Heart Failure|congestive heart failure]] or who use [[diuretics]] or [[ACE Inhibitors: Congestive Heart Failure|ACE]] inhibitors | |||
* | *Use of acid suppressants (H2-receptor antagonists, antacids); these agents can mask the warning symptoms of more serious GI complications, leaving the client unaware of ongoing damage'''<sub></sub>''' | ||
* | *NSAIDs combined with SSRIs | ||
* | |||
''' | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Peptic ulcers are typically caused by ''H. pylori'' infection or acid related consumption and are commonly in young males <ref name="Roth" /> | * Peptic ulcers are typically caused by ''H. pylori'' infection or acid related consumption and are commonly in young males <ref name="Roth" /> | ||
* [[Crohn's Disease]] is a type of inflammatory bowel disease which causes the gastrointestinal tract to be chronically inflamed. Common symptoms of this disease include abdominal pain, diarrhea, blood in the stool and vomiting and can even cause rectal or gastrointestinal bleeding, loss of appetite and liver inflammation. <ref name="Riley">IU health. Riley Hospital for Children: 2013. Available from: http://iuhealth.org/riley/gastroenterology/diseases-conditions/crohns-disease/</ref> | |||
Crohn's Disease is a type of inflammatory bowel disease which causes the gastrointestinal tract to be chronically | * Gastroesophageal Reflux Disease (GERD) is caused by stomach acid back flowing into the esophagus. The most common symptom is heartburn but those with GERD can also have a dry cough, asthma-like symptoms, and trouble swallowing. <ref name="GERD">Berry, J., PhD, APRN. IU Health. Health Encyclopedia. April 2012. Available from: http://iuhealth.staywellsolutionsonline.com/Library/Encyclopedia/85,P00381</ref> | ||
Gastroesophageal Reflux Disease (GERD) is caused by stomach acid back flowing into the esophagus. The most common symptom is heartburn but those with GERD can also have a dry cough, asthma-like symptoms, and trouble swallowing. <ref name="GERD">Berry, J., PhD, APRN. IU Health. Health Encyclopedia. April 2012. Available from: http://iuhealth.staywellsolutionsonline.com/Library/Encyclopedia/85,P00381</ref | |||
== References == | == References == | ||
<references /> <br> | <references /> <br> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]][[Category:Medical]][[Category:Pharmacology]] | ||
Latest revision as of 06:44, 8 February 2023
Original Editors - Amanda Huber & Emily Sipe from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Sipe, Amanda Huber, Lucinda hampton, Admin, Kim Jackson, Elaine Lonnemann, 127.0.0.1, Wendy Walker and Aminat Abolade
Introduction[edit | edit source]
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most highly prescribed drugs in the world. Their analgesic, anti-inflammatory, and antipyretic actions may be beneficial; however, they are associated with severe side effects including gastrointestinal injury and peptic ulceration. Though several approaches for limiting these side effects have been adopted, like the use of COX-2 specific drugs, co-medication of acid suppressants like proton pump inhibitors and prostaglandin analogs, these alternatives have limitations in terms of efficacy and cardiovascular effects side effects.[1]
Current Therapies for Prevention of Gastric Damage[edit | edit source]
Several approaches have been adopted for addressing the prevention and cure of the possible side-effects produced by the NSAIDs in the gut.
- Some of these strategies are routinely prescribed to the patients administering NSAIDs.
- Presently, the most common protective strategies adopted are: combination therapy of NSAIDs with gastroprotective agents and; use of selective COX-2 inhibitors.[1]
Gastrointestinal Effects[edit | edit source]
The use of NSAIDs is associated with gastrointestinal toxicity, affecting both upper gastrointestinal tract (peptic ulcer disease) and lower gastrointestinal tract (NSAID-induced enteropathy). NSAIDs use has been associated with an increased risk of clinical relapse in inflammatory bowel disease patients. [2]
- Some 10%-50% of patients are unable to tolerate NSAID treatment because of side effects, including abdominal pain, diarrhea, and upset stomach.
- Approximately 15% of patients on long-term NSAID treatment develop a peptic ulcer (ulceration of the stomach or duodenum).
- Even though many of these patients with ulcers do not have symptoms and are unaware of their ulcers, they are at risk of developing serious ulcer complications such as bleeding or perforation of the stomach[1].
How do they effect the Gut[edit | edit source]
NSAIDs work by stopping the production of prostaglandins (which promote inflammation, pain, and fever), they do this do this by blocking cyclooxygenases (COX) enzymes. These enzymes produce prostaglandins, yet they also protect your stomach and intestinal lining. This is why NSAIDs can damage your gut. [3]
Examples of NSAIDS Impact on Gut Health
1. Bacterial Imbalance: Recent research suggest that changes in the gut microbiome balance are brought on by these medications. Studies show that the combination of medications you ingest are reflected in the types of bacteria that populate your gut. Scientists believe that each type of NSAID can affect different bacteria in the gut, causing a different imbalance depending on which one you take. Because each person’s gut microbiome is unique, the effects may vary significantly from one person to another.
2. Digestive Discomfort: The most commonly reported side effects of NSAID use are gastrointestinal symptoms, including gas, feeling bloated, stomach pain, constipation and diarrhea because they disrupt the enzymes that protect your gut lining. One study showed that diarrhea due to NSAID use could last for up to six days after their use.
3. Heartburn/GERD
4. Gastrointestinal Ulcers and Bleeding: approximately 15% of patients who take NSAIDs long-term develop a peptic ulcer. The risk of bleeding ulcers doubles if you take aspirin with other NSAIDs.
5. Leaky Gut: NSAIDS not only cause leaky gut, they can be one of the greatest barriers to recovering from it because they increase your intestinal permeability, which means they make leaky gut worse.
6. Acute Colitis and Autoimmune Disease: NSAIDs may also set off a chain reaction that leads to conditions such as ulcerative colitis and Crohn’s disease. NSAIDs are associated with hospitalizations for severe colitis in patients with inflammatory bowel disease (IBD), and relapses of IBD. This is due to the inflammation that they cause, as well as the leaky gut, which can let through food particles that are so similar to your body’s own cells that your immune system attacks your body[3].
Characteristics/Clinical Presentation[edit | edit source]
Up to 50% of NSAID induced gastropathy is asymptomatic. [4]
- Mild dyspepsia
- Heartburn
- Nausea
- Abdominal discomfort
- Erosion
- Ulcers
- Hemorrhage
- Perforation
- Obstruction
- Occult and frank bleeding
- Acute colitis
- Exacerbation of existing colon disease
Associated Co-morbidities[edit | edit source]
- Osteoarthritis
- Rheumatoid Arthritis
- Ankylosing Spondylitis
- Other musculoskeletal conditions
- Cardiovascular Complications
Systemic Involvement[edit | edit source]
The effects of NSAIDs can occur throughout the GI tract from the esophagus to the colon. A potential complication of ulcers left untreated is that the ulcer can perforate through the stomach mucosa and cause infection to spread or the ulcer can erode stomach arteries creating a life-threatening bleed. In addition to effects on the GI system, NSAIDs also affect the renal and cardiovascular systems[7].
Management[edit | edit source]
One of the difficulties of NSAID gastropathy is that its course is asymptomatic 50% of the time[4]. Therefore, it is essential that health care professionals assess each patient's risk factors and recommend either discontinued use of an NSAID or inclusion an accompanying cytoprotectant agent in those patients considered high risk. A preventative approach of discontinued NSAID use is recommended over treating the gastropathy[4].
If long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) leads to reactive gastropathy, it may be recommend that the client stops taking NSAIDs, take a lower dose, or take a different medicine for pain. It may also be recommend to take a PPI (protein pump inhibitors) along with NSAIDs to prevent or treat reactive gastropathy and its possible complications.
Physical Therapy Management[edit | edit source]
Many of the patients seen in physical therapy will be taking NSAIDs for their disorder. PTs must be aware of risk factors, clinical signs and systems (and be aware the patient may be asymptomatic but still have NSAID induced gastropathy), and they must take a detailed patient history including medication questions concerning multiple NSAIDs, prescription drugs combined with NSAIDs, and changes to medications. Any patient who presents with new onset of back or shoulder pain, who takes NSAIDs, and who presents with signs and symptoms of a peptic ulcer must be referred to the MD.[7]
Risk Factors for NSAID gastropathy (should serve as a red flag). The incidence of mortality and morbidity from NSAID use is high among the aging population and taking a detailed patient history is essential.
- Age > 65 years
- History of peptic ulcer or GI disease
- Smoking, alcohol use
- Oral corticosteroid use
- Anticoagulation or use of other anticoagulants.
- Renal complications in clients with hypertension or congestive heart failure or who use diuretics or ACE inhibitors
- Use of acid suppressants (H2-receptor antagonists, antacids); these agents can mask the warning symptoms of more serious GI complications, leaving the client unaware of ongoing damage
- NSAIDs combined with SSRIs
Differential Diagnosis[edit | edit source]
- Peptic ulcers are typically caused by H. pylori infection or acid related consumption and are commonly in young males [4]
- Crohn's Disease is a type of inflammatory bowel disease which causes the gastrointestinal tract to be chronically inflamed. Common symptoms of this disease include abdominal pain, diarrhea, blood in the stool and vomiting and can even cause rectal or gastrointestinal bleeding, loss of appetite and liver inflammation. [8]
- Gastroesophageal Reflux Disease (GERD) is caused by stomach acid back flowing into the esophagus. The most common symptom is heartburn but those with GERD can also have a dry cough, asthma-like symptoms, and trouble swallowing. [9]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Sinha M, Gautam L, Shukla PK, Kaur P, Sharma S, Singh TP. Current perspectives in NSAID-induced gastropathy. Mediators of inflammation. 2013 Oct;2013.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3610380/(accessed 1.11.2021)
- ↑ Hijos-Mallada G, Sostres C, Gomollón F. NSAIDs, gastrointestinal toxicity and Inflammatory Bowel Disease. Gastroenterologia y Hepatologia. 2021 Jun 19.Available: https://pubmed.ncbi.nlm.nih.gov/34157367/(accessed 1.11.2021)
- ↑ 3.0 3.1 AMD 6 Reasons NSAIDs Are Harmful To Your Gut Available: https://www.amymyersmd.com/article/nsaids-harm-gut/(accessed 1.11.21)
- ↑ 4.0 4.1 4.2 4.3 4.4 Roth S. Coming to terms with nonsteroidal anti-inflammatory drug gastropathy. Drugs(2012, May 7), 72(7): 873-879.
- ↑ Gigante A, Tagarro I. Non-steroidal anti-inflammatory drugs and gastroprotection with proton pump inhibitors: a focus on ketoprofen/omeprazole. Clinical Drug Investigation. (2012, Apr 1),32(4): 221-233.
- ↑ Lanza F. A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. The American Journal Of Gastroenterology. (1998, Nov), 93(11): 2037-2046.
- ↑ 7.0 7.1 Goodman, CC, Snyder, TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis: Saunders Elsevier, 2007.
- ↑ IU health. Riley Hospital for Children: 2013. Available from: http://iuhealth.org/riley/gastroenterology/diseases-conditions/crohns-disease/
- ↑ Berry, J., PhD, APRN. IU Health. Health Encyclopedia. April 2012. Available from: http://iuhealth.staywellsolutionsonline.com/Library/Encyclopedia/85,P00381