Gait in prosthetic rehabilitation: Difference between revisions
No edit summary |
No edit summary |
||
| (22 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Abbey Cain|Abby Cain]] as part of the [[ | '''Original Editor '''- [[User:Abbey Cain|Abby Cain]] as part of the [[World Physiotherapy Network for Amputee Rehabilitation Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
| Line 8: | Line 8: | ||
[[Gait|Gait]] is a term used to describe a walking pattern. ‘Normal gait’ is used to define a pattern which has been generalised from the general public across many variables, including age and sex<ref name="Fish">Fish DJ and Nielsen CP. [http://www.oandp.org/jpo/library/1993_02_039.asp Clinical Assessment of Human Gait]. Journal of prosthetics and Orthotics 1993. 2(39).</ref>. | [[Gait|Gait]] is a term used to describe a walking pattern. ‘Normal gait’ is used to define a pattern which has been generalised from the general public across many variables, including age and sex<ref name="Fish">Fish DJ and Nielsen CP. [http://www.oandp.org/jpo/library/1993_02_039.asp Clinical Assessment of Human Gait]. Journal of prosthetics and Orthotics 1993. 2(39).</ref>. | ||
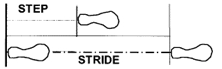
A complete [[Gait|cycle of gait]] begins at initial contact of one limb and ends at the repeated initial contact of the same limb, performing all phases of gait in doing so. This full cycle can be described as a stride. A step is sometimes incorrectly used to describe this cycle. A step however, is different; it is described as the distance of heel strike from one leg to the heel strike of the opposite leg<ref name="Perry">Perry J | A complete [[Gait|cycle of gait]] begins at initial contact of one limb and ends at the repeated initial contact of the same limb, performing all phases of gait in doing so. This full cycle can be described as a stride. A step is sometimes incorrectly used to describe this cycle. A step however, is different; it is described as the distance of heel strike from one leg to the heel strike of the opposite leg<ref name="Perry">Perry J and Burnfield J.M Gait Analysis, Normal and Pathological Function. 2nd Ed. USA, SLACK Incorporated USA 2010</ref>. | ||
[[Image:Step and stride.png|thumb|center|400px|Step and stride in human gait]]<br> | [[Image:Step and stride.png|thumb|center|400px|Step and stride in human gait]]<br> | ||
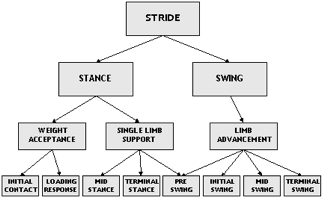
The gait cycle can be split into 2 stages; | The gait cycle can be split into 2 stages.<ref>Masood H, Farooq H. [https://www.mdpi.com/2079-9292/11/15/2386 Utilizing spatio temporal gait pattern and quadratic SVM for gait recognition]. Electronics. 2022; 11(15):2386. </ref> | ||
#'''Stance Phase''' -Time the foot is in contact with the floor, weight acceptance and single leg stance, which makes up 60% of the cycle<ref name="Fish" /> | #'''Stance Phase''' -Time the foot is in contact with the floor, weight acceptance and single leg stance (i.e. the "heel-to-toe contact sequence of the foot"<ref name=":0">Cicirelli G, Impedovo D, Dentamaro V, Marani R, Pirlo G, D'Orazio TR. [https://ieeexplore.ieee.org/abstract/document/9466394 Human gait analysis in neurodegenerative diseases: a review]. IEEE J Biomed Health Inform. 2022 Jan;26(1):229-42. </ref>), which makes up 60% of the cycle<ref name="Fish" /> | ||
#'''Swing Phase''' – The period of time where the limb is lifted from the floor, limb advancement. This makes up 40% of the cycle<ref name="Fish" /> | #'''Swing Phase''' – The period of time where the limb is lifted from the floor, limb advancement (i.e. when the foot is suspended<ref name=":0" />). This makes up 40% of the cycle<ref name="Fish" /> | ||
In order to describe the elements of gait, the cycle can be broken down further into 8 sub factors<ref name="Fish" /><ref name="Perry" />: | In order to describe the elements of gait, the cycle can be broken down further into 8 sub factors<ref name="Fish" /><ref name="Perry" /><ref>Yan S-H, Liu Y-C, Li W, Zhang K. [https://www.sciencedirect.com/science/article/pii/S2590093521000369 Gait phase detection by using a portable system and artificial neural network]. Medicine in Novel Technology and Devices. 2021;12:100092.</ref>: | ||
*Initial | *Initial Contact | ||
*Loading | *Loading Response | ||
*Midstance | *Midstance | ||
*Terminal | *Terminal Stance | ||
*Preswing | *Preswing | ||
*Initial | *Initial Swing | ||
*Midswing | *Midswing | ||
*Terminal | *Terminal Swing | ||
The diagram demonstrates this division of gait cycle. | The diagram demonstrates this division of the gait cycle. | ||
[[Image:Divisions of gait cycle.png|thumb|center|400px|Divisions of Gait Cycle]] | [[Image:Divisions of gait cycle.png|thumb|center|400px|Divisions of Gait Cycle]] | ||
=== Initial | === Initial Contact === | ||
Also known as heel strike. This is the first moment the foot comes into contact with the floor. The hip is flexed approximately to 30 degrees , knee extended between 0-5 degrees and ankle dorsiflexed to a neutral position, giving contact with the floor at approximately a 25 degree angle. This is the first phase of double limb support. The aim of initial contact is to stabilise the limb in preparation for it to take the impending forward translation of body weight<ref name="Perry" /><ref name="Physiopedia">Physiopedia. Gait Cycle http://www.physio-pedia.com/Gait_Cycle (accessed 5 February 2015)</ref>. | Also known as heel strike. This is the first moment the foot comes into contact with the floor. The hip is flexed approximately to 30 degrees, knee extended between 0-5 degrees and ankle dorsiflexed to a neutral position, giving contact with the floor at approximately a 25-degree angle. This is the first phase of double limb support. The aim of initial contact is to stabilise the limb in preparation for it to take the impending forward translation of body weight<ref name="Perry" /><ref name="Physiopedia">Physiopedia. Gait Cycle http://www.physio-pedia.com/Gait_Cycle (accessed 5 February 2015)</ref>. | ||
=== Loading | === Loading Response === | ||
The foot flattens on the floor through pronation. The hip begins to extend and propels the body forwards and over the foot, using the heel as a ‘rocker’. The knee then flexes to allow shock absorption. The aim of this phase is shock absorption, weight bearing stability and preservation of progression<ref name="Perry" /><ref name="Physiopedia" />. | The foot flattens on the floor through pronation. The hip begins to extend and propels the body forwards and over the foot, using the heel as a ‘rocker’. The knee then flexes to allow shock absorption. The aim of this phase is shock absorption, weight bearing stability and preservation of progression<ref name="Perry" /><ref name="Physiopedia" />. | ||
=== Mid | === Mid Stance === | ||
This is the first half of single limb support. Weight is aligned fully over the supporting foot through ankle dorsiflexion, while the hip and knee extend, as the other foot lifts | This is the first half of single limb support. Weight is aligned fully over the supporting foot through ankle dorsiflexion, while the hip and knee extend, as the other foot lifts off the floor. The body weight is fully supported on one leg<ref name="Perry" /><ref name="Physiopedia" />. | ||
=== Terminal | === Terminal Stance === | ||
This is the second half of single leg support; it begins as the other leg lifts | This is the second half of single leg support; it begins as the other leg lifts off the floor. The heel of the loaded limb lifts off the floor and the body weight moves forward past the forefoot, as the hip increases in extension. The knee gains full extension and begins to flex again. This phase is completed when the non-loaded limb makes contact with the floor<ref name="Perry" /><ref name="Physiopedia" />. | ||
=== Pre-swing === | === Pre-swing === | ||
| Line 52: | Line 52: | ||
Also known as ‘toe off’ and is the final phase of stance. The other limb has now begun a new stance phase and is in the initial contact phase. The limb is rapidly off loaded with a forward push to transfer the weight onto the opposite limb. The knee is flexed and the ankle plantarflexes as the toe leaves the ground<ref name="Perry" /><ref name="Physiopedia" />. | Also known as ‘toe off’ and is the final phase of stance. The other limb has now begun a new stance phase and is in the initial contact phase. The limb is rapidly off loaded with a forward push to transfer the weight onto the opposite limb. The knee is flexed and the ankle plantarflexes as the toe leaves the ground<ref name="Perry" /><ref name="Physiopedia" />. | ||
=== Initial | === Initial Swing === | ||
The foot is lifted off the floor by hip and knee flexion, as the ankle begins to dorsiflex. The other foot will be in midstance phase. When the | The foot is lifted off the floor by hip and knee flexion, as the ankle begins to dorsiflex. The other foot will be in midstance phase. When the offloading limb is level with the leg in stance phase the initial swing phase is complete<ref name="Perry" /><ref name="Physiopedia" />. | ||
=== Mid | === Mid Swing === | ||
The limb swings forward of the body through hip flexion as the knee begins to extend. The foot is clear of the floor<ref name="Perry" /> | The limb swings forward of the body through hip flexion as the knee begins to extend. The foot is clear of the floor<ref name="Perry" /> | ||
=== Terminal | === Terminal Swing === | ||
Also known as late swing, the knee becomes fully extended and the ankle dorsiflexes to neutral as the foot prepares to make contact with the floor<ref name="Perry" />. | Also known as late swing, the knee becomes fully extended and the ankle dorsiflexes to neutral as the foot prepares to make contact with the floor<ref name="Perry" />. | ||
| Line 68: | Line 68: | ||
[[Image:Gait-Cycle.jpg|center|800px]] | [[Image:Gait-Cycle.jpg|center|800px]] | ||
{{#ev:youtube| | <br> | ||
{{#ev:youtube|96nLX6sm9Yw|300}}<ref>Global HELP Organization. Understanding & Analyzing Gait For The Clinician: Part 05 [The Gait Cycle] May 2018. Available from: https://youtu.be/96nLX6sm9Yw. </ref> | |||
== Prosthetic Gait == | == Prosthetic Gait == | ||
After an amputation the amputee uses different muscle groups in order to create a smoother gait pattern. Overall energy consumption required is higher, due to the increased effort required to compensate for the | After an amputation, the amputee uses different muscle groups in order to create a smoother gait pattern. Overall energy consumption required is higher, due to the increased effort required to compensate for the loss of the limb. While progress has been made in the design of prostheses, "the replacement of lower-limb segments with a prosthesis affects the efficiency of this locomotion."<ref>Di Gregorio R, Vocenas L. [https://www.mdpi.com/2313-7673/6/2/22/htm Identification of gait-cycle phases for prosthesis control]. Biomimetics (Basel). 2021 Mar 26;6(2):22. </ref> The amount of metabolic oxygen consumption in a non-amputee correlates directly to increased walking distance and speeds. In the amputees, however, this metabolic cost is higher even at normal speed. On average these increased requirements are<ref name="Kishner">Kishner's Gait Analysis after Amputation updated July 2013 http://emedicine.medscape.com/article/1237638-overview (accessed 3 February 2015)</ref>: | ||
*Traumatic Transtibial | *Traumatic Transtibial Gait - 25% increased energy requirement | ||
*Vascular Transtibial | *Vascular Transtibial Gait - 40 % increased energy requirement | ||
*Traumatic Transfemoral | *Traumatic Transfemoral Gait - 68% increased energy requirement | ||
*Vascular | *Vascular Transfemoral Gait -100% increased energy requirement<br> | ||
=== Transtibial Gait === | === Transtibial Gait === | ||
The average gait pattern will vary dependent on the type of prosthesis used for mobility, however generalisations can be made | The average gait pattern will vary dependent on the type of prosthesis used for mobility, however, generalisations can be made. | ||
The | '''The ankle''' of the prosthesis has a reduced range of movement compared to the anatomical ankle. This results in prolonged heel strike and weight bearing through the heel before flat foot contact, with delayed forefoot loading<ref name="Smith">Smith D,, Michael J, W and Bowker J,H American Academy of Orthopaedic Surgeons. Atlas of Amputations and Limb deficiencies. Surgical, prosthetic and rehabilitation Principles. 3rd Ed. USA. 2011</ref> | ||
During swing phase of the prosthetic limb the | '''Knee flexion''' is decreased at initial contact and the overall maximum flexion achieved is reduced as the foot moves to floor contact to<ref name="Smith" />.'''During swing phase''' of the non-prosthetic limb the body weight begins to move forward over the prosthetic limb, which is in stance phase. In order to gain adequate step length of the non-prosthetic limb, heel rise on the prosthesis occurs earlier. The heel rise achieved is greater than that of a normal gait pattern<ref name="Smith" />. This creates an elevation of the body and results in a greater loading force on the non-prosthetic side (or sound side) (approx 130% compared to average 111%) as the body weight drops more rapidly onto the limb. Greater quadriceps contraction is needed to absorb the force<ref name="Kishner" /><ref name="Smith" />. The ‘toe off’ force generated from the prosthetic limb is reduced, which is compensated for by the hip flexors. Flexion of the knee on the prosthetic limb occurs with some hamstring contraction but mainly eccentric contraction of the quadriceps<ref name="AUSTPAR">Australian Physiotherapists in Amputee Rehabilitation http://austpar.com (accessed 7 February 2015)</ref> | ||
= | '''During the stance phase,''' the energy generated by the prosthetic limb is reduced by 50% to that which would be generated by the normal limb, this is compensated by greater energy expenditure in muscles higher up the limb. The rocker effect of the prosthesis results in increased instability and the reduced knee flexion achieved on the prosthetic side requires hip muscles to generate greater energy to ensure stability. As the body transfers weight in a forward motion this energy generation is then transmitted to the trunk muscles in order to generate enough force to propel the body forward and to compensate for the loss of energy through the prosthesis<ref name="Kishner" />. | ||
Due to the reduced ankle movement of the prosthesis the range of extension at the hip is reduced to approx half of that of the opposite limb. The stance time on the non-prosthetic side is also increased compared to the prosthetic side<ref name="Smith" />.<br> | |||
=== Transfemoral Gait === | |||
== | A person with a transfemoral amputation has to compensate for the loss of both the knee and ankle joint<ref name="Kishner" />. '''The gait cycle is affected by''' the quality of the surgery, the type and alignment of the prosthesis, the condition of the stump and the length of the remaining muscular structure and how well these are reattached<ref name="AUSTPAR" />. | ||
The '''main focus''' of the gait cycle is to prevent the knee from buckling during stance phase. A ‘fixed knee’ prosthesis will counteract this issue. | |||
'''A ‘free knee’''' will need to remain in extension for longer throughout the stance phase approx 30-40% to ensure buckling does not occur<ref name="Kishner" />. This extension causes prolonged heel strike and the body will move forward over the prosthetic leg as one unit for stance phase. The hip extensors on the prosthetic side will work to stabilise the limb in prosthetic weight bearing<ref name="Kishner" />. | |||
'''During the swing phase''' of the prosthetic limb, the hip extensors and calf muscles on the sound side help to generate force for the sound limb to swing forwards. Hip flexors on the prosthetic limb must generate the same force required during normal gait. Although the prosthesis is generally 30% lighter than the limb would be, speed generated by the hip flexors is required in order to snap the prosthesis of a ‘free knee’ into extension for heel strike<ref name="Kishner" /><ref name="Smith" />. | |||
= | General control and strength are reduced in a transfemoral amputation due to the shortened lever length of the thigh muscles, which reduces the force of contraction<ref name="Kishner" />. | ||
For amputees with a '''fixed knee''' (locked knee) prosthesis floor clearance is reduced during swing phase, due to the lack of knee flexion and ankle dorsi flexion. Elevation of the hip using trunk and hip muscles is required to prevent dragging on the floor known as ‘hip hitching’ or ‘hip hiking’<ref name="Smith" />. | |||
'''Stance time''' on the sound limb is increased as it is for transtibial amputees, because of the instability resulting from the prosthesis and the reduced range of motion available. Overall energy expenditure is higher than is required for a transtibial amputee due to the energy which is lost through the prosthesis over two joints and not one. Greater compensation is required by the hip and trunk muscles and the contralateral limb to generate the energy required for stability and movement throughout the gait cycle<ref name="Kishner" />.<br> | |||
< | A person with a transfemoral amputation will '''walk 30% slower''' than someone without an amputation. The sound limb will have higher ground reaction force and more hip range with single limb stance than the prosthetic side. The sound ankle, knee and hip also have bigger joint moments. This all leads to asymmetry that can lead to low back pain and sound limb osteoarthritis. <ref name="Harandi">Harandi VJ, Ackland DC, Haddara R, Lizama LE, Graf M, Galea MP, Lee PV. Gait compensatory mechanisms in unilateral transfemoral amputees. Medical Engineering & Physics. 2020 Jan 7.</ref> | ||
= | Harandi et al. <ref name="Harandi">Harandi VJ, Ackland DC, Haddara R, Lizama LE, Graf M, Galea MP, Lee PV. Gait compensatory mechanisms in unilateral transfemoral amputees. Medical Engineering & Physics. 2020 Jan 7.</ref> found the following with regards to people with transfemoral amputations: | ||
*Compensatory strategies are used during walking | |||
*The sound limb muscles are essential in mediolateral balance | |||
*The prosthesis is providing support, progression and breaking during the stance phase of gait | |||
*When there is an increased pelvic tilt to the prosthetic side the person will also have a reduction in hip motion.<ref name="Harandi">Harandi VJ, Ackland DC, Haddara R, Lizama LE, Graf M, Galea MP, Lee PV. Gait compensatory mechanisms in unilateral transfemoral amputees. Medical Engineering & Physics. 2020 Jan 7.</ref> | |||
==Gait Deviations== | |||
While assessing amputee gait it is important to be aware of normal gait and how normal gait in the amputee is affected. Furthermore, there may be deviations which an amputee will adopt to compensate for the prosthesis, muscle weakness or tightening, lack of balance and fear. These deviations create an altered gait pattern and it is important that these are recognised, as rehabilitation of the gait will need to encompass corrections of these deviations<ref name="AUSTPAR" /><ref name="Smith" />. | |||
< | {{#ev:youtube|Syv3vfwm2Js|300}}<ref>American Academy of Orthotists and Prosthetists. Prosthetic Observational Gait Scale (POGS). Dec 2017. Available from: https://youtu.be/Syv3vfwm2Js</ref> | ||
Learn about common gait deviations on the [[Gait_deviations_in_amputees|Gait deviations in amputees]] page. | |||
== Summary == | == Summary == | ||
Amputees should have a | Amputees should have a fully functional and physical assessment and rehabilitation should be based around personalised functional goals. Individualised exercise programmes are developed after a thorough assessment. Awareness of normal gait and the deviations and their cause formulates the basis of the correct rehabilitation of the individual<ref name="Gailey">Gailey R,S and Curtis R,C. Physical Therapy Management of Adult Lower-Limb Amputees. Atlas of Limb Prosthetics; Surgical Prosthetic and Rehabilitation Principles. Chapter 23. Abridged version. O and P Virtual Library</ref><ref name="BACPAR">British association of Chartered Physiotherapists in Amputee Rehabilitation. Evidenced Based Clinical Guidelines for the Physiotherapy Management of Adults with Lower limb Prosthesis. CSP Clinical Guideline 03. November 2012</ref>. There are numerous techniques that can be used during rehabilitation and not all of them will be appropriate for each individual, therefore the programme and technique must be applied to each individual and reviewed regularly to ensure it remains adequate<ref name="Smith" /><ref name="Gailey" />. The amputee’s previous level of activity, overall health and potential to improve needs to be taken into consideration when formulating a rehabilitation programme and should aim at translating the function gained in a controlled environment into their own home functional environment<ref name="Gailey" /><ref name="BACPAR" />.<br> | ||
== References == | == References == | ||
| Line 325: | Line 133: | ||
<references /> | <references /> | ||
[[Category:Amputees]] [[Category: | [[Category:Amputees]] | ||
[[Category:World Physiotherapy Amputee Project]] | |||
[[Category: Course Pages]] | |||
[[Category:Prosthetics and Orthotics]] | |||
Latest revision as of 07:36, 20 November 2022
Original Editor - Abby Cain as part of the World Physiotherapy Network for Amputee Rehabilitation Project
Top Contributors - Admin, Rachael Lowe, Kim Jackson, Tarina van der Stockt, Naomi O'Reilly, Jess Bell and Simisola Ajeyalemi
Normal Gait [edit | edit source]
Gait is a term used to describe a walking pattern. ‘Normal gait’ is used to define a pattern which has been generalised from the general public across many variables, including age and sex[1].
A complete cycle of gait begins at initial contact of one limb and ends at the repeated initial contact of the same limb, performing all phases of gait in doing so. This full cycle can be described as a stride. A step is sometimes incorrectly used to describe this cycle. A step however, is different; it is described as the distance of heel strike from one leg to the heel strike of the opposite leg[2].
The gait cycle can be split into 2 stages.[3]
- Stance Phase -Time the foot is in contact with the floor, weight acceptance and single leg stance (i.e. the "heel-to-toe contact sequence of the foot"[4]), which makes up 60% of the cycle[1]
- Swing Phase – The period of time where the limb is lifted from the floor, limb advancement (i.e. when the foot is suspended[4]). This makes up 40% of the cycle[1]
In order to describe the elements of gait, the cycle can be broken down further into 8 sub factors[1][2][5]:
- Initial Contact
- Loading Response
- Midstance
- Terminal Stance
- Preswing
- Initial Swing
- Midswing
- Terminal Swing
The diagram demonstrates this division of the gait cycle.
Initial Contact[edit | edit source]
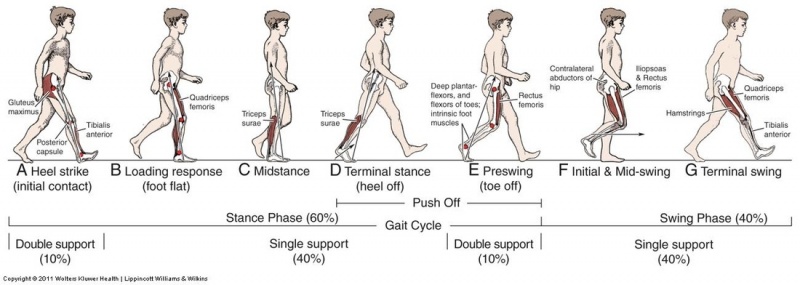
Also known as heel strike. This is the first moment the foot comes into contact with the floor. The hip is flexed approximately to 30 degrees, knee extended between 0-5 degrees and ankle dorsiflexed to a neutral position, giving contact with the floor at approximately a 25-degree angle. This is the first phase of double limb support. The aim of initial contact is to stabilise the limb in preparation for it to take the impending forward translation of body weight[2][6].
Loading Response[edit | edit source]
The foot flattens on the floor through pronation. The hip begins to extend and propels the body forwards and over the foot, using the heel as a ‘rocker’. The knee then flexes to allow shock absorption. The aim of this phase is shock absorption, weight bearing stability and preservation of progression[2][6].
Mid Stance[edit | edit source]
This is the first half of single limb support. Weight is aligned fully over the supporting foot through ankle dorsiflexion, while the hip and knee extend, as the other foot lifts off the floor. The body weight is fully supported on one leg[2][6].
Terminal Stance[edit | edit source]
This is the second half of single leg support; it begins as the other leg lifts off the floor. The heel of the loaded limb lifts off the floor and the body weight moves forward past the forefoot, as the hip increases in extension. The knee gains full extension and begins to flex again. This phase is completed when the non-loaded limb makes contact with the floor[2][6].
Pre-swing[edit | edit source]
Also known as ‘toe off’ and is the final phase of stance. The other limb has now begun a new stance phase and is in the initial contact phase. The limb is rapidly off loaded with a forward push to transfer the weight onto the opposite limb. The knee is flexed and the ankle plantarflexes as the toe leaves the ground[2][6].
Initial Swing[edit | edit source]
The foot is lifted off the floor by hip and knee flexion, as the ankle begins to dorsiflex. The other foot will be in midstance phase. When the offloading limb is level with the leg in stance phase the initial swing phase is complete[2][6].
Mid Swing[edit | edit source]
The limb swings forward of the body through hip flexion as the knee begins to extend. The foot is clear of the floor[2]
Terminal Swing[edit | edit source]
Also known as late swing, the knee becomes fully extended and the ankle dorsiflexes to neutral as the foot prepares to make contact with the floor[2].
The diagram below demonstrates the 8 phases of the gait cycle:
Prosthetic Gait[edit | edit source]
After an amputation, the amputee uses different muscle groups in order to create a smoother gait pattern. Overall energy consumption required is higher, due to the increased effort required to compensate for the loss of the limb. While progress has been made in the design of prostheses, "the replacement of lower-limb segments with a prosthesis affects the efficiency of this locomotion."[8] The amount of metabolic oxygen consumption in a non-amputee correlates directly to increased walking distance and speeds. In the amputees, however, this metabolic cost is higher even at normal speed. On average these increased requirements are[9]:
- Traumatic Transtibial Gait - 25% increased energy requirement
- Vascular Transtibial Gait - 40 % increased energy requirement
- Traumatic Transfemoral Gait - 68% increased energy requirement
- Vascular Transfemoral Gait -100% increased energy requirement
Transtibial Gait[edit | edit source]
The average gait pattern will vary dependent on the type of prosthesis used for mobility, however, generalisations can be made.
The ankle of the prosthesis has a reduced range of movement compared to the anatomical ankle. This results in prolonged heel strike and weight bearing through the heel before flat foot contact, with delayed forefoot loading[10]
Knee flexion is decreased at initial contact and the overall maximum flexion achieved is reduced as the foot moves to floor contact to[10].During swing phase of the non-prosthetic limb the body weight begins to move forward over the prosthetic limb, which is in stance phase. In order to gain adequate step length of the non-prosthetic limb, heel rise on the prosthesis occurs earlier. The heel rise achieved is greater than that of a normal gait pattern[10]. This creates an elevation of the body and results in a greater loading force on the non-prosthetic side (or sound side) (approx 130% compared to average 111%) as the body weight drops more rapidly onto the limb. Greater quadriceps contraction is needed to absorb the force[9][10]. The ‘toe off’ force generated from the prosthetic limb is reduced, which is compensated for by the hip flexors. Flexion of the knee on the prosthetic limb occurs with some hamstring contraction but mainly eccentric contraction of the quadriceps[11]
During the stance phase, the energy generated by the prosthetic limb is reduced by 50% to that which would be generated by the normal limb, this is compensated by greater energy expenditure in muscles higher up the limb. The rocker effect of the prosthesis results in increased instability and the reduced knee flexion achieved on the prosthetic side requires hip muscles to generate greater energy to ensure stability. As the body transfers weight in a forward motion this energy generation is then transmitted to the trunk muscles in order to generate enough force to propel the body forward and to compensate for the loss of energy through the prosthesis[9].
Due to the reduced ankle movement of the prosthesis the range of extension at the hip is reduced to approx half of that of the opposite limb. The stance time on the non-prosthetic side is also increased compared to the prosthetic side[10].
Transfemoral Gait[edit | edit source]
A person with a transfemoral amputation has to compensate for the loss of both the knee and ankle joint[9]. The gait cycle is affected by the quality of the surgery, the type and alignment of the prosthesis, the condition of the stump and the length of the remaining muscular structure and how well these are reattached[11].
The main focus of the gait cycle is to prevent the knee from buckling during stance phase. A ‘fixed knee’ prosthesis will counteract this issue.
A ‘free knee’ will need to remain in extension for longer throughout the stance phase approx 30-40% to ensure buckling does not occur[9]. This extension causes prolonged heel strike and the body will move forward over the prosthetic leg as one unit for stance phase. The hip extensors on the prosthetic side will work to stabilise the limb in prosthetic weight bearing[9].
During the swing phase of the prosthetic limb, the hip extensors and calf muscles on the sound side help to generate force for the sound limb to swing forwards. Hip flexors on the prosthetic limb must generate the same force required during normal gait. Although the prosthesis is generally 30% lighter than the limb would be, speed generated by the hip flexors is required in order to snap the prosthesis of a ‘free knee’ into extension for heel strike[9][10].
General control and strength are reduced in a transfemoral amputation due to the shortened lever length of the thigh muscles, which reduces the force of contraction[9].
For amputees with a fixed knee (locked knee) prosthesis floor clearance is reduced during swing phase, due to the lack of knee flexion and ankle dorsi flexion. Elevation of the hip using trunk and hip muscles is required to prevent dragging on the floor known as ‘hip hitching’ or ‘hip hiking’[10].
Stance time on the sound limb is increased as it is for transtibial amputees, because of the instability resulting from the prosthesis and the reduced range of motion available. Overall energy expenditure is higher than is required for a transtibial amputee due to the energy which is lost through the prosthesis over two joints and not one. Greater compensation is required by the hip and trunk muscles and the contralateral limb to generate the energy required for stability and movement throughout the gait cycle[9].
A person with a transfemoral amputation will walk 30% slower than someone without an amputation. The sound limb will have higher ground reaction force and more hip range with single limb stance than the prosthetic side. The sound ankle, knee and hip also have bigger joint moments. This all leads to asymmetry that can lead to low back pain and sound limb osteoarthritis. [12]
Harandi et al. [12] found the following with regards to people with transfemoral amputations:
- Compensatory strategies are used during walking
- The sound limb muscles are essential in mediolateral balance
- The prosthesis is providing support, progression and breaking during the stance phase of gait
- When there is an increased pelvic tilt to the prosthetic side the person will also have a reduction in hip motion.[12]
Gait Deviations[edit | edit source]
While assessing amputee gait it is important to be aware of normal gait and how normal gait in the amputee is affected. Furthermore, there may be deviations which an amputee will adopt to compensate for the prosthesis, muscle weakness or tightening, lack of balance and fear. These deviations create an altered gait pattern and it is important that these are recognised, as rehabilitation of the gait will need to encompass corrections of these deviations[11][10].
Learn about common gait deviations on the Gait deviations in amputees page.
Summary[edit | edit source]
Amputees should have a fully functional and physical assessment and rehabilitation should be based around personalised functional goals. Individualised exercise programmes are developed after a thorough assessment. Awareness of normal gait and the deviations and their cause formulates the basis of the correct rehabilitation of the individual[14][15]. There are numerous techniques that can be used during rehabilitation and not all of them will be appropriate for each individual, therefore the programme and technique must be applied to each individual and reviewed regularly to ensure it remains adequate[10][14]. The amputee’s previous level of activity, overall health and potential to improve needs to be taken into consideration when formulating a rehabilitation programme and should aim at translating the function gained in a controlled environment into their own home functional environment[14][15].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Fish DJ and Nielsen CP. Clinical Assessment of Human Gait. Journal of prosthetics and Orthotics 1993. 2(39).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Perry J and Burnfield J.M Gait Analysis, Normal and Pathological Function. 2nd Ed. USA, SLACK Incorporated USA 2010
- ↑ Masood H, Farooq H. Utilizing spatio temporal gait pattern and quadratic SVM for gait recognition. Electronics. 2022; 11(15):2386.
- ↑ 4.0 4.1 Cicirelli G, Impedovo D, Dentamaro V, Marani R, Pirlo G, D'Orazio TR. Human gait analysis in neurodegenerative diseases: a review. IEEE J Biomed Health Inform. 2022 Jan;26(1):229-42.
- ↑ Yan S-H, Liu Y-C, Li W, Zhang K. Gait phase detection by using a portable system and artificial neural network. Medicine in Novel Technology and Devices. 2021;12:100092.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Physiopedia. Gait Cycle http://www.physio-pedia.com/Gait_Cycle (accessed 5 February 2015)
- ↑ Global HELP Organization. Understanding & Analyzing Gait For The Clinician: Part 05 [The Gait Cycle] May 2018. Available from: https://youtu.be/96nLX6sm9Yw.
- ↑ Di Gregorio R, Vocenas L. Identification of gait-cycle phases for prosthesis control. Biomimetics (Basel). 2021 Mar 26;6(2):22.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 Kishner's Gait Analysis after Amputation updated July 2013 http://emedicine.medscape.com/article/1237638-overview (accessed 3 February 2015)
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 10.8 Smith D,, Michael J, W and Bowker J,H American Academy of Orthopaedic Surgeons. Atlas of Amputations and Limb deficiencies. Surgical, prosthetic and rehabilitation Principles. 3rd Ed. USA. 2011
- ↑ 11.0 11.1 11.2 Australian Physiotherapists in Amputee Rehabilitation http://austpar.com (accessed 7 February 2015)
- ↑ 12.0 12.1 12.2 Harandi VJ, Ackland DC, Haddara R, Lizama LE, Graf M, Galea MP, Lee PV. Gait compensatory mechanisms in unilateral transfemoral amputees. Medical Engineering & Physics. 2020 Jan 7.
- ↑ American Academy of Orthotists and Prosthetists. Prosthetic Observational Gait Scale (POGS). Dec 2017. Available from: https://youtu.be/Syv3vfwm2Js
- ↑ 14.0 14.1 14.2 Gailey R,S and Curtis R,C. Physical Therapy Management of Adult Lower-Limb Amputees. Atlas of Limb Prosthetics; Surgical Prosthetic and Rehabilitation Principles. Chapter 23. Abridged version. O and P Virtual Library
- ↑ 15.0 15.1 British association of Chartered Physiotherapists in Amputee Rehabilitation. Evidenced Based Clinical Guidelines for the Physiotherapy Management of Adults with Lower limb Prosthesis. CSP Clinical Guideline 03. November 2012