Atrial Fibrillation: Difference between revisions
No edit summary |
No edit summary |
||
| (119 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''[[Stroke|Original]] Editors '''- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]]<br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | |||
== Introduction == | |||
[[File:Atrial_Fibrillation_TPMJM_BUDPT.png|right|528x528px]] | |||
Atrial fibrillation is the most common type of [[Heart Arrhythmias: Assessment|heart arrhythmia]]. It is due to abnormal electrical activity within the atria of the [[Anatomy of the Human Heart|heart]] causing them to fibrillate. Is characterized as a tachyarrhythmia ie the [[Heart Rate|heart rate]] is often fast. Due to its rhythm irregularity, blood flow through the heart becomes turbulent and has a high chance of forming a thrombus which can dislodge and embolize to the [[Brain Anatomy|brain]] and other parts of the body<ref name=":8">Nesheiwat Z, Jagtap M. [https://www.ncbi.nlm.nih.gov/books/NBK526072/ Rhythm, Atrial Fibrillation (A Fib).] InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526072/ (last accessed 11.1.2020)</ref>. | |||
Watch this 1 minute video on AF{{#ev:youtube|pgOHs3NTmIY}} | |||
== Etiology == | |||
[[File:RiskFactors.jpg|thumb|471x471px|AF risk factors]] | |||
The risk of developing AF is substantially higher in elderly individuals. Common causes of AF include long-term high blood pressure, coronary heart disease and valvular heart disease. Other risks for AF include obesity, having a thyroid condition, diabetes, chronic kidney disease, obstructive sleep apnoea, and smoking or consuming alcohol excessively. For some people, there is no apparent cause.<ref name=":0">AIHW Atrial fibrillation in Australia Available:https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/atrial-fibrillation-in-australia/contents/what-is-atrial-fibrillation (accessed 3.2.2022)</ref> | |||
The 3 patterns of atrial fibrillation include: | |||
# Paroxysmal AF: Here the episodes terminate spontaneously within 7 days. | |||
# Persistent AF: The episodes last more than 7 days and often require electrical or pharmacological interventions to terminate the rhythm | |||
# Long-standing persistent AD: rhythm that has persisted for more than 12 months, either because a pharmacological intervention has not been tried or cardioversion has failed.<ref name=":8" />. | |||
== Epidemiology/Prevalence == | |||
The prevalence of atrial fibrillation has been increasing worldwide. It is known that the prevalence of atrial fibrillation generally increases with age. At the age of 80, the lifetime risk of developing atrial fibrillation jumps to 22%.<ref name=":3">Atrial Fibrillation Fact Sheet [Internet]. Center for Disease Control and Prevention; 2013 [updated 2015 August 13; cited 2016 April 5] Available from: http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_atrial_fibrillation.htm</ref> | |||
== Pathophysiology == | |||
There are a wide variety of pathophysiology mechanisms that play a role in the development of atrial fibrillation. Most commonly, hypertension, structural, valvular, and ischemic heart disease illicit the paroxysmal and persistent forms of atrial fibrillation but the underlying pathophysiology is not well understood. Some research has shown evidence of genetic causes of atrial fibrillation involving chromosome 10.<ref name=":8" /> | |||
== Clinical Presentation == | |||
[[File:Atrial fib stroke.jpeg|thumb|AF Stoke|alt=]] | |||
== | Often, people with AF do not know that they have it, and they do not experience any symptoms. Others may experience an irregular pulse, heart palpitations (‘fluttering’), fatigue, weakness, discomfort, shortness of breath or dizziness.<ref name=":0" /> | ||
== | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
These include, but not limited to:; [[Stroke]]; [[Obesity]]; [[Sleep Apnea-Hypopnea Syndrome|Obstructive sleep apnea]]; [[Diabetes]]; [[Heart Failure|Congestive Heart Failure]]; [[Cardiac Valve Defects|Mitral valve disease]]; [[Coronary Artery|Coronary artery disease]] <ref name=":1">Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2006: 114(7): p. 257-354.</ref><ref name=":4">Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. 5th ed. St. Louis Saunders; 2012. p. 264-266.</ref><ref name=":5">Wadke R. Atrial Fibrillation. Disease-a-Month. 2013 March: 59(3): 67-73.</ref><ref name=":6">Oishi ML, Xing S. Atrial fibrillation: Management strategies in the emergency department. Emerg Med Prac. 2013: 15(2): p. 1-26.</ref><ref name=":7">Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J Kara T, Somers VK. Obstructive Sleep Apnea, Obesity, and the Risk of Incident Atrial Fibrillation. J Am Coll Cardiol [Internet]. 2007 Feb [cited 2016 April 9]; 49(5): 565-571. Available from: http://content.onlinejacc.org/article.aspx?articleid=1188673&...#tab1</ref> | |||
Stroke can occur during atrial fibrillation. A blood clot forms in the left atrium of the heart, a piece of the clot breaks off and travels to an artery in the brain. See illustration. | |||
== Diagnosis == | |||
Atrial fibrillation is usually diagnosed using an [[electrocardiogram]] (ECG). Other tests include: 24-hour heart holter monitor; Cardiogram (heart ultrasound); [[Blood Tests|Blood test]]; Stress tests; [[Six Minute Walk Test / 6 Minute Walk Test|6 minute walk test]]; Physical Exam: Irregular [[Heart Rate|heart rate]], irregular jugular venous pulsations, variation in the intensity of first heart sound.<ref name=":1" /><ref name=":2">Amerena JV, Walters TE, Mirzaee S, Kalman JM. Update on the management of atrial fibrillation. Med J Aust. 2013: 199(9): p. 592-7.</ref><ref name=":4" /><ref name=":5" /> | |||
== | |||
== Systemic Involvement == | == Systemic Involvement == | ||
High concentrations of CRP, which confirm the presence of systemic inflammation are present in people with AF | High concentrations of CRP in the [[Blood Tests|blood test]], which confirm the presence of systemic [[Inflammation Acute and Chronic|inflammation]] are present in people with Atrial Fibrillation (AF).<ref name=":1" /> | ||
Changes in an individual's health such as a newly diagnosed complication may have a psychological impact. Patients may experience [[depression]] and other psycho-social challenges as a result of changes in their health status, treatment, frequent visits to the physician's office, and fear of the unknown that may accompany a diagnosis of atrial fibrillation. | |||
== Management == | |||
[[File:Cardioversion.png|thumb|Cardioversion]] | |||
Treatment strategy in recently diagnosed cases of atrial fibrillation includes identification and solution of reversible risk factors with anticoagulation therapy followed by [[Beta-blockers in the Treatment of Hypertension|beta-blockers]].<ref>Radiopedia AF Available: https://radiopaedia.org/articles/atrial-fibrillation?lang=us<nowiki/>(accessed 3,3.2022)</ref> | |||
Non-pharmacological therapy includes ablation therapy, a hospital procedure which inactivates small areas of tissue in the heart responsible for the abnormal electrical signals associated with AF. [[Cardiac Implantable Electronic Devices (CIEDs)|Pacemaker placement]] is considered in severe causes resulting in heart failure in atrial fibrillation<ref name=":8" />. | |||
People with prolonged or severe AF may undergo [[cardioversion]]. Pharmacological cardioversion uses medicines to achieve the same purpose. After cardioversion, long-term medicines are often prescribed to help prevent AF from reoccurring<ref name=":0" />. | |||
== | == Physical Therapy Management == | ||
There is limited research on the effect of traditional physical therapy and Atrial Fibrillation. <br>There is also conflicting information on the use of exercise to reduce the risk of AF. Since obesity is an important risk factor, management of weight through exercise and education is a crucial, proactive measure that may reduce the incidence of AF. However, there is conflicting evidence in regard to the optimal prescription of exercise. | |||
== Case Reports | == Case Reports == | ||
Ezekowitz MD, Aikens TH, Nagarakanti R, Shapiro T. [http://circ.ahajournals.org/content/124/1/95.full#cited-by Atrial fibrillation: outpatient presentation and management]. Circulation. 2011; 124: 95–99. Available from: American Heart Association.<br>. | |||
== Resources | == Resources == | ||
* <u></u>AFIB matters: [http://www.afibmatters.org/Living-with-atrial-fibrillation Atrial Fibrillation] | |||
* American Heart Association: [http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/AFib-Resources-For-Patients-Professionals_UCM_423786_Article.jsp#.Vww-X4S9jzI Atrial Fibrillation Resources For Patients & Professionals] | |||
* Cleveland Clinic: [http://www.clevelandclinic.org/lp/atrial_fibrillation/index.html?searchdef=21076362156527&002=2107636&006=89400250002&007=Search&008=&009=b&012=a%20fib&021=26286861794902&025=c&026=&utm_campaign=CS+-+Heart+-+DR+-+Afib+Local&utm_medium=cpc&utm_source=google_ppc&utm_term=a+fib&utm_content=89400250002&k_clickid=d4933b79-9aaf-4351-b2b0-eab57ffb625b&gclid=CjwKEAjw86e4BRCnzuWGlpjLoUcSJACaHG55gPkgoyxTsODA4sc2FaTx-j9dd0P8TON9Rr-8A1OWBRoCCr3w_wcB&k_clickid=d4933b79-9aaf-4351-b2b0-eab57ffb625b Advanced Treatment for Atrial Fibrillation] | |||
* Mayo Clinic: [http://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/atrial-fibrillation-care-at-mayo-clinic/ovc-20164979 Atrial Fibrillation] | |||
* StopAfib.org: [http://www.stopafib.org/resources.cfm Atrial Fibrillation Resources] | |||
== References == | == References == | ||
[[Category:Bellarmine_Student_Project]] | |||
[[Category:Medical]] | |||
[[Category:Acute Care]] | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Cardiovascular Disease - Conditions]] | |||
<references /> | <references /> | ||
Latest revision as of 06:42, 3 March 2022
Top Contributors - Paul McDermott, James Moore, Lucinda hampton, Kim Jackson, Adam Vallely Farrell, Karen Wilson, Vidya Acharya, Elaine Lonnemann, George Prudden and WikiSysop
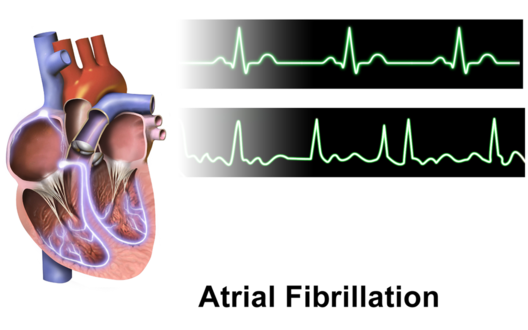
Introduction[edit | edit source]
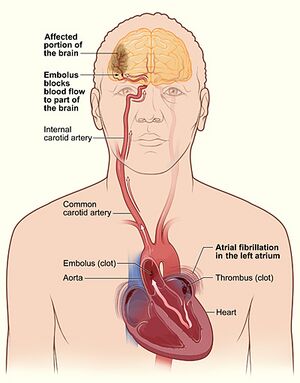
Atrial fibrillation is the most common type of heart arrhythmia. It is due to abnormal electrical activity within the atria of the heart causing them to fibrillate. Is characterized as a tachyarrhythmia ie the heart rate is often fast. Due to its rhythm irregularity, blood flow through the heart becomes turbulent and has a high chance of forming a thrombus which can dislodge and embolize to the brain and other parts of the body[1].
Watch this 1 minute video on AF
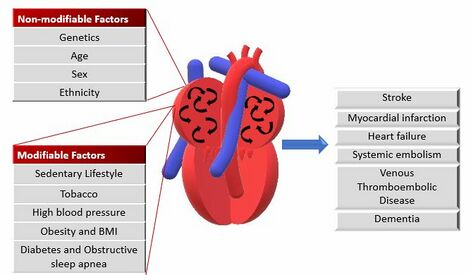
Etiology[edit | edit source]
The risk of developing AF is substantially higher in elderly individuals. Common causes of AF include long-term high blood pressure, coronary heart disease and valvular heart disease. Other risks for AF include obesity, having a thyroid condition, diabetes, chronic kidney disease, obstructive sleep apnoea, and smoking or consuming alcohol excessively. For some people, there is no apparent cause.[2]
The 3 patterns of atrial fibrillation include:
- Paroxysmal AF: Here the episodes terminate spontaneously within 7 days.
- Persistent AF: The episodes last more than 7 days and often require electrical or pharmacological interventions to terminate the rhythm
- Long-standing persistent AD: rhythm that has persisted for more than 12 months, either because a pharmacological intervention has not been tried or cardioversion has failed.[1].
Epidemiology/Prevalence[edit | edit source]
The prevalence of atrial fibrillation has been increasing worldwide. It is known that the prevalence of atrial fibrillation generally increases with age. At the age of 80, the lifetime risk of developing atrial fibrillation jumps to 22%.[3]
Pathophysiology[edit | edit source]
There are a wide variety of pathophysiology mechanisms that play a role in the development of atrial fibrillation. Most commonly, hypertension, structural, valvular, and ischemic heart disease illicit the paroxysmal and persistent forms of atrial fibrillation but the underlying pathophysiology is not well understood. Some research has shown evidence of genetic causes of atrial fibrillation involving chromosome 10.[1]
Clinical Presentation[edit | edit source]
Often, people with AF do not know that they have it, and they do not experience any symptoms. Others may experience an irregular pulse, heart palpitations (‘fluttering’), fatigue, weakness, discomfort, shortness of breath or dizziness.[2]
Associated Co-morbidities[edit | edit source]
These include, but not limited to:; Stroke; Obesity; Obstructive sleep apnea; Diabetes; Congestive Heart Failure; Mitral valve disease; Coronary artery disease [4][5][6][7][8]
Stroke can occur during atrial fibrillation. A blood clot forms in the left atrium of the heart, a piece of the clot breaks off and travels to an artery in the brain. See illustration.
Diagnosis[edit | edit source]
Atrial fibrillation is usually diagnosed using an electrocardiogram (ECG). Other tests include: 24-hour heart holter monitor; Cardiogram (heart ultrasound); Blood test; Stress tests; 6 minute walk test; Physical Exam: Irregular heart rate, irregular jugular venous pulsations, variation in the intensity of first heart sound.[4][9][5][6]
Systemic Involvement[edit | edit source]
High concentrations of CRP in the blood test, which confirm the presence of systemic inflammation are present in people with Atrial Fibrillation (AF).[4]
Changes in an individual's health such as a newly diagnosed complication may have a psychological impact. Patients may experience depression and other psycho-social challenges as a result of changes in their health status, treatment, frequent visits to the physician's office, and fear of the unknown that may accompany a diagnosis of atrial fibrillation.
Management[edit | edit source]
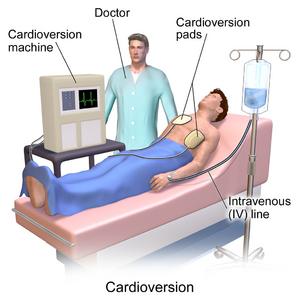
Treatment strategy in recently diagnosed cases of atrial fibrillation includes identification and solution of reversible risk factors with anticoagulation therapy followed by beta-blockers.[10]
Non-pharmacological therapy includes ablation therapy, a hospital procedure which inactivates small areas of tissue in the heart responsible for the abnormal electrical signals associated with AF. Pacemaker placement is considered in severe causes resulting in heart failure in atrial fibrillation[1].
People with prolonged or severe AF may undergo cardioversion. Pharmacological cardioversion uses medicines to achieve the same purpose. After cardioversion, long-term medicines are often prescribed to help prevent AF from reoccurring[2].
Physical Therapy Management[edit | edit source]
There is limited research on the effect of traditional physical therapy and Atrial Fibrillation.
There is also conflicting information on the use of exercise to reduce the risk of AF. Since obesity is an important risk factor, management of weight through exercise and education is a crucial, proactive measure that may reduce the incidence of AF. However, there is conflicting evidence in regard to the optimal prescription of exercise.
Case Reports[edit | edit source]
Ezekowitz MD, Aikens TH, Nagarakanti R, Shapiro T. Atrial fibrillation: outpatient presentation and management. Circulation. 2011; 124: 95–99. Available from: American Heart Association.
.
Resources[edit | edit source]
- AFIB matters: Atrial Fibrillation
- American Heart Association: Atrial Fibrillation Resources For Patients & Professionals
- Cleveland Clinic: Advanced Treatment for Atrial Fibrillation
- Mayo Clinic: Atrial Fibrillation
- StopAfib.org: Atrial Fibrillation Resources
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Nesheiwat Z, Jagtap M. Rhythm, Atrial Fibrillation (A Fib). InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526072/ (last accessed 11.1.2020)
- ↑ 2.0 2.1 2.2 AIHW Atrial fibrillation in Australia Available:https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/atrial-fibrillation-in-australia/contents/what-is-atrial-fibrillation (accessed 3.2.2022)
- ↑ Atrial Fibrillation Fact Sheet [Internet]. Center for Disease Control and Prevention; 2013 [updated 2015 August 13; cited 2016 April 5] Available from: http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_atrial_fibrillation.htm
- ↑ 4.0 4.1 4.2 Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2006: 114(7): p. 257-354.
- ↑ 5.0 5.1 Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. 5th ed. St. Louis Saunders; 2012. p. 264-266.
- ↑ 6.0 6.1 Wadke R. Atrial Fibrillation. Disease-a-Month. 2013 March: 59(3): 67-73.
- ↑ Oishi ML, Xing S. Atrial fibrillation: Management strategies in the emergency department. Emerg Med Prac. 2013: 15(2): p. 1-26.
- ↑ Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J Kara T, Somers VK. Obstructive Sleep Apnea, Obesity, and the Risk of Incident Atrial Fibrillation. J Am Coll Cardiol [Internet]. 2007 Feb [cited 2016 April 9]; 49(5): 565-571. Available from: http://content.onlinejacc.org/article.aspx?articleid=1188673&...#tab1
- ↑ Amerena JV, Walters TE, Mirzaee S, Kalman JM. Update on the management of atrial fibrillation. Med J Aust. 2013: 199(9): p. 592-7.
- ↑ Radiopedia AF Available: https://radiopaedia.org/articles/atrial-fibrillation?lang=us(accessed 3,3.2022)