Baker's Cyst: Difference between revisions
No edit summary |
No edit summary |
||
| (43 intermediate revisions by 6 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
A popliteal cyst, better known as Baker’s cyst, is a fluid-filled swelling that is developed at the back of the knee in the popliteal fossa region.<ref name=":0">Di Sante, L., Paoloni, M., Ioppolo, F., Dimaggio, M., Di Renzo, S., & Santilli, V. Ultrasound-guided aspiration and corticosteroid injection of Baker's cysts in knee osteoarthritis: a prospective observational study. American Journal of Physical Medicine & Rehabilitation.2010<sub>;</sub> 89(12): 970-975. </ref> Ganglia which are benign cystic tumors, originate from synovial tissue. Common areas for cyst can occur at the wrist, hand, foot, and knee.<ref name=":1">Larking P. [https://www.acc.co.nz/assets/research/knee-injury-causation-a.pdf Causation review – meniscal cysts. New Zealand: ACC]; 2010. </ref><ref>Walter B. Greene, MD - editor. 2nd edition. Essentials of Muscluloskeletal Care. Section 6, Knee and Lower leg - popliteal cyst: 2001:397-398 </ref> | |||
The cyst can exercise pressure on some anatomical structures, in most cases, the affected anatomical structure is the popliteal vein. Which can develop into thrombophlebitis.<ref name=":2">Fritschy, D., Fasel, J., Imbert, J. C., Bianchi, S., Verdonk, R., & Wirth, C. J. The popliteal cyst. ''Knee'' Surgery, Sports Traumatology, Arthroscopy. 2006'';'' ''14''(7): 623-628. </ref> | |||
{{#ev:youtube|kH6of0ipfXw|width}} | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
A Baker’s cyst is an enlarged bursa that is normally located between the medial head of the [[gastrocnemius]] and a capsular reflection of the semimembranosus, named oblique popliteal ligament. The two requirements for a cyst formation are the anatomical communication and a chronic effusion. Knee joint effusions may replete the gastrocnemius-semimembranosus bursa with synovial fluid and if the fluid outflow is hindered by a unidirectional mechanism, the gastrocnemius-semimembranosus bursa enlarges giving rise to a pseudocystic cavity, referred to as a Baker’s cyst.<ref name=":1" /> | |||
== Epidemiology /Etiology == | |||
A Baker’s cyst is an | A Baker’s cyst, or a popliteal cyst, occurs if there is an underlying intraarticular problem with the knee or and inflammatory reactions, commonly as a result of losing bodies formed in conditions such as osteoarthritis, [[Rheumatoid Arthritis|rheumatoid arthritis]], [[gout]], ACL tears, meniscal tears or because of particles following knee arthroplasty, mostly from the polyethylene liner.<ref name=":1" /><ref name=":3">Bowen, D., Gill, J. R., Pulido, P. G., Melton, J. T. K., & Cross, M. [http://abjs.mums.ac.ir/article_10279_8b8cf7c191e6a77f68519c91f08cebeb.pdf An Anteriorly Presenting ‘Wrap Around’Popliteal Cyst]. Archives of Bone and Joint Surgery.2018; 6(5): 420.</ref> | ||
* Primary Cyst: An expansion arising independently from the joint and there is no knee derangement. | |||
* Secondary Cyst: A distension of the bursa located between the gastrocnemius and semimembranosus tendons: fluid finds its way through the channel the normal bursa communicates with the joint. This is the most common occurrence<ref name=":2" /><ref name=":0" /> | |||
<br>The cyst can vary in size, from a very small (asymptomatic) to a large one but a change in size is very common. Especially in smaller cysts a septum may exist separating the semimembranosus and gastrocnemius components. This may function as a flap valve allowing fluid to enter a popliteal cyst and not to exit it. <br><br>There are differences between a popliteal cyst in children and in adults. In children, there are cystic masses filled with gelatinous material that develop in the popliteal fossa, are usually asymptomatic, and are not related to intra-articular pathology. Spontaneous resolution usually occurs, although the process can take several years. In adults, a Baker’s cyst is often found in combination with other intra-articular pathologies and inflammatory conditions. <ref name=":4">Herman, A. M., & Marzo, J. M. Popliteal cysts: a current review. Orthopedics. 2014'';37''(8):678-684.</ref><ref name=":0" /> | |||
== Clinical Presentation == | |||
== | Symptoms can include | ||
* Vague posterior pain<ref name=":1" /><ref name=":2" /><ref name=":4" /> | |||
* Swelling and a mass in the popliteal space<ref name=":1" /> | |||
* Limited range of motion<ref name=":1" /> | |||
* Stiffness in the back of the knee sometimes increased by activity<ref name=":2" /><ref name=":4" /> | |||
* Tightness behind the knee.<ref name=":1" /> | |||
Most cysts are found on the medial side of the popliteal space in the gastrocnemius-semimembranosus bursa, but they could be found in the popliteal bursa so the mass will be found on the lateral side of the popliteal space. Also, there are some rare cases in which popliteal cyst extend superiorly or anteriorly<ref name=":3" /><ref name=":10">Sanchez JE, Conkling N, Labropoulos N. [https://reader.elsevier.com/reader/sd/pii/S0741521411018349?token=C1A9236F4D30932E86D487D97A8AFC86A3F868FD10292EBAC4B8B90831EF63676D6C331592CE21A4059A52AEE03C4F89&originRegion=eu-west-1&originCreation=20220501042530 Compression syndromes of the popliteal neurovascular bundle due to Baker cyst. Journal of vascular surgery]. 2011 Dec 1;54(6):1821-9.</ref> | |||
Cysts may range in size from small, from clinically, asymptomatic and not palpable, to large masses causing visible swelling of the patient’s knee. The size of the cyst or pain can cause limitations in range of motion. If the cyst is large, it may result in mechanical problems in knee flexion and limiting mobility.<ref name=":1" />In rare cases there will be signs and symptoms of a meniscal tear which can be tested by [[McMurrays Test|McMurray test]]. | |||
Popliteal cysts can give pressure against other anatomic structures. Compression of the popliteal artery or vein can cause ischemia or thrombosis, respectively, whereas compression of the tibial or peroneal nerve can cause peripheral neuropathy. | |||
A ruptured cyst can manifest as calf pain or even swelling, it can also cause an itching feeling in the calf. There are more common in patients with an inflammatory pathology than in patients with a degenerative pathology.<ref name=":2" /> | |||
== Differential Diagnosis | == Differential Diagnosis == | ||
Baker’s cyst can be mistaken for several other injuries in the knee. The patient’s history, as well as the clinical investigation and imaging allow for proper differential diagnosis of the disease<ref name=":10" />: | |||
{| class="wikitable" | |||
! colspan="2" |Conditions presenting as soft tissue masses in the posterior leg<ref name=":5">Constantinou, M., & Vicenzino, B. [https://www.jospt.org/doi/pdf/10.2519/jospt.2005.0814 Differential diagnosis of a soft tissue mass in the calf]. Journal of Orthopaedic & Sports Physical Therapy.2005; 35(2):88-94. | |||
</ref> | |||
|- | |||
|Muscle strain or tear | |||
|Palpable mass/tenderness, swelling/warmth, pain on contraction and/or stretch of muscle | |||
|- | |||
|Muscle contusion or hematomas | |||
|Local damage to muscle (bleeding, swelling), painful muscle contraction/stretch. If the hematoma is old, organized thickening is developed | |||
|- | |||
|Muscle spasm or cramp | |||
|Painful palpable lump/thickening, possible range of motion restriction, pain on stretch of muscle | |||
|- | |||
|Fascial tear with muscle herniation | |||
|Palpable soft mass, severe muscle pain with increased activity, localized swelling post activity | |||
|- | |||
|Myositis ossificans | |||
|Palpable painful mass in the muscle, microtears in the muscle fibers that cause pain and swelling with muscle contraction or stretch, loss of motion from restricted muscle function | |||
|- | |||
|Deep vein thrombosis (DVT)5 | |||
|Constant pain, pain on passive dorsiflexion (Homan’s sign), localized warmth, localized tenderness on calf palpation and possible swelling, elevated body temperature | |||
|- | |||
|Benign tumor | |||
|Localized pain and tenderness, may be palpably soft or hard, may cause movement dysfunction (location dependent) | |||
|- | |||
|Malignant tumor | |||
|Generalized malaise, possible sudden weight loss, localized pain and/or swelling various sizes and consistency | |||
|- | |||
|Hemangioma | |||
|Present for a long time, slow changes in size over time, palpable lump, may be painful, may/may not limit motion | |||
|- | |||
|Baker’s cyst5 | |||
|Palpable lump with possible tenderness in posterior knee and posteromedial calf | |||
|- | |||
|Ruptured or enlarging Baker’s cyst (pseudothrombophlebitis) | |||
|Can mimic DVT, swelling in the calf, acute pain that worsens with compression | |||
|} | |||
Baker’s cyst | Popliteal Cyst may also confused with lipoma which would represent less resisting pressure when compared to a Baker’s cyst or aneurysm differentiated by Doppler evaluation (ultrasound). | ||
< | Some examples of supporting and negating evidence of the possible diagnoses are: | ||
{| class="wikitable" | |||
! colspan="3" |Differential diagnoses of mass in the calf muscle.<ref name=":5" /> | |||
|- | |||
!Possible Diagnosis | |||
!Supporting evidence | |||
!Negating Evidence | |||
|- | |||
|Old muscle strain or trauma with scar tissue | |||
|Palpable mass | |||
|No previous history of a muscle tear or trauma, no pain with running | |||
|- | |||
|Fascial tear with muscle herniation | |||
|Pain walking more than 0.5 km, palpable tenderness | |||
|Nonincident related, insidious onset, No pain with running or general exercise | |||
|- | |||
|Localized muscle spasm | |||
|Pain walking more than 0.5 km, palpable tenderness | |||
|No pain on passive calf stretch, no pain on resisted muscle contraction, no limitation of motion in foot or knee | |||
|- | |||
|Deep vein thrombosis (DVT) | |||
|Palpable tenderness, pain, sitting with legs crossed, family history of increased clotting factor XII in blood, taking oral contraceptive agents | |||
|No history of DVT ,no recent immobilization, no edema, no raised body temperature, negative Homan’s sign, local pulses present | |||
|- | |||
|Benign tumor | |||
|Palpable mass, palpable tenderness, insidious onset | |||
|Intermittent pain | |||
|- | |||
|Malignant tumor | |||
|Palpable mass, palpable tenderness, insidious onset | |||
|No weight loss, no night pain or feeling unwell, intermittent pain, good general health | |||
|- | |||
|Hemangioma | |||
|Insidious onset, unknown cause, hormonal changes (oral contraceptive agents), present for a long time, slow changes in size over time, palpable lump, may be painfully ,may not limit motion | |||
| | |||
|} | |||
Precise differentiation of the patient’s symptoms can be located by ultrasonography.<ref name=":2" /><ref name=":7">Handy, J. R. Popliteal cysts in adults: a review. In Seminars in Arthritis and Rheumatism. 2001; 31(2):108-118). WB Saunders. </ref> | |||
If the popliteal cyst becomes infected, this can often result in a painful mass behind the knee. In such cases, it could be difficult to make a diagnosis and the infected cyst can be mistaken for a neoplasm. The cyst can rupture (split open) resulting in severe calf pain, decreased motion at the ankle and cause similar symptoms as a deep vein thrombosis (evident on ultrasound or venogram). | |||
It is important to diagnose a ruptured Baker’s cyst early in order to determine the best treatment and avoid complications, such as compartment syndrome<ref name=":6">Torreggiani, W. C., Al-Ismail, K., Munk, P. L., Roche, C., Keogh, C., Nicolaou, S., & Marchinkow, L. O. The imaging spectrum of Baker's (popliteal) cysts. Clinical radiology.2002;''57''(8): 681-691. </ref> and to differentiate from: | |||
* Thrombophlebitis | |||
* Popliteal aneurysm | |||
* Inflammatory arthritis | |||
* Medial gastrocnemius strain | |||
* Soft-tissue tumor or muscle tear | |||
It must be considered, that Popliteal cyst can rarely present as a swelling on the anterior surface of the proximal tibia as part of the differential diagnoses when faced with a patient with a previous history of an ipsilateral total knee arthroplasty<ref name=":3" /> | |||
== Diagnostic Procedures == | |||
< | The imaging workup of knees with suspected popliteal cysts can include plain radiographs, arthrography, ultrasound, and MRI<ref name=":10" />. Early in the evaluation it can be useful to obtain plain radiographs (as posteroanterior Rosenberg, lateral, and patellofemoral axial views) for detecting other conditions found in association with popliteal cysts, such as osteoarthritis, inflammatory arthritis, and loose bodies. In addition, loose bodies may be seen in a Baker’s cyst on plain radiographs. | ||
<br>in | <br>At first, direct arthrography was used for detecting popliteal cysts. Direct arthrography involved intra-articular injection of the knee with gas or an iodinated contrast medium, followed by mobilization of the joint to force the contrast into the cyst. Afterwards, spot radiographs or fluoroscopy were used to detect the presence of the contrast in the cysts. The disadventages of this technique include the use of ionizing radiation and the use of invasive techniques to inject the contrast. | ||
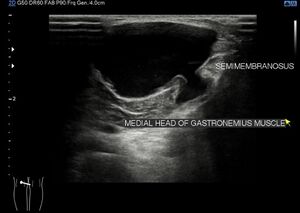
<br>The advantages of ultrasound provide a replacement of arthrography by ultrasound. The advantages are its low cost, noninvasive usage and the absence of radiation. The main disadvantage is the fact that it is user dependent. Ultrasound is able to detect Baker’s cysts near 100% but lacks to differentiate from other conditions, such as meniscal cysts or myxoid tumors, it also doesn’t visualize other conditions in the knee that are often associated with these cysts. | |||
<br>The gold standard for diagnosis of Baker’s cysts and differentiating them from other conditions remains magnetic resonance imaging. It allows to assess soft tissue abnormalities and has the added advantage of being accurate at diagnosing associated joint disorders<ref name=":6" /> so the entire spectrum of related disorders is possible to assess | |||
{| class="FCK__ShowTableBorders" border="0" cellspacing="1" cellpadding="1 | Conditions such as meniscal cysts are more easily differentiated from Baker’s cysts with MRI than ultrasound. This may be the gold standard but is also a high-cost technique, therefore, ultrasound should be considered as a screening modality if the evaluation of the intra-articular structures is not necessary.<ref name=":8">Frush, T. J., & Noyes, F. R. Baker’s cyst: diagnostic and surgical considerations. Sports health.2015;''7''(4): 359-365.</ref><br> | ||
{| class="FCK__ShowTableBorders" width="100%" border="0" cellspacing="1" cellpadding="1" | |||
|- | |- | ||
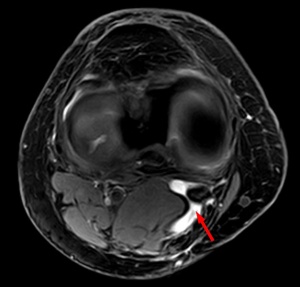
| [[Image:Bakers-cyst.jpg|thumb|center|Baker's cyst on axial MRI with communicating channel between the semimembranosus muscle and the medial head of the gastrocnemius muscle]] | | [[Image:Bakers-cyst.jpg|thumb|center|Baker's cyst on axial MRI with communicating channel between the semimembranosus muscle and the medial head of the gastrocnemius muscle]] | ||
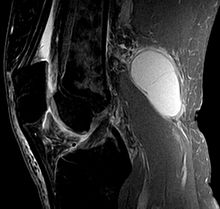
| [[Image:Bakers-cyst-MRI.jpg|thumb|center|220px|Baker's cyst on MRI, sagittal image]] | | [[Image:Bakers-cyst-MRI.jpg|thumb|center|220px|Baker's cyst on MRI, sagittal image]] | ||
|} | |} | ||
[[File:Baker-cyst-3.jpg|center|thumb|Ultrasoud image of Baker's cyst. Fluid filled cyst noted between the medial head of the gastrocnemius and the semimembranosus tendon taking appearance of a "speech bubble".]] | |||
<br> | |||
== Outcome measures == | |||
< | Outcome measures are used to determine and evaluate the expected results of the therapy/procedure to be compared to the results found within the patient. | ||
# Western Ontario and McCaster universities pain subscale (WOMAC): Is a multidimensional instrument that measures 17 functional activities. 5 pain-related activities and joint stiffness categories. It measures pain and dysfunction | |||
< | # Visual analog scale (VAS): It measures pain on a line from 0 to 10. From no pain to extreme pain. It is easy or the patient to mark how much pain he/she has.T | ||
# The Rauschning and Lindgren classification(RL): was used to evaluate the outcome and therapeutic efficacy. Grading is from 0 to 3 | |||
# The Newcastle-ottawa scale(NOS): Is a simple scale to evaluate the quality of non-randomized controlled studies <ref name=":9">Di Sante, L., Paoloni, M., Dimaggio, M., Colella, L., Cerino, A., Bernetti, A., ... & Santilli, V. [https://www.minervamedica.it/en/getfreepdf/kSdYauUxSB2ntzYZI2aorslB5rQfXPsfqC2lwDZjQ8xMzZF8asWua0NBK649cO%252B%252BOxh16gBbsdZ11i39P6vWeQ%253D%253D/R33Y2012N04A0561.pdf Ultrasound-guided aspiration and corticosteroid injection compared to horizontal therapy for treatment of knee osteoarthritis complicated with Baker’s cyst: a randomized, controlled trial]. Eur J Phys Rehabil Med.2012; ''48''(4): 561-7.</ref><ref>Zhou, X. N., Li, B., Wang, J. S., & Bai, L. H. [https://josr-online.biomedcentral.com/track/pdf/10.1186/s13018-016-0356-3 Surgical treatment of popliteal cyst: a systematic review and meta-analysis]. Journal of orthopaedic surgery and research.2016;11(1): 22. </ref><ref>Bandinelli, F., Fedi, R., Generini, S., Porta, F., Candelieri, A., Mannoni, A., ... & Cerinic, M. M. (2012). Longitudinal ultrasound and clinical follow-up of Baker’s cysts injection with steroids in knee osteoarthritis. Clinical rheumatology. 2012;''31''(4):727-731.</ref> | |||
== Examination == | |||
<div>The examination is more of clinical observation and ruling out other possible conditions. If infected or severe conditions, radiological investigations may be helpful. | |||
== Examination | Patients with a Baker’s cyst commonly have symptoms of meniscal or chondral pathology which can be tested by McMurray test.<ref name=":6" /> Symptoms related to a popliteal cyst are rare. If these symptoms are present, they may be related to the size of the cyst and include posterior or posteromedial fullness and achiness, mass and stiffness. The most common symptoms are popliteal swelling and posterior aching. Patients may also complain of pain that occurs with terminal knee extension.<ref name=":8" /> During the examination testing of knee flexion can be useful. | ||
<div>The examination is more of clinical observation and ruling out other possible conditions. If infected or severe conditions, | |||
Patients with large cysts may develop loss of knee flexion because the cysts mechanically block flexion. The examination will often reveal knee meniscal or chondral pathology, there can be palpable posteromedial fullness or tenderness. A palpable cyst is often firm in full knee extension and soft in knee flexion. This finding is known as “Foucher's sign” and is due to cyst compression. With extension, the gastrocnemius and the semimembranosus muscles approximate each other and the joint capsule compressing the cyst against the deep fascia. The mechanism of Foucher’s sign is useful for distinguishing Baker’s cysts from lesions such as popliteal artery aneurysms, adventitial cysts, ganglia, and sarcomas, for which the palpation of the mass is unaffected by the knee position, therefore this is considered the test for finding a Baker's cyst.<ref name=":4" /><ref>Canoso, J. J., Goldsmith, M. R., Gerzof, S. G., & Wohlgethan, J. R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1002105/pdf/annrheumd00282-0052.pdf Foucher's sign of the Baker's cyst]. Annals of the rheumatic diseases. 1987; ''46''(3): 228.</ref> | |||
</div> | |||
== Medical Management == | == Medical Management == | ||
Sometimes no treatment or simple supportive measures lead to spontaneous resolution or to a reduction of the symptoms. If this does not happen, invasive and surgical techniques may be an option.<ref name=":2" /><ref name=":4" /> | |||
The asymptomatic popliteal cyst often gets better and disappears by itself over time. If symptomatic, rest can temper the pain that bursa is causing, take non-steroidal anti-inflammatory drugs (NSAID) to alleviate the pain and restrict movement, also alternate with ice. | |||
By a popliteal cyst of inflammatory origin it is enough to treat the underlying disease. When the underlying disease doesn’t get treated, the Baker’s cyst can come back. Arthroscopic examination should be performed and all pathologic conditions treated before considering the excision of a popliteal cyst. | If the pain persists, a subsequent steroid injection with a solution of anesthetic and steroid can be advised which can relieve pain, but not prevent recurrence of the cyst. It’s only a temporary solution.<ref name=":2" />By a popliteal cyst of inflammatory origin, it is enough to treat the underlying disease. When the underlying disease doesn’t get treated, the Baker’s cyst can come back. Arthroscopic examination should be performed and all pathologic conditions treated before considering the excision of a popliteal cyst.<ref name=":2" /> | ||
The cyst can be removed with surgery if it becomes very large or causes symptoms such as discomfort, stiffness or painful swelling.<ref name=":6" /><ref name=":7" /> There are three surgical techniques available to treat the cyst: common posterior approach, the posteromedial approach, and the medial intra-articular approach. The first two techniques are techniques where the cyst is going to be removed. In the last technique, they make an opening in the cyst and close it afterward. The popliteal cyst will eventually disappear.<ref name=":2" /> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. The treatment is based on the principles of R.I.C.E (rest, ice, compression, and elevation) followed by some muscle-conditioning exercises. | An ice massage<ref name=":11">Website-peak-physio.com.au.Available from:https://www.peak-physio.com.au/education/bakers-cyst/ [Last Accessed 02/05/2022]</ref> of 15 minutes every 4-7 hours will reduce the inflammation. The treatment is based on the principles of R.I.C.E (rest, ice, compression, and elevation) followed by some muscle-conditioning exercises. | ||
A rehabilitation program can improve the control of the knee joint by range of motion exercises<ref name=":11" />. It will increase the motion of the joint as well as increase flexibility. The physiotherapist will give a mobility, a hamstring stretching program and a concurrent quadriceps strengthening program that has to repeat several times a day. This will result in less pain at about 6-8 weeks. | |||
{| class="FCK__ShowTableBorders" cellspacing="1" cellpadding="1 | There is an experiment comparing ultrasound guided corticosteroid injections with a horizontal therapy. 60 people were divided in three groups, only injections (group A), only horizontal therapy (group B) and (group C) they got both the injections and the horizontal therapy. The horizontal therapy was delivered through a specific commercial device, and they followed the instructions, provided by the manufacturer. Patients in groups A and C had a lower level of pain after one month. Group C had the lowest VAS scores and group C also scored best on the WOMAC. In group B and C the stiffness and disability scores were also improved the most.<ref name=":9" /> | ||
{| class="FCK__ShowTableBorders" width="100%" cellspacing="1" cellpadding="1" | |||
|- | |- | ||
| {{#ev:youtube|xjX9jBWXLkM|300}} <ref>Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]</ref> | | {{#ev:youtube|xjX9jBWXLkM|300}} <ref>Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]</ref> | ||
| {{#ev:youtube|ETorNuyS4JA|300}}<ref>TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]</ref> | | {{#ev:youtube|ETorNuyS4JA|300}}<ref>TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]</ref> | ||
|} | |} | ||
== Clinical bottom line == | |||
Baker’s cysts have different causes, therefore finding one solution is difficult. The most common treatments are invasive, such as corticosteroid injections<ref name=":0" /> and NSAID or surgery. When the pain is worse, an injection can help to relieve the pain. However, it cannot ensure that the cyst will not come back. Often the cyst disappears by itself. However, this is not always the case. A patient who has a lot of pain from the Baker’s cyst may use ice<ref>Website-Musculaskeletal Australia. Available from:https://msk.org.au/ [Last accessed 01/05/2022]</ref> or NSAID, in order to reduce the pain. At this stage, there is a need for more research on physical therapy, applied on Baker’s cyst patients. | |||
== References == | == References == | ||
<references /> | |||
[[Category:Knee]] | |||
[[Category:Conditions]] | |||
[[Category:Knee]] [[Category: | [[Category:Knee - Conditions]] | ||
Latest revision as of 14:56, 2 May 2022
Original Editor - Agapi Hakobyan
Top Contributors - Claudia Karina, Admin, Sheik Abdul Khadir, Chenoa Morales Caceres, Laura Ritchie, Kaviesha Madurapperuma, Agapi Hakobyan, Kim Jackson, Candace Goh, WikiSysop, Evan Thomas and Scott Buxton
Definition/Description[edit | edit source]
A popliteal cyst, better known as Baker’s cyst, is a fluid-filled swelling that is developed at the back of the knee in the popliteal fossa region.[1] Ganglia which are benign cystic tumors, originate from synovial tissue. Common areas for cyst can occur at the wrist, hand, foot, and knee.[2][3]
The cyst can exercise pressure on some anatomical structures, in most cases, the affected anatomical structure is the popliteal vein. Which can develop into thrombophlebitis.[4]
Clinically Relevant Anatomy[edit | edit source]
A Baker’s cyst is an enlarged bursa that is normally located between the medial head of the gastrocnemius and a capsular reflection of the semimembranosus, named oblique popliteal ligament. The two requirements for a cyst formation are the anatomical communication and a chronic effusion. Knee joint effusions may replete the gastrocnemius-semimembranosus bursa with synovial fluid and if the fluid outflow is hindered by a unidirectional mechanism, the gastrocnemius-semimembranosus bursa enlarges giving rise to a pseudocystic cavity, referred to as a Baker’s cyst.[2]
Epidemiology /Etiology[edit | edit source]
A Baker’s cyst, or a popliteal cyst, occurs if there is an underlying intraarticular problem with the knee or and inflammatory reactions, commonly as a result of losing bodies formed in conditions such as osteoarthritis, rheumatoid arthritis, gout, ACL tears, meniscal tears or because of particles following knee arthroplasty, mostly from the polyethylene liner.[2][5]
- Primary Cyst: An expansion arising independently from the joint and there is no knee derangement.
- Secondary Cyst: A distension of the bursa located between the gastrocnemius and semimembranosus tendons: fluid finds its way through the channel the normal bursa communicates with the joint. This is the most common occurrence[4][1]
The cyst can vary in size, from a very small (asymptomatic) to a large one but a change in size is very common. Especially in smaller cysts a septum may exist separating the semimembranosus and gastrocnemius components. This may function as a flap valve allowing fluid to enter a popliteal cyst and not to exit it.
There are differences between a popliteal cyst in children and in adults. In children, there are cystic masses filled with gelatinous material that develop in the popliteal fossa, are usually asymptomatic, and are not related to intra-articular pathology. Spontaneous resolution usually occurs, although the process can take several years. In adults, a Baker’s cyst is often found in combination with other intra-articular pathologies and inflammatory conditions. [6][1]
Clinical Presentation[edit | edit source]
Symptoms can include
- Vague posterior pain[2][4][6]
- Swelling and a mass in the popliteal space[2]
- Limited range of motion[2]
- Stiffness in the back of the knee sometimes increased by activity[4][6]
- Tightness behind the knee.[2]
Most cysts are found on the medial side of the popliteal space in the gastrocnemius-semimembranosus bursa, but they could be found in the popliteal bursa so the mass will be found on the lateral side of the popliteal space. Also, there are some rare cases in which popliteal cyst extend superiorly or anteriorly[5][7]
Cysts may range in size from small, from clinically, asymptomatic and not palpable, to large masses causing visible swelling of the patient’s knee. The size of the cyst or pain can cause limitations in range of motion. If the cyst is large, it may result in mechanical problems in knee flexion and limiting mobility.[2]In rare cases there will be signs and symptoms of a meniscal tear which can be tested by McMurray test.
Popliteal cysts can give pressure against other anatomic structures. Compression of the popliteal artery or vein can cause ischemia or thrombosis, respectively, whereas compression of the tibial or peroneal nerve can cause peripheral neuropathy.
A ruptured cyst can manifest as calf pain or even swelling, it can also cause an itching feeling in the calf. There are more common in patients with an inflammatory pathology than in patients with a degenerative pathology.[4]
Differential Diagnosis[edit | edit source]
Baker’s cyst can be mistaken for several other injuries in the knee. The patient’s history, as well as the clinical investigation and imaging allow for proper differential diagnosis of the disease[7]:
| Conditions presenting as soft tissue masses in the posterior leg[8] | |
|---|---|
| Muscle strain or tear | Palpable mass/tenderness, swelling/warmth, pain on contraction and/or stretch of muscle |
| Muscle contusion or hematomas | Local damage to muscle (bleeding, swelling), painful muscle contraction/stretch. If the hematoma is old, organized thickening is developed |
| Muscle spasm or cramp | Painful palpable lump/thickening, possible range of motion restriction, pain on stretch of muscle |
| Fascial tear with muscle herniation | Palpable soft mass, severe muscle pain with increased activity, localized swelling post activity |
| Myositis ossificans | Palpable painful mass in the muscle, microtears in the muscle fibers that cause pain and swelling with muscle contraction or stretch, loss of motion from restricted muscle function |
| Deep vein thrombosis (DVT)5 | Constant pain, pain on passive dorsiflexion (Homan’s sign), localized warmth, localized tenderness on calf palpation and possible swelling, elevated body temperature |
| Benign tumor | Localized pain and tenderness, may be palpably soft or hard, may cause movement dysfunction (location dependent) |
| Malignant tumor | Generalized malaise, possible sudden weight loss, localized pain and/or swelling various sizes and consistency |
| Hemangioma | Present for a long time, slow changes in size over time, palpable lump, may be painful, may/may not limit motion |
| Baker’s cyst5 | Palpable lump with possible tenderness in posterior knee and posteromedial calf |
| Ruptured or enlarging Baker’s cyst (pseudothrombophlebitis) | Can mimic DVT, swelling in the calf, acute pain that worsens with compression |
Popliteal Cyst may also confused with lipoma which would represent less resisting pressure when compared to a Baker’s cyst or aneurysm differentiated by Doppler evaluation (ultrasound).
Some examples of supporting and negating evidence of the possible diagnoses are:
| Differential diagnoses of mass in the calf muscle.[8] | ||
|---|---|---|
| Possible Diagnosis | Supporting evidence | Negating Evidence |
| Old muscle strain or trauma with scar tissue | Palpable mass | No previous history of a muscle tear or trauma, no pain with running |
| Fascial tear with muscle herniation | Pain walking more than 0.5 km, palpable tenderness | Nonincident related, insidious onset, No pain with running or general exercise |
| Localized muscle spasm | Pain walking more than 0.5 km, palpable tenderness | No pain on passive calf stretch, no pain on resisted muscle contraction, no limitation of motion in foot or knee |
| Deep vein thrombosis (DVT) | Palpable tenderness, pain, sitting with legs crossed, family history of increased clotting factor XII in blood, taking oral contraceptive agents | No history of DVT ,no recent immobilization, no edema, no raised body temperature, negative Homan’s sign, local pulses present |
| Benign tumor | Palpable mass, palpable tenderness, insidious onset | Intermittent pain |
| Malignant tumor | Palpable mass, palpable tenderness, insidious onset | No weight loss, no night pain or feeling unwell, intermittent pain, good general health |
| Hemangioma | Insidious onset, unknown cause, hormonal changes (oral contraceptive agents), present for a long time, slow changes in size over time, palpable lump, may be painfully ,may not limit motion | |
Precise differentiation of the patient’s symptoms can be located by ultrasonography.[4][9]
If the popliteal cyst becomes infected, this can often result in a painful mass behind the knee. In such cases, it could be difficult to make a diagnosis and the infected cyst can be mistaken for a neoplasm. The cyst can rupture (split open) resulting in severe calf pain, decreased motion at the ankle and cause similar symptoms as a deep vein thrombosis (evident on ultrasound or venogram).
It is important to diagnose a ruptured Baker’s cyst early in order to determine the best treatment and avoid complications, such as compartment syndrome[10] and to differentiate from:
- Thrombophlebitis
- Popliteal aneurysm
- Inflammatory arthritis
- Medial gastrocnemius strain
- Soft-tissue tumor or muscle tear
It must be considered, that Popliteal cyst can rarely present as a swelling on the anterior surface of the proximal tibia as part of the differential diagnoses when faced with a patient with a previous history of an ipsilateral total knee arthroplasty[5]
Diagnostic Procedures[edit | edit source]
The imaging workup of knees with suspected popliteal cysts can include plain radiographs, arthrography, ultrasound, and MRI[7]. Early in the evaluation it can be useful to obtain plain radiographs (as posteroanterior Rosenberg, lateral, and patellofemoral axial views) for detecting other conditions found in association with popliteal cysts, such as osteoarthritis, inflammatory arthritis, and loose bodies. In addition, loose bodies may be seen in a Baker’s cyst on plain radiographs.
At first, direct arthrography was used for detecting popliteal cysts. Direct arthrography involved intra-articular injection of the knee with gas or an iodinated contrast medium, followed by mobilization of the joint to force the contrast into the cyst. Afterwards, spot radiographs or fluoroscopy were used to detect the presence of the contrast in the cysts. The disadventages of this technique include the use of ionizing radiation and the use of invasive techniques to inject the contrast.
The advantages of ultrasound provide a replacement of arthrography by ultrasound. The advantages are its low cost, noninvasive usage and the absence of radiation. The main disadvantage is the fact that it is user dependent. Ultrasound is able to detect Baker’s cysts near 100% but lacks to differentiate from other conditions, such as meniscal cysts or myxoid tumors, it also doesn’t visualize other conditions in the knee that are often associated with these cysts.
The gold standard for diagnosis of Baker’s cysts and differentiating them from other conditions remains magnetic resonance imaging. It allows to assess soft tissue abnormalities and has the added advantage of being accurate at diagnosing associated joint disorders[10] so the entire spectrum of related disorders is possible to assess
Conditions such as meniscal cysts are more easily differentiated from Baker’s cysts with MRI than ultrasound. This may be the gold standard but is also a high-cost technique, therefore, ultrasound should be considered as a screening modality if the evaluation of the intra-articular structures is not necessary.[11]
Outcome measures[edit | edit source]
Outcome measures are used to determine and evaluate the expected results of the therapy/procedure to be compared to the results found within the patient.
- Western Ontario and McCaster universities pain subscale (WOMAC): Is a multidimensional instrument that measures 17 functional activities. 5 pain-related activities and joint stiffness categories. It measures pain and dysfunction
- Visual analog scale (VAS): It measures pain on a line from 0 to 10. From no pain to extreme pain. It is easy or the patient to mark how much pain he/she has.T
- The Rauschning and Lindgren classification(RL): was used to evaluate the outcome and therapeutic efficacy. Grading is from 0 to 3
- The Newcastle-ottawa scale(NOS): Is a simple scale to evaluate the quality of non-randomized controlled studies [12][13][14]
Examination[edit | edit source]
Patients with a Baker’s cyst commonly have symptoms of meniscal or chondral pathology which can be tested by McMurray test.[10] Symptoms related to a popliteal cyst are rare. If these symptoms are present, they may be related to the size of the cyst and include posterior or posteromedial fullness and achiness, mass and stiffness. The most common symptoms are popliteal swelling and posterior aching. Patients may also complain of pain that occurs with terminal knee extension.[11] During the examination testing of knee flexion can be useful.
Patients with large cysts may develop loss of knee flexion because the cysts mechanically block flexion. The examination will often reveal knee meniscal or chondral pathology, there can be palpable posteromedial fullness or tenderness. A palpable cyst is often firm in full knee extension and soft in knee flexion. This finding is known as “Foucher's sign” and is due to cyst compression. With extension, the gastrocnemius and the semimembranosus muscles approximate each other and the joint capsule compressing the cyst against the deep fascia. The mechanism of Foucher’s sign is useful for distinguishing Baker’s cysts from lesions such as popliteal artery aneurysms, adventitial cysts, ganglia, and sarcomas, for which the palpation of the mass is unaffected by the knee position, therefore this is considered the test for finding a Baker's cyst.[6][15]
Medical Management[edit | edit source]
Sometimes no treatment or simple supportive measures lead to spontaneous resolution or to a reduction of the symptoms. If this does not happen, invasive and surgical techniques may be an option.[4][6]
The asymptomatic popliteal cyst often gets better and disappears by itself over time. If symptomatic, rest can temper the pain that bursa is causing, take non-steroidal anti-inflammatory drugs (NSAID) to alleviate the pain and restrict movement, also alternate with ice.
If the pain persists, a subsequent steroid injection with a solution of anesthetic and steroid can be advised which can relieve pain, but not prevent recurrence of the cyst. It’s only a temporary solution.[4]By a popliteal cyst of inflammatory origin, it is enough to treat the underlying disease. When the underlying disease doesn’t get treated, the Baker’s cyst can come back. Arthroscopic examination should be performed and all pathologic conditions treated before considering the excision of a popliteal cyst.[4]
The cyst can be removed with surgery if it becomes very large or causes symptoms such as discomfort, stiffness or painful swelling.[10][9] There are three surgical techniques available to treat the cyst: common posterior approach, the posteromedial approach, and the medial intra-articular approach. The first two techniques are techniques where the cyst is going to be removed. In the last technique, they make an opening in the cyst and close it afterward. The popliteal cyst will eventually disappear.[4]
Physical Therapy Management[edit | edit source]
An ice massage[16] of 15 minutes every 4-7 hours will reduce the inflammation. The treatment is based on the principles of R.I.C.E (rest, ice, compression, and elevation) followed by some muscle-conditioning exercises.
A rehabilitation program can improve the control of the knee joint by range of motion exercises[16]. It will increase the motion of the joint as well as increase flexibility. The physiotherapist will give a mobility, a hamstring stretching program and a concurrent quadriceps strengthening program that has to repeat several times a day. This will result in less pain at about 6-8 weeks.
There is an experiment comparing ultrasound guided corticosteroid injections with a horizontal therapy. 60 people were divided in three groups, only injections (group A), only horizontal therapy (group B) and (group C) they got both the injections and the horizontal therapy. The horizontal therapy was delivered through a specific commercial device, and they followed the instructions, provided by the manufacturer. Patients in groups A and C had a lower level of pain after one month. Group C had the lowest VAS scores and group C also scored best on the WOMAC. In group B and C the stiffness and disability scores were also improved the most.[12]
| [17] | [18] |
Clinical bottom line[edit | edit source]
Baker’s cysts have different causes, therefore finding one solution is difficult. The most common treatments are invasive, such as corticosteroid injections[1] and NSAID or surgery. When the pain is worse, an injection can help to relieve the pain. However, it cannot ensure that the cyst will not come back. Often the cyst disappears by itself. However, this is not always the case. A patient who has a lot of pain from the Baker’s cyst may use ice[19] or NSAID, in order to reduce the pain. At this stage, there is a need for more research on physical therapy, applied on Baker’s cyst patients.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Di Sante, L., Paoloni, M., Ioppolo, F., Dimaggio, M., Di Renzo, S., & Santilli, V. Ultrasound-guided aspiration and corticosteroid injection of Baker's cysts in knee osteoarthritis: a prospective observational study. American Journal of Physical Medicine & Rehabilitation.2010; 89(12): 970-975.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Larking P. Causation review – meniscal cysts. New Zealand: ACC; 2010.
- ↑ Walter B. Greene, MD - editor. 2nd edition. Essentials of Muscluloskeletal Care. Section 6, Knee and Lower leg - popliteal cyst: 2001:397-398
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Fritschy, D., Fasel, J., Imbert, J. C., Bianchi, S., Verdonk, R., & Wirth, C. J. The popliteal cyst. Knee Surgery, Sports Traumatology, Arthroscopy. 2006; 14(7): 623-628.
- ↑ 5.0 5.1 5.2 Bowen, D., Gill, J. R., Pulido, P. G., Melton, J. T. K., & Cross, M. An Anteriorly Presenting ‘Wrap Around’Popliteal Cyst. Archives of Bone and Joint Surgery.2018; 6(5): 420.
- ↑ 6.0 6.1 6.2 6.3 6.4 Herman, A. M., & Marzo, J. M. Popliteal cysts: a current review. Orthopedics. 2014;37(8):678-684.
- ↑ 7.0 7.1 7.2 Sanchez JE, Conkling N, Labropoulos N. Compression syndromes of the popliteal neurovascular bundle due to Baker cyst. Journal of vascular surgery. 2011 Dec 1;54(6):1821-9.
- ↑ 8.0 8.1 Constantinou, M., & Vicenzino, B. Differential diagnosis of a soft tissue mass in the calf. Journal of Orthopaedic & Sports Physical Therapy.2005; 35(2):88-94.
- ↑ 9.0 9.1 Handy, J. R. Popliteal cysts in adults: a review. In Seminars in Arthritis and Rheumatism. 2001; 31(2):108-118). WB Saunders.
- ↑ 10.0 10.1 10.2 10.3 Torreggiani, W. C., Al-Ismail, K., Munk, P. L., Roche, C., Keogh, C., Nicolaou, S., & Marchinkow, L. O. The imaging spectrum of Baker's (popliteal) cysts. Clinical radiology.2002;57(8): 681-691.
- ↑ 11.0 11.1 Frush, T. J., & Noyes, F. R. Baker’s cyst: diagnostic and surgical considerations. Sports health.2015;7(4): 359-365.
- ↑ 12.0 12.1 Di Sante, L., Paoloni, M., Dimaggio, M., Colella, L., Cerino, A., Bernetti, A., ... & Santilli, V. Ultrasound-guided aspiration and corticosteroid injection compared to horizontal therapy for treatment of knee osteoarthritis complicated with Baker’s cyst: a randomized, controlled trial. Eur J Phys Rehabil Med.2012; 48(4): 561-7.
- ↑ Zhou, X. N., Li, B., Wang, J. S., & Bai, L. H. Surgical treatment of popliteal cyst: a systematic review and meta-analysis. Journal of orthopaedic surgery and research.2016;11(1): 22.
- ↑ Bandinelli, F., Fedi, R., Generini, S., Porta, F., Candelieri, A., Mannoni, A., ... & Cerinic, M. M. (2012). Longitudinal ultrasound and clinical follow-up of Baker’s cysts injection with steroids in knee osteoarthritis. Clinical rheumatology. 2012;31(4):727-731.
- ↑ Canoso, J. J., Goldsmith, M. R., Gerzof, S. G., & Wohlgethan, J. R. Foucher's sign of the Baker's cyst. Annals of the rheumatic diseases. 1987; 46(3): 228.
- ↑ 16.0 16.1 Website-peak-physio.com.au.Available from:https://www.peak-physio.com.au/education/bakers-cyst/ [Last Accessed 02/05/2022]
- ↑ Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]
- ↑ TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]
- ↑ Website-Musculaskeletal Australia. Available from:https://msk.org.au/ [Last accessed 01/05/2022]