Osteoporosis: Difference between revisions
Rachael Lowe (talk | contribs) m (Reverted edits by Nikhil Benhur Abburi (talk) to last revision by Kim Jackson) |
No edit summary |
||
| (74 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- Alli Castagno | '''Original Editors '''- [[User:Alli Castagno|Alli Castagno]] and [[User:Christy Kaiser|Christy Kaiser]] [[Pathophysiology of Complex Patient Problems| from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | |||
</div> | |||
== Definition/Description == | |||
[[File:Osteoprosis of Spine.jpg|right|frameless]] | |||
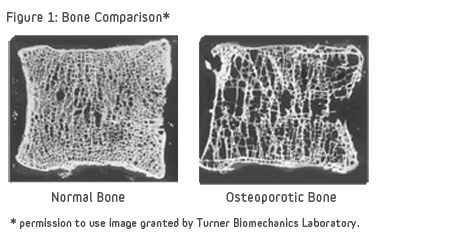
Osteoporosis is defined as low [[Bone Density|bone mineral density]] caused by altered [[bone]] microstructure ultimately predisposing patients to low-impact, [[Osteoporotic Vertebral Fractures|fragility fractures]]. In 2004, the WHO operationally defined osteoporosis based upon the bone mineral density (BMD) assessment of the patient. Thus the current osteoporosis definition is a “BMD that lies 2.5 standard deviations or more below the average value for young healthy women (a T-score of <-2.5 SD).”<ref>World Health Organization. [https://www.who.int/chp/topics/Osteoporosis.pdf WHO scientific group on the assessment of osteoporosis at primary health care level.] Summary meeting report 2004 May 5 (Vol. 5, pp. 5-7).</ref> The WHO definition applies to postmenopausal women and men aged 50 years or older. Although these definitions are necessary to establish the prevalence of osteoporosis, they should not be used as the sole determinant of treatment decisions. This diagnostic classification should not be applied to premenopausal women, men younger than 50 years, or children.<ref>Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. ''Osteoporos Int''. 1994 Nov. 4(6):368-81.</ref> Osteoporosis, in which low bone mass and micro-structural deterioration of bone tissue lead to increased bone fragility, it is a chronic, progressive disease of multifactorial etiology. | |||
In the last 15 years, there has been a movement to base the management of osteoporosis not on the absolute BMD values but to rather consider the [[Fracture Risk Assessment (FRAX) Tool|risk for fracture]] risk in the future<ref name=":4">Paskins Z, Ong T, Armstrong DJ. [https://academic.oup.com/ageing/article/49/3/329/5799034. Bringing osteoporosis up to date: time to address the identity crisis.] Age & Aging. 2020.</ref>. This was fuelled by the fact that most patients with a fragility fracture were not diagnosed with osteoporosis because their BMD did not meet the definition cut-off<ref name=":4" />. | |||
Osteoporotic fractures lead to a significant decrease in [[Quality of Life|quality of life]], with increased morbidity, mortality, and disability. Over 50% of postmenopausal white women will have an osteoporotic-related [[fracture]]. Only 33% of senior women who have a hip fracture will be able to return to independence. In white men, the risk of an osteoporotic fracture is 20%, but the one-year mortality in men who have a [[Femoral Neck Hip Fracture|hip fracture]] is twice that of women. Black males and females have less osteoporosis than their white counterparts, but those diagnosed with osteoporosis have similar fracture risks. The [[Older People - An Introduction|aging]] of the American population is expected to triple the number of osteoporotic [[Fracture|fractures]].<ref name=":1">Joann L. Porter; Matthew Varacallo 19.12.2019 [https://www.ncbi.nlm.nih.gov/books/NBK441901/ Osteoporosis] Available from:https://www.ncbi.nlm.nih.gov/books/NBK441901/ (last accessed 27.2.2020)</ref> | |||
== Associated definitions == | |||
[[Osteopenia]] is defined as a medical condition in which bone tissue's protein and mineral content is reduced, but less severely than in osteoporosis. | |||
[[Sarcopenia]] is a multifactorial syndrome defined as a progressive and generalized loss of skeletal muscle mass and function, with an increased risk of disability, metabolic dysfunction, poor quality of life, and death. <ref>Cannataro R, Carbone L, Petro JL, Cione E, Vargas S, Angulo H, Forero DA, Odriozola-Martínez A, Kreider RB, Bonilla DA. [https://www.mdpi.com/1422-0067/22/18/9724 Sarcopenia: Etiology, nutritional approaches, and miRNAs]. International Journal of Molecular Sciences. 2021 Sep 8;22(18):9724.</ref> | |||
== Etiology == | |||
Bone tissue is constantly being absorbed and replaced throughout one's life span. Bone mass decreases when the rate of absorption increases the rate of production; typically occurring with advanced age. Peak bone mass is met at an average age of 20. Those who develop less bone mass prior to this time, have a high chance of developing osteoporosis.<ref name="mc1">Mayo Clinic. Osteoporosis. http://www.mayoclinic.com/health/osteoporosis/DS00128 (accessed 28 March 2013)</ref> | |||
Primary osteoporosis | === Primary osteoporosis === | ||
Primary osteoporosis has no known definite cause, but there are many contributing factors associated with the disorder. These include prolonged negative calcium balance, impaired gonadal and adrenal function, oestrogen deficiency, or sedentary lifestyle. | |||
==== Types of primary osteoporosis: ==== | |||
* Postmenopausal osteoporosis is associated with increased bone loss due to decreased production of oestrogen.<ref name="patho">Goodman. Fuller. Boissonnault. Pathology; Implications for the Physical Therapist. 2nd. Philadelphia: Saunders, 2003.</ref> Women commonly lose 1% per year after peak bone density has been met, for up to 8 years after menopause.<ref name="mc3">Mayo Clinic. Osteoporosis Causes. http://www.mayoclinic.com/health/osteoporosis/DS00128/DSECTION=causes (accessed 28 March 2013)</ref> | |||
* Senile osteoporosis is an age-related bone loss that often accompanies advanced ageing.<ref name="patho" /> | |||
* Idiopathic juvenile osteoporosis | |||
== | === Secondary osteoporosis === | ||
Secondary osteoporosis is caused by prolonged use of medications or secondary to another disease or condition which inhibits the absorption of calcium or impedes the body's ability to produce bone.<ref name="patho" /> | |||
Low calcium intake or absorption can greatly increase one's risk of developing osteoporosis. Life-long calcium intake is crucial in building up bone stock prior to peak levels of bone mass, as well as to maintain bone mass after the age of 20. Excessive alcohol consumption can decrease the body's ability to absorb calcium.<ref name="mc2">Mayo Clinic. Osteoporosis: Risk Factors. http://www.mayoclinic.com/health/osteoporosis/DS00128/DSECTION=risk%2Dfactors (accessed 28 March 2013)</ref> | |||
< | Bone responds to the load applied to it. [[Physical Activity|Physically active]] individuals typically have higher bone density, than those who have a sedentary lifestyle.<ref name="mc2" /> | ||
[[Hormones|Hormone]] levels, either too little or too much, can impede the body's ability to produce and maintain adequate bone mass. Dysfunction with sex glands, thyroid, parathyroid, or adrenal glands is often associated with osteoporosis. <ref name="mc2" /> | |||
==== Types of secondary osteoporosis ==== | |||
* Endocrine origin | |||
** Hypogonadism/Hypogonadal state | |||
** Hypercortisolism | |||
** [[Hyperthyroidism]] | |||
** Hyperparathyroidism | |||
** Hyperprolactinemia | |||
** [[Diabetes|Diabetes mellitus]] | |||
* Gastrointestinal diseases | |||
** Chronic inflammatory bowel disease | |||
** Malabsorption/Deficiences | |||
** Malnutrition | |||
** [[Liver Disease|Primary biliary cirrhosis]] | |||
** Lactose intolerance | |||
* Rheumatological and [[Connective Tissue Disorders|connective tissue diseases]] | |||
* Inflammatory diseases | |||
* Hematological and neoplastic disorders | |||
* Medications - eg.Glucocorticoids, Chemotherapeutic/transplant drugs, Anticonvulsants | |||
* Immobilisation | |||
* Chronic [[alcoholism]] | |||
* Organ Transplantation | |||
* Genetic/congenital - eg. Marfan syndrome, Osteogenesis imperfecta, Glycogen storage disease, etc. | |||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|F1KJq6Pdp54}} <div class="text-right"><ref>Amgen. Osteoporosis 101: What is Osteoporosis and What You Need to Know. Available from: https://youtu.be/F1KJq6Pdp54 [last accessed 30/10/2020]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|c5tc01WFYks}} <div class="text-right"><ref>Amgen. Postmenopausal Osteoporosis. Available from: https://youtu.be/c5tc01WFYks [last accessed 30/10/2020]</ref></div></div> | |||
</div> | |||
== | == Risk Factors == | ||
Risk factors for osteoporosis include the following<ref>Lyles KW, Schenck AP, Colón-Emeric CS. Hip and other osteoporotic fractures increase the risk of subsequent fractures in nursing home residents. Osteoporosis international. 2008 Aug;19(8):1225-33.</ref> : | |||
* Advanced age (≥50 years) | |||
* Female sex | |||
* White or Asian ethnicity | |||
* Genetic factors, such as a family history of osteoporosis | |||
* Thin build or small stature (eg, bodyweight less than 127 lb [57.6 kg]) | |||
* Amenorrhea | |||
* Late menarche | |||
* Early menopause | |||
* Postmenopausal state | |||
* Physical inactivity or immobilization | |||
* Use of certain drugs (eg, anticonvulsants, systemic steroids, thyroid supplements, heparin, chemotherapeutic agents, insulin) | |||
* Alcohol and tobacco use | |||
* Androgen or estrogen deficiency | |||
* Calcium or vitamin D deficiency | |||
* Dowager hump | |||
== | == Epidemiology == | ||
Over 200 million people have osteoporosis and the incidence rate increases with age. | |||
* Over 70% of those over age 80 are affected | |||
* It is more common in females than in males <ref>Rosen CJ. [https://www.ncbi.nlm.nih.gov/books/NBK279134/ The epidemiology and pathogenesis of osteoporosis]. Endotext [Internet]. 2020 Jun 21.</ref> | |||
* In the developed world, 2% to 8% of males and 9% to 38% of females are affected | |||
* Worldwide, there are approximately 9 million fractures per year as a result of osteoporosis | |||
* 1 in 3 females and 1 in 5 males over the age of 50 will have an osteoporotic fracture | |||
* Areas of the world with less [[Vitamin D Deficiency|Vitamin D]] through sunlight compared to regions closer to the equator have higher fracture rates in comparison to people living at lower latitudes<ref name=":1" /> | |||
* In the United States alone, approximately 10 million individuals are estimated to already have the disease and 34 million at increased risk for osteoporosis.<ref name=":0">National Osteoporosis Foundation Report Finds Patient-Centered Care Is Key Element in Delivering High-Quality, High-Value Treatment. 2019. Available from: https://www.nof.org/news/national-osteoporosis-foundation-report-finds-patient-centered-care-is-key-element-in-delivering-high-quality-high-value-treatment/ (accessed 14 October 2019) | |||
</ref> 55% of Americans over the age of 50 have the disorder<ref name=":0" /> | |||
== Diagnosis == | |||
Patients with a diagnosis of osteoporosis should have: | |||
* Laboratory assessment of their renal and thyroid function, a 25-hydroxyvitamin D and calcium level | |||
* [[DEXA Scan|DEXA scan]] - the World Health Organization (WHO) established that dual x-ray absorptiometry tests scans (DEXA) of the central skeleton is the best test for assessing bone mineral density | |||
** Scores between negative 1 and negative 2.5 reflect a diagnosis of osteopenia | |||
** Scores below negative 2.5 reflect a diagnosis of osteoporosis | |||
* The [[FRAX tool|Fracture Risk Assessment Tool]] (FRAX) has become a more accurate way to measure 10years fracture probability. The FRAX questionnaire takes into account elements that influence an individual's bone quality as well as his/her bone density. <ref name="patho" /> To learn more about FRAX [http://blog.melioguide.com/physical-therapy-continuing-education/frax-tutorial-for-health-professionals/ view this tutorial] | |||
* The Garvan Fracture Risk Calculator with BMD | |||
* Conventional radiography is used for the qualitative and semiquantitative evaluation | |||
* Secondary tests for screening of secondary osteoporosis to determine causes of osteoporosis like 24-Hour urine calcium level, Parathyroid Hormone levels, Testosterone and gonadotropin levels in younger men with low bone densities, serum markers of osteoclasts/osteoblasts, etc. | |||
== Characteristics/Clinical Presentation == | |||
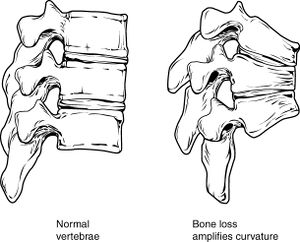
The physical exam rarely reveals any changes until osteoporosis is quite advanced. At that point, loss of height and [[Thoracic Hyperkyphosis|kyphosis]] is evident from [[Osteoporotic Vertebral Fractures|vertebral fractures.]] | |||
In healthy individuals without risk factors, experts recommend: | |||
* Start to screen women at the age of 65 years and men at the age of 70 | |||
* Patients with risk factors or a high score on an osteoporosis risk assessment test should be screened sooner<ref name=":1" /> | |||
[[File:Bone Comparison of Healthy and Osteoporotic Vertibrae.png|right|frameless|474x474px]] | |||
Clinical Signs and Symptoms | |||
*Back pain: Episodic, acute low thoracic/high lumbar pain | *[[Low Back Pain|Back pain]]: Episodic, acute low thoracic/high lumbar pain | ||
*Compression fracture of the spine | *Compression fracture of the spine | ||
*Bone fractures | *Bone fractures | ||
*Decrease in height | *Decrease in height | ||
*Kyphosis | *[[Kyphosis]] | ||
*Dowager’s hump | *Dowager’s hump | ||
*Decreased activity tolerance | *Decreased activity tolerance | ||
*Early satiety< | *Early satiety<ref name="dd">Goodman. Snyder. Differential Diagnosis for Physical Therapists; Screening for Referral. 4th. St.Louis: Saunders, 2007.</ref> | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
As many diseases increase an individual's risk of osteoporosis, they also may be seen as comorbidities.<ref name="dd" / | As many diseases increase an individual's risk of osteoporosis, they also may be seen as comorbidities.<ref name="dd" /> | ||
*Eating disorders | *[[Anorexia Nervosa|Eating disorders]] | ||
*Cancer and cancer treatment | *[[Cancer Rehabilitation and the Importance of Balance Training|Cancer]] and cancer treatment | ||
*Chronic renal failure | *[[Chronic Kidney Disease|Chronic renal failure]] | ||
*Osteogenesis imperfect | *[[Osteogenesis Imperfecta|Osteogenesis imperfect]] | ||
*Rheumatic diseases | *[[Rheumatoid Arthritis|Rheumatic]] diseases | ||
*Chronic pulmonary disease | *Chronic pulmonary disease | ||
*Cushing’s Disease | *[[Cushing's Syndrome|Cushing’s]] Disease | ||
*Male hypogonadism | *Male hypogonadism | ||
*Hypothyroidism | *[[Hypothyroidism]] | ||
*Hyperparathyroidism | *[[Hyperparathyroidism]] | ||
*Type 2 Diabetes Mellitus | *Type 2 [[Diabetes Mellitus Type 2|Diabetes Mellitus]] | ||
*Gastrointestinal Disease | *Gastrointestinal Disease | ||
*Hepatic disease<span id="1364846108836E" style="display: none;"> </span> | *[[Liver Disease|Hepatic disease<span id="1364846108836E" style="display: none;"> </span>]] | ||
=== | == Medicines for Osteoporosis == | ||
Osteoporosis medicines can increase bone density and while the increases may appear small this can have a very positive effect on reducing fracture rates. For example, medication can increase bone density in the hip by approx. 1-3% and in the spine by 4-8%, over the first 3-4years of treatment. Medication can reduce spinal fractures by around 30-70% and [[Femoral Neck Hip Fracture|hip fractures]] by 30-50% (a positive effect can be seen as early as 6 – 12 months after starting treatment). | |||
[[File:Pill banner.png|right|frameless]] | |||
Osteoporosis medicines are grouped into different 'classes' depending on their 'active ingredient' | |||
#Bisphosphonates - Tablets (daily, weekly or monthly): Alendronate (brand name Fosamax, or other generic brands), Risedronate (brand name Actonel, or other generic brands), once yearly intravenous infusion: Zoledronic acid (brand name Aclasta) | |||
#Denosumab - 6 monthly injection: Denosumab (brand name: Prolia)<br>Denosumab works in a different way to bisphosphonates, but has the same effect of slowing the rate at which bone is broken down, with similar reductions in the risk of fracture. | |||
#Selective oestrogen receptor modulators (SERMS) - Daily tablet: Raloxifene (brand name: Evista) | |||
#* This medicine acts on bones in a similar way to that of the hormone oestrogen, slowing bone loss and reducing the risk of spinal fractures in women who have been through menopause | |||
#Hormone replacement therapy (HRT) - The active ingredient is the hormone oestrogen. Some HRT treatments also contain progestogen (combined HRT) | |||
#* Even at low doses, HRT helps to slow bone loss, reducing the risk of osteoporosis and fractures in women who have gone through menopause. HRT is safe and effective for most women under the age of 60 who have osteoporosis and who also need hormonal treatment to relieve the symptoms of menopause. It may also be prescribed for women under 60 who are unable to take other osteoporosis medicines. It is particularly useful for women who have undergone early menopause (before 45 years of age) | |||
#* Due to the small increased risk of heart disease, strokes and breast cancer in older women, other osteoporosis medicines are more suitable for women over the age of 60 | |||
#Teriparatide - Daily injection for 18 months (self-administered): Teriparatide (Brand name: Forteo) | |||
#* This medicine stimulates bone-forming cells, resulting in improved bone strength and structure. It is only prescribed for people with severe osteoporosis when other osteoporosis medicines have not worked and the risk of more fractures is still very high. Teriparatide must be prescribed by a specialist and can only be taken for 18 months. Once the course of teriparatide is finished, another osteoporosis medicine must be started to ensure that the new bone formed is maintained and improved<ref>Osteoporosis Australia. [https://www.osteoporosis.org.au/treatment-options Treatment options] Available from:https://www.osteoporosis.org.au/treatment-options (last accessed 27.2.2020)</ref> | |||
#Romosozumab - monthly injection: Romosozumab (brand name: Evenity) | |||
#*This medicine is a monoclonal antibody that binds and inhibits sclerostin, with a dual effect of increasing bone formation and decreasing bone resorption.<ref>Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CA, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A. [https://pubmed.ncbi.nlm.nih.gov/27641143/ Romosozumab Treatment in Postmenopausal Women with Osteoporosis.] N Engl J Med. 2016 Oct 20;375(16):1532-1543.</ref><ref>McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, Langdahl BL, Reginster JY, Zanchetta JR, Wasserman SM, Katz L, Maddox J, Yang YC, Libanati C, Bone HG. [https://pubmed.ncbi.nlm.nih.gov/24382002/ Romosozumab in postmenopausal women with low bone mineral density.] N Engl J Med. 2014 Jan 30;370(5):412-20.</ref> | |||
[[File:Smoking-1026556 960 720-2.jpg|right|frameless|250x250px]] | |||
Take note - Medical management isn't the only way to treat osteoporosis. It is also important to include daily exercise, good [[nutrition]] (including adequate amounts of calcium and [[Vitamin D Deficiency|vitamin D]]), smoking cessation, and limiting alcohol intake.<ref name="mayo">Mayo Clinic. Osteoporosis treatment: Medication can help. http://www.mayoclinic.com/health/osteoporosis-treatment/WO00127 (Accessed 28 March 2013).</ref><br> | |||
== Physical Therapy Management == | |||
* | |||
* | |||
* | |||
* | |||
Medical management isn't the only way to treat osteoporosis. It is also important to include daily exercise, good nutrition (including | |||
== Physical Therapy Management | |||
Physical therapy intervention for individuals with osteoporosis, or even osteopenia, should include: | Physical therapy intervention for individuals with osteoporosis, or even osteopenia, should include: | ||
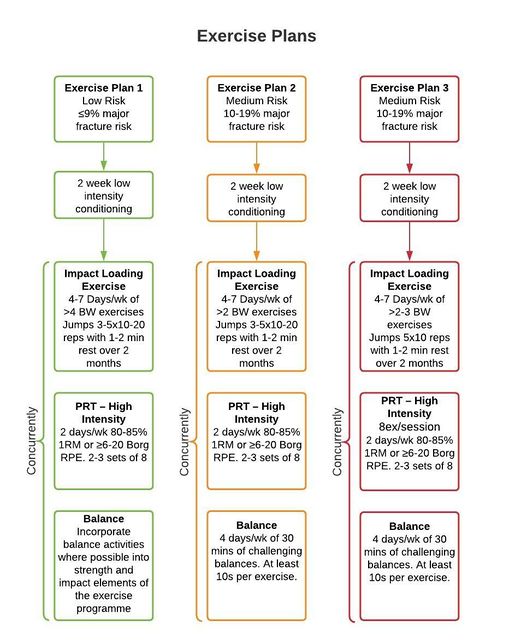
#Weight-bearing exercises | |||
#* Exercises such as walking or hopping, has been shown to maintain or improve bone density in this population | |||
#* Strengthening exercises, using weights or resistance bands, have also been shown to maintain or improve bone density at the location of the targeted muscle attachments | |||
#* Maintaining bone health in this population is extremely important, especially in the elderly as there is typically has a decline in bone mass with age<ref>Zehnacker CH, Bemis‐Dougherty A. Effect of Weighted Exercises on Bone Mineral Density in Post Menopausal Women A Systematic Review. Journal of Geriatric Physical Therapy. 2007; 30(2):79-88.</ref> | |||
#Flexibility and [[Strength Training versus Power Training|strengthening]] exercise | |||
#*These can help improve the individual's overall physical function and postural control. eg [[Tai Chi and the Older Person|Tai chi]], [[Yoga]] | |||
#* Improving postural control is important to reduce the risk of [[Falls in elderly|falls]] | |||
#* Falls often result in fractures in frail individuals | |||
#* Balance exercises are also important to incorporate to further reduce the risk of falls.<ref name="burke">Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. [https://pubmed.ncbi.nlm.nih.gov/22498664/ Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial.] Clinical Rehabilitation; 26 (11): 1021-1031.</ref> eg [[Otago Exercise Programme|Otago]] Programme | |||
# [[Posture|Postural]] exercise | |||
#*These are crucial to prevent structural changes that often accompany osteoporosis, such as thoracic kyphosis | |||
#* Every osteoporosis program should include extension exercises; chin tucks, scapular retractions, thoracic extensions, and hip extensions | |||
#* Strengthening the extensor muscles will promote improved posture and improved balance | |||
#* Flexion exercises are CONTRAINDICATED especially in patients with a risk of a spinal fracture. Anterior compressive forces to the vertebra can contribute to compression fractures<ref name="patho" />. Flexion and twisting place a high compressive load on the vertebral bodies, these high levels should be avoided <ref>Bonner Jr FJ, Sinaki M, Grabois M, Shipp KM, Lane JM, Lindsay R, Gold DT, Cosman F, Bouxsein ML, Weinstein JN, Gallagher RM. [https://www.researchgate.net/profile/Deborah_Gold/publication/10749063_Health_Professional's_Guide_to_Rehabilitation_of_the_Patient_with_Osteoporosis/links/0912f50454de2c1f48000000.pdf Health professional's guide to rehabilitation of the patient with osteoporosis]. Osteoporosis International. 2003 May 1;14:S1.</ref>. | |||
# [[Balance]] exercise | |||
# Education - top tips easily given to clients | |||
#*Follow a healthy diet that includes enough calcium and Vitamin D | |||
#* Wear sensible, well-fitting shoes to avoid falls | |||
#* Avoid rugs and sloppy slippers – both can cause trips | |||
#* Have good lighting on stairs | |||
#* Get eyesight checked regularly | |||
#* Try to avoid heavy lifting – consider home delivery grocery shopping | |||
#Back pain | |||
#*Physiotherapists may treat patients with osteoporosis for back pain | |||
#* Agility training, resistance training, and stretching have all been shown to decrease back pain and its related disabilities in this population<ref name="ambrose">Liu-Ambrose TY, Khan KM, Eng JJ, Lord SR, Lentle B, McKay HA. [https://pubmed.ncbi.nlm.nih.gov/15702262/ Both resistance and agility training reduce back pain and improve health-related quality of life in older women with low bone mass.] Osteoporos Int. 2005 Nov;16(11):1321-9.</ref> | |||
#High-intensity training - Research highly supports high-intensity training in the prevention of bone loss for women in menopausal years and the early post-menopausal period | |||
#* High-intensity training would include body-weight and resistive exercises at a high-intensity, similar to circuit training.<ref name="martyn">Martyn-St James M, Carroll S. [https://pubmed.ncbi.nlm.nih.gov/16823548/ High Intensity resistance training and postmenopausal bone loss: a meta-analysis.] Osteoporosis International; 17: 1225-1240.</ref> This type of training is often contraindicated for individuals with low bone mass | |||
#* Dynamic weight-bearing, high force exercise results with the greatest improvements at the femoral neck and moderate results at the femoral trochanter | |||
#* Dynamic weight-bearing, low force exercise had moderate positive effects on the spine | |||
#* Non-weight-bearing, high force exercises were shown to have moderate effects on the femoral neck<ref name="cochrane">Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. [https://pubmed.ncbi.nlm.nih.gov/21735380/ Exercise for preventing and treating osteoporosis in postmenopausal women.] The Cochrane Collaboration. 2011;(2). </ref> | |||
[[File:Osteoporosis Exercise plan.jpg|center|645x645px]]<div class="text-center">Adapted exercise plan diagram<ref>Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane database of systematic reviews. 2011(11).</ref> <ref>Beck BR, Daly RM, Singh MA, Taaffe DR. Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of science and medicine in sport. 2017 May 1;20(5):438-45.</ref></div> | |||
== Clinical Considerations == | |||
* ''Manipulations:'' A strong precaution should be taken before performing manual techniques such as manipulations or joint assessments that may increase an individual's risk for fractures, especially in the spine | |||
* ''Body Weight Supported Treadmill Training:'' It is contraindicated to use body-weight supported treadmill training with individuals who have severe osteoporosis or lower extremity, pelvic, or rib fracture. Severe osteoporosis is considered a T-score greater than 2.5<ref name="guide">U.S. Department of Health & Human Services. National Guideline Clearing House. Best evidence statement (BESt). Intensive partial body weight supported treadmill training. http://guideline.gov/content.aspx?id=24531&search=Gait+training+procedure+ (accessed 28 March 2013)</ref> | |||
* Plyometrics and balance exercises should be performed with care and precaution to prevent falls and fractures. | |||
=== | == Dietary Management == | ||
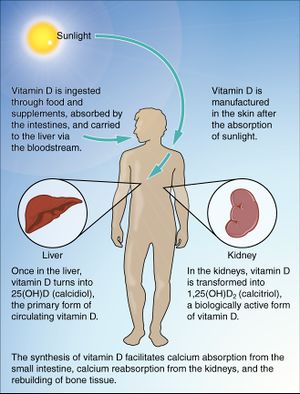
* [[File:Vitamin D.jpg|right|frameless]]The most important nutrients for people with osteoporosis are calcium and vitamin D. Calcium is a key building block for bones. Vitamin D helps the body to absorb calcium. | |||
* Calcium can be from diet, supplements, or both (it is best to get these nutrients from food, rather than supplements) | |||
** For adults aged 50 and older, the National Osteoporosis Foundation of the USA has recommended intake is 1000–1200 mg/day of elemental calcium. <ref name=":2" /><ref name=":3" /> | |||
* Optimal vitamin D can be acquired 3 ways: | |||
** Eating foods that naturally contain vitamin D or are fortified with vitamin D | |||
** Sensible sun exposure | |||
*** A few minutes, regularly, with good skin exposure, no sun cream and your shadow should be shorter than you. If it is longer than you are, you are not producing any vitamin D<ref>Zielinska-Dabkowska KM. Vitamin D. The truth about Vitamin D and sun exposure demystified. Finding the balance for personal health.</ref> | |||
** Taking a vitamin D supplement | |||
*** For adults aged 50 and older, the National Osteoporosis Foundation of the USA has recommended intake is 700–800 IU/day <ref name=":2">Muscogiuri G, Altieri B, Annweiler C, Balercia G, Pal HB, Boucher BJ, Cannell JJ, Foresta C, Grübler MR, Kotsa K, Mascitelli L. Vitamin D and chronic diseases: the current state of the art. Archives of toxicology. 2017 Jan;91(1):97-107.</ref><ref name=":3">Wacker M, Holick MF. Sunlight and Vitamin D: A global perspective for health. Dermato-endocrinology. 2013 Jan 1;5(1):51-108.</ref> | |||
== Team Work == | |||
Osteoporosis is a major public health problem affecting millions of elderly individuals. Besides causing fractures, the disorder leads to severe psychosocial and financial consequences for the patient. The condition has many risk factors and is best managed by an interprofessional team of healthcare workers. | |||
* Patient education is vital as many are unaware of the serious consequences of the disorder. Early prevention can help reduce the high morbidity | |||
* Attending physiotherapy for exercise prescription and participation in a supervised exercise programme is recommended | |||
* Patients should be urged to modify their lifestyle and remain compliant with the medications prescribed | |||
* The patient should be urged to quit smoking and abstain from alcohol | |||
* The dietitian should educate the patient on a calcium-rich diet and the need to take vitamin D supplements | |||
* The pharmacist should assist the team by educating the patient about the benefits of bisphosphonates and their adverse effects | |||
* Women over the age of 65 should be urged to have a bone density scan<ref name=":1" /><br><br> | |||
== Conclusion == | |||
*Osteoporosis is a common and silent disease until it is complicated by fractures | |||
== | * It is estimated that 50% of women and 20% of men over the age of 50 years will develop an osteoporosis-related fracture at some stage | ||
* These fractures are responsible for lasting disability, impaired quality of life, and increased mortality, with enormous medical and heavy personnel burden on both the patient’s and the nation’s economy | |||
* Osteoporosis can be diagnosed and prevented with effective treatments before fractures occur | |||
* The prevention, detection, and treatment of osteoporosis is important <ref>Sözen T, Özışık L, Başaran NÇ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335887/ An overview and management of osteoporosis.] European journal of rheumatology. 2017 Mar;4(1):46.</ref> | |||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
The Effects of Whole Body Vibration on Bone Mineral Density for a Person with a Spinal Cord Injury: A Case Study | [https://core.ac.uk/reader/61745056?utm_source=linkout The Effects of Whole Body Vibration on Bone Mineral Density for a Person with a Spinal Cord Injury: A Case Study] | ||
[http://web.ebscohost.com/ehost/pdfviewer/pdfviewer?sid=3b623171-c43b-4552-a1a2-8a5f00983206%40sessionmgr15&vid=5&hid=22 Asymmetric lower-limb bone loss after spinal cord injury: Case report] | |||
== Resources == | == Resources == | ||
[http://www.nof.org/ National Osteoporosis Foundation] | |||
[http://www.physther.org/content/67/7/1100.full.pdf Journal of the American Physical Therapy Association] | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Medical]] | |||
[[Category:Metabolic/Endocrine|Endocrine]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Womens Health]] | |||
[[Category:Conditions]] | |||
[[Category:Older People/Geriatrics - Conditions]] | |||
[[Category:Non Communicable Diseases]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
[http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000333.pub2/abstract Cochrane Review] | |||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 00:31, 27 December 2022
Original Editors - Alli Castagno and Christy Kaiser from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Alli Castagno, Christy Kaiser, Kim Jackson, Admin, Carin Hunter, Lucinda hampton, Elaine Lonnemann, Wataru Okuyama, Nikhil Benhur Abburi, Tarina van der Stockt, Rotimi Alao, Margaret Martin, Ewa Jaraczewska, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Scott Buxton, WikiSysop, 127.0.0.1, Tony Lowe, Vidya Acharya, Wanda van Niekerk, Hardik Bhatt, Ajay Upadhyay, Shreya Pavaskar, De Maeght Kim, Ward dirk Merckx, Rishika Babburu, Rachael Lowe, Aranka Van de Steene, Wendy Walker and Jess Bell
Definition/Description[edit | edit source]
Osteoporosis is defined as low bone mineral density caused by altered bone microstructure ultimately predisposing patients to low-impact, fragility fractures. In 2004, the WHO operationally defined osteoporosis based upon the bone mineral density (BMD) assessment of the patient. Thus the current osteoporosis definition is a “BMD that lies 2.5 standard deviations or more below the average value for young healthy women (a T-score of <-2.5 SD).”[1] The WHO definition applies to postmenopausal women and men aged 50 years or older. Although these definitions are necessary to establish the prevalence of osteoporosis, they should not be used as the sole determinant of treatment decisions. This diagnostic classification should not be applied to premenopausal women, men younger than 50 years, or children.[2] Osteoporosis, in which low bone mass and micro-structural deterioration of bone tissue lead to increased bone fragility, it is a chronic, progressive disease of multifactorial etiology.
In the last 15 years, there has been a movement to base the management of osteoporosis not on the absolute BMD values but to rather consider the risk for fracture risk in the future[3]. This was fuelled by the fact that most patients with a fragility fracture were not diagnosed with osteoporosis because their BMD did not meet the definition cut-off[3].
Osteoporotic fractures lead to a significant decrease in quality of life, with increased morbidity, mortality, and disability. Over 50% of postmenopausal white women will have an osteoporotic-related fracture. Only 33% of senior women who have a hip fracture will be able to return to independence. In white men, the risk of an osteoporotic fracture is 20%, but the one-year mortality in men who have a hip fracture is twice that of women. Black males and females have less osteoporosis than their white counterparts, but those diagnosed with osteoporosis have similar fracture risks. The aging of the American population is expected to triple the number of osteoporotic fractures.[4]
Associated definitions[edit | edit source]
Osteopenia is defined as a medical condition in which bone tissue's protein and mineral content is reduced, but less severely than in osteoporosis.
Sarcopenia is a multifactorial syndrome defined as a progressive and generalized loss of skeletal muscle mass and function, with an increased risk of disability, metabolic dysfunction, poor quality of life, and death. [5]
Etiology[edit | edit source]
Bone tissue is constantly being absorbed and replaced throughout one's life span. Bone mass decreases when the rate of absorption increases the rate of production; typically occurring with advanced age. Peak bone mass is met at an average age of 20. Those who develop less bone mass prior to this time, have a high chance of developing osteoporosis.[6]
Primary osteoporosis[edit | edit source]
Primary osteoporosis has no known definite cause, but there are many contributing factors associated with the disorder. These include prolonged negative calcium balance, impaired gonadal and adrenal function, oestrogen deficiency, or sedentary lifestyle.
Types of primary osteoporosis:[edit | edit source]
- Postmenopausal osteoporosis is associated with increased bone loss due to decreased production of oestrogen.[7] Women commonly lose 1% per year after peak bone density has been met, for up to 8 years after menopause.[8]
- Senile osteoporosis is an age-related bone loss that often accompanies advanced ageing.[7]
- Idiopathic juvenile osteoporosis
Secondary osteoporosis[edit | edit source]
Secondary osteoporosis is caused by prolonged use of medications or secondary to another disease or condition which inhibits the absorption of calcium or impedes the body's ability to produce bone.[7]
Low calcium intake or absorption can greatly increase one's risk of developing osteoporosis. Life-long calcium intake is crucial in building up bone stock prior to peak levels of bone mass, as well as to maintain bone mass after the age of 20. Excessive alcohol consumption can decrease the body's ability to absorb calcium.[9]
Bone responds to the load applied to it. Physically active individuals typically have higher bone density, than those who have a sedentary lifestyle.[9]
Hormone levels, either too little or too much, can impede the body's ability to produce and maintain adequate bone mass. Dysfunction with sex glands, thyroid, parathyroid, or adrenal glands is often associated with osteoporosis. [9]
Types of secondary osteoporosis[edit | edit source]
- Endocrine origin
- Hypogonadism/Hypogonadal state
- Hypercortisolism
- Hyperthyroidism
- Hyperparathyroidism
- Hyperprolactinemia
- Diabetes mellitus
- Gastrointestinal diseases
- Chronic inflammatory bowel disease
- Malabsorption/Deficiences
- Malnutrition
- Primary biliary cirrhosis
- Lactose intolerance
- Rheumatological and connective tissue diseases
- Inflammatory diseases
- Hematological and neoplastic disorders
- Medications - eg.Glucocorticoids, Chemotherapeutic/transplant drugs, Anticonvulsants
- Immobilisation
- Chronic alcoholism
- Organ Transplantation
- Genetic/congenital - eg. Marfan syndrome, Osteogenesis imperfecta, Glycogen storage disease, etc.
Risk Factors[edit | edit source]
Risk factors for osteoporosis include the following[12] :
- Advanced age (≥50 years)
- Female sex
- White or Asian ethnicity
- Genetic factors, such as a family history of osteoporosis
- Thin build or small stature (eg, bodyweight less than 127 lb [57.6 kg])
- Amenorrhea
- Late menarche
- Early menopause
- Postmenopausal state
- Physical inactivity or immobilization
- Use of certain drugs (eg, anticonvulsants, systemic steroids, thyroid supplements, heparin, chemotherapeutic agents, insulin)
- Alcohol and tobacco use
- Androgen or estrogen deficiency
- Calcium or vitamin D deficiency
- Dowager hump
Epidemiology[edit | edit source]
Over 200 million people have osteoporosis and the incidence rate increases with age.
- Over 70% of those over age 80 are affected
- It is more common in females than in males [13]
- In the developed world, 2% to 8% of males and 9% to 38% of females are affected
- Worldwide, there are approximately 9 million fractures per year as a result of osteoporosis
- 1 in 3 females and 1 in 5 males over the age of 50 will have an osteoporotic fracture
- Areas of the world with less Vitamin D through sunlight compared to regions closer to the equator have higher fracture rates in comparison to people living at lower latitudes[4]
- In the United States alone, approximately 10 million individuals are estimated to already have the disease and 34 million at increased risk for osteoporosis.[14] 55% of Americans over the age of 50 have the disorder[14]
Diagnosis[edit | edit source]
Patients with a diagnosis of osteoporosis should have:
- Laboratory assessment of their renal and thyroid function, a 25-hydroxyvitamin D and calcium level
- DEXA scan - the World Health Organization (WHO) established that dual x-ray absorptiometry tests scans (DEXA) of the central skeleton is the best test for assessing bone mineral density
- Scores between negative 1 and negative 2.5 reflect a diagnosis of osteopenia
- Scores below negative 2.5 reflect a diagnosis of osteoporosis
- The Fracture Risk Assessment Tool (FRAX) has become a more accurate way to measure 10years fracture probability. The FRAX questionnaire takes into account elements that influence an individual's bone quality as well as his/her bone density. [7] To learn more about FRAX view this tutorial
- The Garvan Fracture Risk Calculator with BMD
- Conventional radiography is used for the qualitative and semiquantitative evaluation
- Secondary tests for screening of secondary osteoporosis to determine causes of osteoporosis like 24-Hour urine calcium level, Parathyroid Hormone levels, Testosterone and gonadotropin levels in younger men with low bone densities, serum markers of osteoclasts/osteoblasts, etc.
Characteristics/Clinical Presentation[edit | edit source]
The physical exam rarely reveals any changes until osteoporosis is quite advanced. At that point, loss of height and kyphosis is evident from vertebral fractures.
In healthy individuals without risk factors, experts recommend:
- Start to screen women at the age of 65 years and men at the age of 70
- Patients with risk factors or a high score on an osteoporosis risk assessment test should be screened sooner[4]
Clinical Signs and Symptoms
- Back pain: Episodic, acute low thoracic/high lumbar pain
- Compression fracture of the spine
- Bone fractures
- Decrease in height
- Kyphosis
- Dowager’s hump
- Decreased activity tolerance
- Early satiety[15]
Associated Co-morbidities[edit | edit source]
As many diseases increase an individual's risk of osteoporosis, they also may be seen as comorbidities.[15]
- Eating disorders
- Cancer and cancer treatment
- Chronic renal failure
- Osteogenesis imperfect
- Rheumatic diseases
- Chronic pulmonary disease
- Cushing’s Disease
- Male hypogonadism
- Hypothyroidism
- Hyperparathyroidism
- Type 2 Diabetes Mellitus
- Gastrointestinal Disease
- Hepatic disease
Medicines for Osteoporosis[edit | edit source]
Osteoporosis medicines can increase bone density and while the increases may appear small this can have a very positive effect on reducing fracture rates. For example, medication can increase bone density in the hip by approx. 1-3% and in the spine by 4-8%, over the first 3-4years of treatment. Medication can reduce spinal fractures by around 30-70% and hip fractures by 30-50% (a positive effect can be seen as early as 6 – 12 months after starting treatment).
Osteoporosis medicines are grouped into different 'classes' depending on their 'active ingredient'
- Bisphosphonates - Tablets (daily, weekly or monthly): Alendronate (brand name Fosamax, or other generic brands), Risedronate (brand name Actonel, or other generic brands), once yearly intravenous infusion: Zoledronic acid (brand name Aclasta)
- Denosumab - 6 monthly injection: Denosumab (brand name: Prolia)
Denosumab works in a different way to bisphosphonates, but has the same effect of slowing the rate at which bone is broken down, with similar reductions in the risk of fracture. - Selective oestrogen receptor modulators (SERMS) - Daily tablet: Raloxifene (brand name: Evista)
- This medicine acts on bones in a similar way to that of the hormone oestrogen, slowing bone loss and reducing the risk of spinal fractures in women who have been through menopause
- Hormone replacement therapy (HRT) - The active ingredient is the hormone oestrogen. Some HRT treatments also contain progestogen (combined HRT)
- Even at low doses, HRT helps to slow bone loss, reducing the risk of osteoporosis and fractures in women who have gone through menopause. HRT is safe and effective for most women under the age of 60 who have osteoporosis and who also need hormonal treatment to relieve the symptoms of menopause. It may also be prescribed for women under 60 who are unable to take other osteoporosis medicines. It is particularly useful for women who have undergone early menopause (before 45 years of age)
- Due to the small increased risk of heart disease, strokes and breast cancer in older women, other osteoporosis medicines are more suitable for women over the age of 60
- Teriparatide - Daily injection for 18 months (self-administered): Teriparatide (Brand name: Forteo)
- This medicine stimulates bone-forming cells, resulting in improved bone strength and structure. It is only prescribed for people with severe osteoporosis when other osteoporosis medicines have not worked and the risk of more fractures is still very high. Teriparatide must be prescribed by a specialist and can only be taken for 18 months. Once the course of teriparatide is finished, another osteoporosis medicine must be started to ensure that the new bone formed is maintained and improved[16]
- Romosozumab - monthly injection: Romosozumab (brand name: Evenity)
Take note - Medical management isn't the only way to treat osteoporosis. It is also important to include daily exercise, good nutrition (including adequate amounts of calcium and vitamin D), smoking cessation, and limiting alcohol intake.[19]
Physical Therapy Management[edit | edit source]
Physical therapy intervention for individuals with osteoporosis, or even osteopenia, should include:
- Weight-bearing exercises
- Exercises such as walking or hopping, has been shown to maintain or improve bone density in this population
- Strengthening exercises, using weights or resistance bands, have also been shown to maintain or improve bone density at the location of the targeted muscle attachments
- Maintaining bone health in this population is extremely important, especially in the elderly as there is typically has a decline in bone mass with age[20]
- Flexibility and strengthening exercise
- These can help improve the individual's overall physical function and postural control. eg Tai chi, Yoga
- Improving postural control is important to reduce the risk of falls
- Falls often result in fractures in frail individuals
- Balance exercises are also important to incorporate to further reduce the risk of falls.[21] eg Otago Programme
- Postural exercise
- These are crucial to prevent structural changes that often accompany osteoporosis, such as thoracic kyphosis
- Every osteoporosis program should include extension exercises; chin tucks, scapular retractions, thoracic extensions, and hip extensions
- Strengthening the extensor muscles will promote improved posture and improved balance
- Flexion exercises are CONTRAINDICATED especially in patients with a risk of a spinal fracture. Anterior compressive forces to the vertebra can contribute to compression fractures[7]. Flexion and twisting place a high compressive load on the vertebral bodies, these high levels should be avoided [22].
- Balance exercise
- Education - top tips easily given to clients
- Follow a healthy diet that includes enough calcium and Vitamin D
- Wear sensible, well-fitting shoes to avoid falls
- Avoid rugs and sloppy slippers – both can cause trips
- Have good lighting on stairs
- Get eyesight checked regularly
- Try to avoid heavy lifting – consider home delivery grocery shopping
- Back pain
- Physiotherapists may treat patients with osteoporosis for back pain
- Agility training, resistance training, and stretching have all been shown to decrease back pain and its related disabilities in this population[23]
- High-intensity training - Research highly supports high-intensity training in the prevention of bone loss for women in menopausal years and the early post-menopausal period
- High-intensity training would include body-weight and resistive exercises at a high-intensity, similar to circuit training.[24] This type of training is often contraindicated for individuals with low bone mass
- Dynamic weight-bearing, high force exercise results with the greatest improvements at the femoral neck and moderate results at the femoral trochanter
- Dynamic weight-bearing, low force exercise had moderate positive effects on the spine
- Non-weight-bearing, high force exercises were shown to have moderate effects on the femoral neck[25]
Clinical Considerations[edit | edit source]
- Manipulations: A strong precaution should be taken before performing manual techniques such as manipulations or joint assessments that may increase an individual's risk for fractures, especially in the spine
- Body Weight Supported Treadmill Training: It is contraindicated to use body-weight supported treadmill training with individuals who have severe osteoporosis or lower extremity, pelvic, or rib fracture. Severe osteoporosis is considered a T-score greater than 2.5[28]
- Plyometrics and balance exercises should be performed with care and precaution to prevent falls and fractures.
Dietary Management[edit | edit source]
- The most important nutrients for people with osteoporosis are calcium and vitamin D. Calcium is a key building block for bones. Vitamin D helps the body to absorb calcium.
- Calcium can be from diet, supplements, or both (it is best to get these nutrients from food, rather than supplements)
- Optimal vitamin D can be acquired 3 ways:
- Eating foods that naturally contain vitamin D or are fortified with vitamin D
- Sensible sun exposure
- A few minutes, regularly, with good skin exposure, no sun cream and your shadow should be shorter than you. If it is longer than you are, you are not producing any vitamin D[31]
- Taking a vitamin D supplement
Team Work[edit | edit source]
Osteoporosis is a major public health problem affecting millions of elderly individuals. Besides causing fractures, the disorder leads to severe psychosocial and financial consequences for the patient. The condition has many risk factors and is best managed by an interprofessional team of healthcare workers.
- Patient education is vital as many are unaware of the serious consequences of the disorder. Early prevention can help reduce the high morbidity
- Attending physiotherapy for exercise prescription and participation in a supervised exercise programme is recommended
- Patients should be urged to modify their lifestyle and remain compliant with the medications prescribed
- The patient should be urged to quit smoking and abstain from alcohol
- The dietitian should educate the patient on a calcium-rich diet and the need to take vitamin D supplements
- The pharmacist should assist the team by educating the patient about the benefits of bisphosphonates and their adverse effects
- Women over the age of 65 should be urged to have a bone density scan[4]
Conclusion[edit | edit source]
- Osteoporosis is a common and silent disease until it is complicated by fractures
- It is estimated that 50% of women and 20% of men over the age of 50 years will develop an osteoporosis-related fracture at some stage
- These fractures are responsible for lasting disability, impaired quality of life, and increased mortality, with enormous medical and heavy personnel burden on both the patient’s and the nation’s economy
- Osteoporosis can be diagnosed and prevented with effective treatments before fractures occur
- The prevention, detection, and treatment of osteoporosis is important [32]
Case Reports/ Case Studies[edit | edit source]
Asymmetric lower-limb bone loss after spinal cord injury: Case report
Resources[edit | edit source]
National Osteoporosis Foundation
Journal of the American Physical Therapy Association Cochrane Review
References[edit | edit source]
- ↑ World Health Organization. WHO scientific group on the assessment of osteoporosis at primary health care level. Summary meeting report 2004 May 5 (Vol. 5, pp. 5-7).
- ↑ Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. 1994 Nov. 4(6):368-81.
- ↑ 3.0 3.1 Paskins Z, Ong T, Armstrong DJ. Bringing osteoporosis up to date: time to address the identity crisis. Age & Aging. 2020.
- ↑ 4.0 4.1 4.2 4.3 Joann L. Porter; Matthew Varacallo 19.12.2019 Osteoporosis Available from:https://www.ncbi.nlm.nih.gov/books/NBK441901/ (last accessed 27.2.2020)
- ↑ Cannataro R, Carbone L, Petro JL, Cione E, Vargas S, Angulo H, Forero DA, Odriozola-Martínez A, Kreider RB, Bonilla DA. Sarcopenia: Etiology, nutritional approaches, and miRNAs. International Journal of Molecular Sciences. 2021 Sep 8;22(18):9724.
- ↑ Mayo Clinic. Osteoporosis. http://www.mayoclinic.com/health/osteoporosis/DS00128 (accessed 28 March 2013)
- ↑ 7.0 7.1 7.2 7.3 7.4 Goodman. Fuller. Boissonnault. Pathology; Implications for the Physical Therapist. 2nd. Philadelphia: Saunders, 2003.
- ↑ Mayo Clinic. Osteoporosis Causes. http://www.mayoclinic.com/health/osteoporosis/DS00128/DSECTION=causes (accessed 28 March 2013)
- ↑ 9.0 9.1 9.2 Mayo Clinic. Osteoporosis: Risk Factors. http://www.mayoclinic.com/health/osteoporosis/DS00128/DSECTION=risk%2Dfactors (accessed 28 March 2013)
- ↑ Amgen. Osteoporosis 101: What is Osteoporosis and What You Need to Know. Available from: https://youtu.be/F1KJq6Pdp54 [last accessed 30/10/2020]
- ↑ Amgen. Postmenopausal Osteoporosis. Available from: https://youtu.be/c5tc01WFYks [last accessed 30/10/2020]
- ↑ Lyles KW, Schenck AP, Colón-Emeric CS. Hip and other osteoporotic fractures increase the risk of subsequent fractures in nursing home residents. Osteoporosis international. 2008 Aug;19(8):1225-33.
- ↑ Rosen CJ. The epidemiology and pathogenesis of osteoporosis. Endotext [Internet]. 2020 Jun 21.
- ↑ 14.0 14.1 National Osteoporosis Foundation Report Finds Patient-Centered Care Is Key Element in Delivering High-Quality, High-Value Treatment. 2019. Available from: https://www.nof.org/news/national-osteoporosis-foundation-report-finds-patient-centered-care-is-key-element-in-delivering-high-quality-high-value-treatment/ (accessed 14 October 2019)
- ↑ 15.0 15.1 Goodman. Snyder. Differential Diagnosis for Physical Therapists; Screening for Referral. 4th. St.Louis: Saunders, 2007.
- ↑ Osteoporosis Australia. Treatment options Available from:https://www.osteoporosis.org.au/treatment-options (last accessed 27.2.2020)
- ↑ Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CA, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A. Romosozumab Treatment in Postmenopausal Women with Osteoporosis. N Engl J Med. 2016 Oct 20;375(16):1532-1543.
- ↑ McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, Langdahl BL, Reginster JY, Zanchetta JR, Wasserman SM, Katz L, Maddox J, Yang YC, Libanati C, Bone HG. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014 Jan 30;370(5):412-20.
- ↑ Mayo Clinic. Osteoporosis treatment: Medication can help. http://www.mayoclinic.com/health/osteoporosis-treatment/WO00127 (Accessed 28 March 2013).
- ↑ Zehnacker CH, Bemis‐Dougherty A. Effect of Weighted Exercises on Bone Mineral Density in Post Menopausal Women A Systematic Review. Journal of Geriatric Physical Therapy. 2007; 30(2):79-88.
- ↑ Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clinical Rehabilitation; 26 (11): 1021-1031.
- ↑ Bonner Jr FJ, Sinaki M, Grabois M, Shipp KM, Lane JM, Lindsay R, Gold DT, Cosman F, Bouxsein ML, Weinstein JN, Gallagher RM. Health professional's guide to rehabilitation of the patient with osteoporosis. Osteoporosis International. 2003 May 1;14:S1.
- ↑ Liu-Ambrose TY, Khan KM, Eng JJ, Lord SR, Lentle B, McKay HA. Both resistance and agility training reduce back pain and improve health-related quality of life in older women with low bone mass. Osteoporos Int. 2005 Nov;16(11):1321-9.
- ↑ Martyn-St James M, Carroll S. High Intensity resistance training and postmenopausal bone loss: a meta-analysis. Osteoporosis International; 17: 1225-1240.
- ↑ Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. Exercise for preventing and treating osteoporosis in postmenopausal women. The Cochrane Collaboration. 2011;(2).
- ↑ Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane database of systematic reviews. 2011(11).
- ↑ Beck BR, Daly RM, Singh MA, Taaffe DR. Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of science and medicine in sport. 2017 May 1;20(5):438-45.
- ↑ U.S. Department of Health & Human Services. National Guideline Clearing House. Best evidence statement (BESt). Intensive partial body weight supported treadmill training. http://guideline.gov/content.aspx?id=24531&search=Gait+training+procedure+ (accessed 28 March 2013)
- ↑ 29.0 29.1 Muscogiuri G, Altieri B, Annweiler C, Balercia G, Pal HB, Boucher BJ, Cannell JJ, Foresta C, Grübler MR, Kotsa K, Mascitelli L. Vitamin D and chronic diseases: the current state of the art. Archives of toxicology. 2017 Jan;91(1):97-107.
- ↑ 30.0 30.1 Wacker M, Holick MF. Sunlight and Vitamin D: A global perspective for health. Dermato-endocrinology. 2013 Jan 1;5(1):51-108.
- ↑ Zielinska-Dabkowska KM. Vitamin D. The truth about Vitamin D and sun exposure demystified. Finding the balance for personal health.
- ↑ Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. European journal of rheumatology. 2017 Mar;4(1):46.