Hip Examination: Difference between revisions
No edit summary |
No edit summary |
||
| (23 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Laura Ritchie|Laura Ritchie]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Laura Ritchie|Laura Ritchie]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
| Line 10: | Line 9: | ||
=== Patient Intake === | === Patient Intake === | ||
The first step during the examination is the patient interview, during which the clinician gets a description of the presenting symptoms from the patient. Taking the history is a vital component of the subjective examination as it helps the clinician develop a hypothesis about the mechanism of injury, type of the injured structures and extent of the injury or damage. Details like the location of the pain, nature of the pain, 24-hour pattern of the pain, activities that trigger the pain, pain aggravating and relieving factors etc., are gotten from the patient during the interview. | The first step during the examination is the patient interview, during which the clinician gets a description of the presenting symptoms from the patient. Research suggests patient history plays a vital role in the differential diagnosis of hip pain and, in some cases, can be superior to objective tests and measures<ref name=":3">Wright AA, Ness BM, Donaldson M. [https://www.sciencedirect.com/science/article/abs/pii/S0003999321003208 Diagnostic accuracy of patient history in the diagnosis of hip-related pain: a systematic review.] Archives of Physical Medicine and Rehabilitation. 2021 Apr 28.</ref>. Taking the history is a vital component of the subjective examination as it helps the clinician develop a hypothesis about the mechanism of injury, type of the injured structures and extent of the injury or damage. Details like the location of the pain, nature of the pain, 24-hour pattern of the pain, activities that trigger the pain, pain aggravating and relieving factors etc., are gotten from the patient during the interview. According to new systematic review published in the Archives of Physical Medicine and Rehabilitation, thigh/groin pain and constant back/buttock pain are better indicators of hip OA than stand-alone tests and reported hip crepitus is a strong indicator of intra-articular hip pathology. <ref name=":3" /> | ||
The patient's past medical history, as well as their social/family history is also important as this helps the clinician rule out hereditary conditions. Any surgical histories that are specific to the hip region is also vital, for example, a patient who had a hip joint replacement surgery and is currently complaining of pain at the hip joint. The patient's drug history and current medications they are on should also be documented as well as any allergies they might have. The effects of the condition on the patient' functional status and Activities of Daily Living (ADLs) should be well assessed and documented. | The patient's past medical history, as well as their social/family history is also important as this helps the clinician rule out hereditary conditions. Any surgical histories that are specific to the hip region is also vital, for example, a patient who had a hip joint replacement surgery and is currently complaining of pain at the hip joint. The patient's drug history and current medications they are on should also be documented as well as any allergies they might have. The effects of the condition on the patient' functional status and Activities of Daily Living (ADLs) should be well assessed and documented. | ||
In the elderly it is also worth considering whether a fall was the result of a simple trip, or secondary to another reason, e.g. seizure, cardiovascular trigger, stroke or loss of consciousness. Relevant assessment of the cardiovascular or neurological system may be required with additional tests, e.g. ECG, CT brain.<ref name=":0" /> | In the elderly it is also worth considering whether a fall was the result of a simple trip, or secondary to another reason, e.g. seizure, cardiovascular trigger, stroke or loss of consciousness. Relevant assessment of the cardiovascular or neurological system may be required with additional tests, e.g. ECG, CT brain.<ref name=":0" /> | ||
=== Special | === Special Considerations === | ||
'''Red Flags'''<ref name=":2" /> | |||
* | * Sudden onset of pain. | ||
* A history of trauma | |||
* Any swelling | |||
* Any deformity | |||
* An inability to bear weight | |||
* Any lumps or bumps felt in the groin | |||
* Night pain | |||
* Any noticeable groin pulsations | |||
* Constipation or vomiting | |||
* Haematuria | |||
* Fever | |||
* Lower limb neurological symptoms - weakness, numbness or tingling | |||
* History of steroid use | |||
* Testicular swelling | |||
* Night sweats, unintentional weight loss, appetite loss | |||
* History of malignancy | |||
* High-risk sexual activity | |||
'''Other Flags''' | |||
It is also important to screen for [[The Flag System|other (yellow, orange, blue and black) flags]] as these may interfere with physiotherapy interventions. | |||
=== Investigations === | === Investigations === | ||
| Line 28: | Line 46: | ||
=== Observation === | === Observation === | ||
Upon conclusion of the patient interview, the clinician proceeds to the objective examination. A Pain [[Visual Analogue Scale|VAS]] is administered to determine the patient's baseline pain level and then the examiner observes and documents the following: | Upon conclusion of the patient interview, the clinician proceeds to the objective examination. A Pain [[Visual Analogue Scale|VAS]] is administered to determine the patient's baseline pain level and then the examiner observes and documents the following: | ||
*Bony deformity / Bony alignment<ref name=":1" /> | *Bony deformity / Bony alignment<ref name=":1">Nathan Humphries. Hip Objective Assessment. Heart of England Foundation Trust Emergency Department. Available from: <nowiki>http://www.heftemcast.co.uk/wp-content/uploads/2014/05/MSK-Objective-Assessments-Hip.pdf</nowiki> (accessed 30 August, 2018)</ref> | ||
##[[Gait|Gait pattern]]: There are several types of abnormal gait patterns associated with hip pathologies which the clinician needs to look out for such as Antalgic gait, [[Trendelenburg Gait|Trendelenburg gait]], Arthrogenic gait and Lurching gait. | ##[[Gait|Gait pattern]]: There are several types of abnormal gait patterns associated with hip pathologies which the clinician needs to look out for such as Antalgic gait, [[Trendelenburg Gait|Trendelenburg gait]], Arthrogenic gait and Lurching gait. | ||
##Weight Bearing | ##Weight Bearing | ||
| Line 38: | Line 56: | ||
*Swelling, scarring, skin changes (wounds) | *Swelling, scarring, skin changes (wounds) | ||
=== Palpation<ref name=":1" | === Palpation === | ||
During palpation, the examiner checks<ref name=":1" />: | |||
* Vascular System – Distal pulses, capillary refill | * Vascular System – Distal pulses, capillary refill | ||
* Sensation (Neurological Examination) – Peripheral nerve skin sensation and power | * Sensation (Neurological Examination) – Peripheral nerve skin sensation and power | ||
| Line 54: | Line 72: | ||
=== Neurologic Assessment === | === Neurologic Assessment === | ||
* [[Muscle Strength|Manual Muscle Testing]]: The strength of the muscle groups surrounding the hip joint, namely the hip extensors, flexors, abductors, adductors, internal and external rotators should be graded and documented. | * [[Muscle Strength Testing|Manual Muscle Testing]]: The strength of the muscle groups surrounding the hip joint, namely the hip extensors, flexors, abductors, adductors, internal and external rotators should be graded and documented. | ||
* [[Straight Leg Raise Test|Straight Leg Raise]] | * [[Straight Leg Raise Test|Straight Leg Raise]] | ||
* Dermatome Testing | * Dermatome Testing | ||
| Line 61: | Line 79: | ||
=== Movement Testing === | === Movement Testing === | ||
The available ranges of motion at the hip joint (Active and Passive) are measured using a goniometer and documented. These measurements serve as baseline readings and help determine if the intervention is yielding results. | The available ranges of motion at the hip joint (Active and Passive) are measured using a goniometer and documented. These measurements serve as baseline readings and help determine if the intervention is yielding results. | ||
{{#ev:youtube|sqY23nmTV40|300}} | |||
=== Special Tests === | === Special Tests === | ||
* [[Thomas Test|Thomas test]] | * [[Thomas Test|Thomas test]] | ||
* [[Trendelenburg | * [[Trendelenburg Sign|Trendelenberg sign]] | ||
* FABER test | * FABER test | ||
* FADDIR test | * FADDIR test | ||
* [[Ober's Test|Ober's test]] | * [[Ober's Test|Ober's test]] | ||
* Log roll | * Log roll test | ||
* Stinchfield test | * Stinchfield test | ||
* [[Ely's test]] | * [[Ely's test]] | ||
| Line 92: | Line 107: | ||
</div> | </div> | ||
== Differential Diagnosis == | |||
'''Orthopaedic/rheumatological causes'''<ref name=":2">Pipin Singh. Hip pain in adults - red flag symptoms. 2018. Available from: https://www.gponline.com/hip-pain-adults-red-flag-symptoms/musculoskeletal-disorders/article/1460668 (accessed 30 August 2018)</ref> | |||
* [[Osteoarthritis]] | |||
* [[Septic (Infectious) Arthritis|Septic arthritis]] | |||
* [[Osteomyelitis]] | |||
* Hip dislocation | |||
* [[Gout]] | |||
* Fractured neck of femur | |||
'''Pathological causes''' | |||
* [[Trochanteric Bursitis|Trochanteric bursitis]] | |||
* [[Iliotibial Band Syndrome|Iliotibial band syndrome]] | |||
* Meralgia paraesthetica | |||
* [[Avascular Necrosis Femoral Head|Avascular necrosis]] | |||
* [[Labral Tear|Labral tears]] | |||
* Referred from lumbar spine | |||
* Referred from sacroiliac joint | |||
'''Hernias, aneurysms and benign lumps''' | |||
* Inguinal lymphadenopathy secondary to multiple causes | |||
* [[Inguinal Hernia|Inguinal hernia]] | |||
* Femoral hernia | |||
* Femoral artery aneurysm | |||
* Lipoma | |||
* Sebaceous cyst | |||
'''Malignant causes''' | |||
* [[Osteosarcoma]] | |||
* Metastatic disease such as prostate cancer or pelvic tumours | |||
'''Miscellaneous''' | |||
* Renal calculus (loin to groin pain) | |||
* Iliopsoas abscess | |||
== Outcome Measures == | |||
* [[Harris Hip Score]] (HHS), | |||
* [[Hip Disability and Osteoarthritis Outcome Score]] (HOOS), | |||
* [[Oxford Hip Score]] (OHS), | |||
* Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH). | |||
* American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. | |||
* [[WOMAC Osteoarthritis Index|Western Ontario and McMaster Universities Osteoarthritis Index]] (WOMAC): | |||
== Resources == | |||
{{#ev:vimeo|93491651}} <div class="text-right"><ref name=":1">Nathan Humphries. Hip Objective Assessment. Heart of England Foundation Trust Emergency Department. Available from: <nowiki>http://www.heftemcast.co.uk/wp-content/uploads/2014/05/MSK-Objective-Assessments-Hip.pdf</nowiki> (accessed 30 August, 2018)</ref></div> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Hip]] | ||
[[Category:Assessment]] | |||
[[Category:Hip - Assessment and Examination]] | |||
[[Category:Athlete Assessment]] | |||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
Latest revision as of 15:00, 15 December 2022
Introduction[edit | edit source]
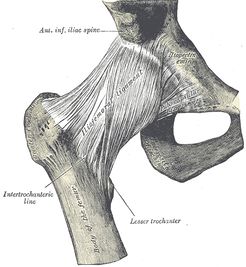
The Hip joint is one of the most important joints in the body because of the vital role it plays in locomotion. It is the second largest weight-bearing joint in the body, after the knee joint. It is a ball-and-socket synovial joint formed between the os coxa (hip bone) and the femur. The rounded head of the femur forms the ball, which fits into the acetabulum (socket in the pelvic bone) and ligaments connect the ball to the socket, thereby providing tremendous stability to the joint. Functionally, the hip joint enjoys a very high range of motion.
All of the various components of the hip mechanism assist in the mobility of the joint. Damage to any single component can negatively affect range of motion and ability to bear weight on the joint. In hip injury, as with other traumatic presentations, age distribution is bimodal with high-energy trauma in the younger population and potentially trivial mechanisms of injury in the older population, e.g. a simple fall.[1]
Subjective Examination[edit | edit source]
Patient Intake[edit | edit source]
The first step during the examination is the patient interview, during which the clinician gets a description of the presenting symptoms from the patient. Research suggests patient history plays a vital role in the differential diagnosis of hip pain and, in some cases, can be superior to objective tests and measures[2]. Taking the history is a vital component of the subjective examination as it helps the clinician develop a hypothesis about the mechanism of injury, type of the injured structures and extent of the injury or damage. Details like the location of the pain, nature of the pain, 24-hour pattern of the pain, activities that trigger the pain, pain aggravating and relieving factors etc., are gotten from the patient during the interview. According to new systematic review published in the Archives of Physical Medicine and Rehabilitation, thigh/groin pain and constant back/buttock pain are better indicators of hip OA than stand-alone tests and reported hip crepitus is a strong indicator of intra-articular hip pathology. [2]
The patient's past medical history, as well as their social/family history is also important as this helps the clinician rule out hereditary conditions. Any surgical histories that are specific to the hip region is also vital, for example, a patient who had a hip joint replacement surgery and is currently complaining of pain at the hip joint. The patient's drug history and current medications they are on should also be documented as well as any allergies they might have. The effects of the condition on the patient' functional status and Activities of Daily Living (ADLs) should be well assessed and documented.
In the elderly it is also worth considering whether a fall was the result of a simple trip, or secondary to another reason, e.g. seizure, cardiovascular trigger, stroke or loss of consciousness. Relevant assessment of the cardiovascular or neurological system may be required with additional tests, e.g. ECG, CT brain.[1]
Special Considerations[edit | edit source]
Red Flags[3]
- Sudden onset of pain.
- A history of trauma
- Any swelling
- Any deformity
- An inability to bear weight
- Any lumps or bumps felt in the groin
- Night pain
- Any noticeable groin pulsations
- Constipation or vomiting
- Haematuria
- Fever
- Lower limb neurological symptoms - weakness, numbness or tingling
- History of steroid use
- Testicular swelling
- Night sweats, unintentional weight loss, appetite loss
- History of malignancy
- High-risk sexual activity
Other Flags
It is also important to screen for other (yellow, orange, blue and black) flags as these may interfere with physiotherapy interventions.
Investigations[edit | edit source]
The first investigation of choice in a patient with hip pain following trauma is a hip x-ray. This will be an AP radiograph of the pelvis and a lateral radiograph of the painful hip. Fractures are not always identified on initial x-ray imaging. If there is a clinical concern for a hip fracture, but the x-ray is normal, further imaging is required. Both CT and MRI can be used to look for a radiographically occult fracture - MRI is more sensitive, but CT is usually easier to organise and in many institutions is the second-line investigation of choice.[1]
In complex fractures, CT can be helpful to get additional preoperative information that can be used to plan surgery and aid discussion about consent and prognosis. It is also worthwhile considering that interpretation of a hip x-ray will be complicated in the elderly by the present of other conditions, e.g. secondary osteoarthritis.[1]
Objective Examination[edit | edit source]
Observation[edit | edit source]
Upon conclusion of the patient interview, the clinician proceeds to the objective examination. A Pain VAS is administered to determine the patient's baseline pain level and then the examiner observes and documents the following:
- Bony deformity / Bony alignment[4]
- Gait pattern: There are several types of abnormal gait patterns associated with hip pathologies which the clinician needs to look out for such as Antalgic gait, Trendelenburg gait, Arthrogenic gait and Lurching gait.
- Weight Bearing
- Balance and Posture
- In Standing: Lumbar spine, Level of iliac crests (To rule out pelvic/SIJ dysfunction)
- Lying Supine: Leg length (apparent and real leg lengths), External rotation of leg.
- Colour changes e.g. bruising, inflammation, infection, rash.
- Muscle wasting, muscle spasm and muscle bulk
- Swelling, scarring, skin changes (wounds)
Palpation[edit | edit source]
During palpation, the examiner checks[4]:
- Vascular System – Distal pulses, capillary refill
- Sensation (Neurological Examination) – Peripheral nerve skin sensation and power
- Temperature – Infection / Inflammation
- Swelling – Effusion, Synovial thickening, Extra capsular
- Tenderness
- Lumbar spine
- Pelvis: Iliac crest, ASIS, Pubic rami, Symphysis pubis, PSIS, SIJ, Ischial tuberosity, Sacrum, Coccyx
- Greater trochanter
- Inguinal ligament
- Femoral triangle (hip joint)
- Knee
Neurologic Assessment[edit | edit source]
- Manual Muscle Testing: The strength of the muscle groups surrounding the hip joint, namely the hip extensors, flexors, abductors, adductors, internal and external rotators should be graded and documented.
- Straight Leg Raise
- Dermatome Testing
- Skin sensation test
Movement Testing[edit | edit source]
The available ranges of motion at the hip joint (Active and Passive) are measured using a goniometer and documented. These measurements serve as baseline readings and help determine if the intervention is yielding results.
Special Tests[edit | edit source]
- Thomas test
- Trendelenberg sign
- FABER test
- FADDIR test
- Ober's test
- Log roll test
- Stinchfield test
- Ely's test
Differential Diagnosis[edit | edit source]
Orthopaedic/rheumatological causes[3]
- Osteoarthritis
- Septic arthritis
- Osteomyelitis
- Hip dislocation
- Gout
- Fractured neck of femur
Pathological causes
- Trochanteric bursitis
- Iliotibial band syndrome
- Meralgia paraesthetica
- Avascular necrosis
- Labral tears
- Referred from lumbar spine
- Referred from sacroiliac joint
Hernias, aneurysms and benign lumps
- Inguinal lymphadenopathy secondary to multiple causes
- Inguinal hernia
- Femoral hernia
- Femoral artery aneurysm
- Lipoma
- Sebaceous cyst
Malignant causes
- Osteosarcoma
- Metastatic disease such as prostate cancer or pelvic tumours
Miscellaneous
- Renal calculus (loin to groin pain)
- Iliopsoas abscess
Outcome Measures[edit | edit source]
- Harris Hip Score (HHS),
- Hip Disability and Osteoarthritis Outcome Score (HOOS),
- Oxford Hip Score (OHS),
- Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH).
- American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire.
- Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC):
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Dr Jeremy Jones, Dr Derek Smith and Dr Craig Hacking. Investigation of hip injury (summary). 2018. Available from: https://radiopaedia.org/articles/investigation-of-hip-injury-summary (accessed 29 August 2018)
- ↑ 2.0 2.1 Wright AA, Ness BM, Donaldson M. Diagnostic accuracy of patient history in the diagnosis of hip-related pain: a systematic review. Archives of Physical Medicine and Rehabilitation. 2021 Apr 28.
- ↑ 3.0 3.1 Pipin Singh. Hip pain in adults - red flag symptoms. 2018. Available from: https://www.gponline.com/hip-pain-adults-red-flag-symptoms/musculoskeletal-disorders/article/1460668 (accessed 30 August 2018)
- ↑ 4.0 4.1 4.2 Nathan Humphries. Hip Objective Assessment. Heart of England Foundation Trust Emergency Department. Available from: http://www.heftemcast.co.uk/wp-content/uploads/2014/05/MSK-Objective-Assessments-Hip.pdf (accessed 30 August, 2018)
- ↑ BJSM Videos. Hip and Groin Exam (3 of 7): Patient history & palpation. Available from: http://www.youtube.com/watch?v=Y_EZvm0iSno [last accessed 25/01/14]
- ↑ BJSM Videos. FADDIR test. Available from: http://www.youtube.com/watch?v=3wK8JtHHAbg [last accessed 25/01/14]
- ↑ BJSM Videos. Flexion internal rotation test. Available from: http://www.youtube.com/watch?v=7RvaGasiWXM[last accessed 25/01/14]
- ↑ BJSM Videos. Thomas test. Available from: http://www.youtube.com/watch?v=lYbsVNtC1PM [last accessed 25/01/14]
- ↑ BJSM Videos. Trendelenburg's Sign. Available from: http://www.youtube.com/watch?v=Cewq53Wc7Jw[last accessed 25/01/14]
- ↑ BJSM Videos. Resisted Hip Abduction test. Available from: http://www.youtube.com/watch?v=goJXyusCCzA [last accessed 25/01/14]
- ↑ BJSM Videos. Resisted External Derotation Test. Available from: http://www.youtube.com/watch?v=Aq3Ripz4Jjw [last accessed 25/01/14]
- ↑ BJSM Videos. Single Adductor Test. Available from: http://www.youtube.com/watch?v=I21LmYARno0 [last accessed 25/01/14]
- ↑ BJSM Videos. Squeeze test. Available from: http://www.youtube.com/watch?v=--W5G9lP7pM [last accessed 25/01/14]
- ↑ BJSM Videos. Bilateral Adductor Test. Available from: http://www.youtube.com/watch?v=zOSoTz1IwWs [last accessed 25/01/14]