Methicillin-Resistant Staphylococcus Aureus: Difference between revisions
No edit summary |
No edit summary |
||
| (75 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's | '''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Scanning electron micrograph of Methicillin-resistant Staphylococcus aureus (MRSA) and a dead Human neutrophil - NIAID.jpg|right|frameless]] | |||
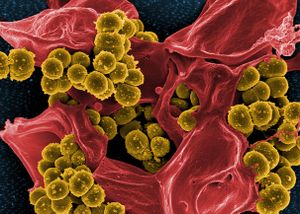
Methicillin-resistant Staphylococcus aureus (MRSA) is a [[Bacterial Infections|bacterium]] that causes infections in different parts of the body. It's tougher to treat than most strains of staphylococcus aureus -- or staph -- because it's resistant to some commonly used antibiotics. R image - scanning electronic microscope of MRSA and a dead neutrophil. | |||
MRSA infection is one of the leading causes of hospital-acquired infections and is commonly associated with significant morbidity, mortality, length of stay, and cost burden. MRSA infections can be further divided into hospital-associated (HA-MRSA) infections and community-associated (CA-MRSA) infections. They differ not only in respect to their clinical features and molecular biology but also to their antibiotic susceptibility and treatment<ref name=":0">Siddiqui AH, Koirala J. [https://www.ncbi.nlm.nih.gov/books/NBK482221/ Methicillin resistant Staphylococcus aureus (MRSA]). Available from:https://www.ncbi.nlm.nih.gov/books/NBK482221/ (last accessed 7.3.2020)</ref> | |||
= | The bacteria from which MRSA arises, staphylococcus aureus, is found in the skin and in the nostrils of one third of all people whom do not show any symptoms of having been exposed to the bacteria. These carriers of the bacteria are then exposing the bacteria to all of the items that they touch as well as expelling it into the air where it will remain until the item is next cleaned.<ref name="K4">Robinson J, Edgley A, Morrell J. MRSA care in the community: why patient education matters. British Journal of Community Nursing. 2014;19(9):436-441. http://dx.doi.org.libproxy.bellarmine.edu/10.12968/bjcn.2014.19.9.436&nbsp; (accessed 2 April 2016).</ref> | ||
=== Prevention === | |||
[[Image:Management of MRSA.jpg|right|frameless]]Prevention and control of MRSA infections include necessary infection-control steps like strict hand hygiene and adequate contact precautions. Hand hygiene means washing hands with soap and water or an alcohol-based cleanser before and after contact with patients who have MRSA infection. Contact precautions include the use of gowns, gloves, and possibly masks during clinical encounters with patients with MRSA infection. Infection control also may include keeping patients in isolated rooms or the same rooms of other patients who have an MRSA<ref name=":0" /> infection.<ref name="K4" /> | |||
== | == Etiology == | ||
Methicillin resistance has occurred in ''S. aureus'' by mutation of a penicillin-binding protein, a chromosome-encoded protein. This type of resistance is transferred between ''S. aureus'' organisms by bacteriophages. This is one of the only medically relevant examples of chromosome-mediated drug resistance by phage transduction.<ref name=":0" /> | |||
== Epidemiology == | |||
The history of MRSA infection goes back to 1961 when it was first described. Since then, the incidence and prevalence of MRSA infection have been increasing dramatically across the United States. Recently, some population studies have hinted at reducing HA-MRSA incidences in the United States but at the expense of a growing prevalence of CA-MRSA. The reported incidence of MRSA infection ranges from 7% to 60%. | |||
'''Risk Factors''' | |||
* The commonly associated risk factors for MRSA infection are prolonged hospitalization, intensive care admission, recent hospitalization, recent antibiotic use, MRSA colonization, invasive procedures, HIV infection, admission to nursing homes, open wounds, hemodialysis, and discharge with long-term central venous access or long-term indwelling urinary catheter. | |||
* A higher incidence of MRSA infection is also seen among healthcare workers who come in direct contact with patients infected with this organism. | |||
* Although advancing age by itself is not considered a risk factor for MRSA infection, age more than 65 years is a significant risk factor for hospitalization. | |||
* Living in an area with a high prevalence of CA-MRSA or admission to a hospital with a high prevalence of HA-MRSA also is considered a significant risk factor for MRSA colonization.<ref name=":0" /> | |||
== Pathophysiology == | |||
The key reason for MRSA resistance to beta-lactam antibiotics is due to the presence of the mecA gene sequence, which is known to generate transpeptidase PB2a that lowers the affinity of the organism to bind to beta-lactam antibiotics.<ref name=":0" /> | |||
== | == Clinical Presentation == | ||
[[Image:Definition of MRSA.jpg|MRSA infection.|right|frameless|250x250px]]MRSA can cause a range of organ-specific infections, the most common being the skin and subcutaneous tissues, followed by invasive infections like osteomyelitis, meningitis, pneumonia, lung abscess, and empyema. Infective endocarditis caused by MRSA is associated with an increased morbidity and mortality compared to any other organism and is linked to intravenous drug abuse. | |||
'''Skin and soft tissue infections (SSTI):''' CA-MRSA is a predominant organism associated with SSTIs like cellulitis, necrotizing fasciitis, and diabetic foot ulcers. It also is increasingly associated with more invasive disease than those due to non-MRSA. More frequently these infections are multidrug-resistant leading to frequent recurrence, increased hospitalization, and mortality. | |||
== | '''Bone and joint infection:''' Staphylococci are the most common cause of bone and joint infections. MRSA can cause osteomyelitis of spine, long bones of upper and lower extremities by extension of local infection from a wound or as a part of hematogenous infection. Similarly, MRSA can cause septic arthritis of both native and prosthetic joints. | ||
'''Pneumonia:''' Staphylococcal pneumonia - CA-MRSA can cause life-threatening necrotizing pneumonia in otherwise healthy individuals. It is characterized by severe respiratory symptoms, high fevers, hemoptysis, and hypotension. It rapidly progresses to sepsis and septic shock with leukopenia and elevated C-reactive protein. Multilobar cavitating alveolar infiltrates in a clinical setting like this is consistent with CA-MRSA infection. | |||
MRSA is also a leading cause of hospital-acquired and ventilator-associated pneumonia. | |||
'''Bacteremia:''' Bacteremia due to ''S. aureus'' has been reported to be associated with mortality rates of 15% to 60%. MRSA bacteremia is commonly seen in intensive care unit patients with central line insertions. Infective endocarditis is associated with MRSA bacteremia and should be ruled out in any patient with MRSA in the bloodstream. The outcomes related to MRSA bacteremia are worse than other MRSA infections because of the decreased response to vancomycin in these patients. | |||
'''Endocarditis:''' MRSA is an important cause of bacterial endocarditis which can cause mortality in about a third of the infected patients (30-37%). Right-sided MRSA endocarditis is commonly associated with intravenous drug use and intravenous catheters. Patients with tricuspid valve vegetations may have septic pulmonary emboli causing nodular infiltrates and cavitating lesions in the lungs. Similarly, patients with involvement of mitral and aortic valves may have secondary infections in distant foci such as bones and joints, kidneys, brain, and other organs. It is important to take history and perform a thorough examination of these patients combined with necessary labs and radiological tests.<ref name=":0" /> | |||
== Characteristics == | |||
• Chest pain<br>• Cough<br>• Shortness of breath<br>• Fatigue<br>• Fever and chills<br>• General ill feeling<br>• Headache<br>• Rash<br>• Wounds that do not heal | |||
Differences in Characteristics Between HA-MRSA and CA-MRSA<ref name="K2">Millar B, Loughrey A, Elborn J, Moore J. Proposed definitions of community-associated meticillin-resistant Staphylococcus aureus (CA-MRSA). Journal of Hospital Infection. 2007;67(2):109-113. http://eds.b.ebscohost.com.libproxy.bellarmine.edu/ehost/detail/detail?vid=14&sid=71ee6b7e-199d-4adc-8e31-bc94eca59a09%40sessionmgr113&hid=112&bdata=JmxvZ2luLmFzcCZzaXRlPWVob3N0LWxpdmUmc2NvcGU9c2l0ZQ%3d%3d#AN=105828672&db=cin20 (accessed 2 April 2016).</ref> | |||
{| width="75%" border="1" cellpadding="1" cellspacing="1" | |||
|- | |||
| '''Characteristic''' | |||
| '''HA-MRSA''' | |||
| '''CA-MRSA''' | |||
|- | |||
| Site of Infection | |||
| Bacteraemia, wound infections, respiratory tract, urinary tract | |||
| Mainly skin (abscesses, cellulitis, furunculosis | |||
|- | |||
| Risk Factors | |||
| Indwelling devices, catheters, lines, hemodialysis, prolonged hospitalization, long-term antibiotic use | |||
| Close physical contact, abrasion injuries, poor hygiene | |||
|- | |||
| Transmission | |||
| Person-to-person (healthcare staff, visitors, patients), environment-to-person (hospital equipment | |||
| Person-to-person (contact sports), environment-to-person (shared facilities, shared sports equipment) | |||
|} | |||
== | == Medical Management == | ||
The selection of empiric antibiotic therapy for the treatment of MRSA infection depends on the type of disease, local ''S. aureus'' resistance patterns, availability of the drug, side effect profile, and individual patient profile. | |||
'''SSTIs:''' For most uncomplicated SSTIs suspected of MRSA infection, empirical treatment is with oral antibiotics like trimethoprim/sulfamethoxazole, tetracyclines, such as doxycycline or minocycline, and clindamycin. | |||
Parenteral antibiotics are indicated for invasive SSTIs or with signs of systemic involvement, inadequate response to oral therapy, or if an SSTI occurs adjacent to an indwelling device. | |||
Intravenous vancomycin is the drug of choice for most MRSA infections seen in hospitalized patients. It can be used both as empiric and definitive therapy as most MRSA infections are susceptible to vancomycin. There are sporadic cases of vancomycin-resistant MRSA. | |||
Daptomycin is a suitable parenteral alternative when vancomycin is not available or not being tolerated. Other short-acting options include ceftaroline and telavancin. Long-acting treatment options include dalbavancin and oritavancin. Regardless of the initial empiric antibiotic choice, subsequent therapy should be tailored based on the careful review of culture and susceptibility data. | |||
The duration of therapy for treatment of MRSA SSTIs may range from 5 to 14 days depending on the extent of infection and response to treatment.<ref name="K4" /> | |||
== | == Diagnostic Tests/Lab Tests/Lab Values == | ||
Clinical Laboratories for MRSA, according to the Clinical and Laboratory Standards Institute (CLSI)<ref>Centers for Disease Control and Prevention. Laboratory Testing for MRSA. http://www.cdc.gov/mrsa/lab/ (accessed 8 April 2016).</ref><br> | |||
Broth Microdultion Testing with the addition of one of the following: | |||
*A plate containing 6 μg/ml of oxacillin in Mueller-Hinton agar supplemented with 4% NaCl as alternative methods of testing for MRSA | |||
*Latex Agglutination Test for PBP2 - tests for the mecA gene (Staphylococcal resistance to oxacillin/methicillin happens when an altered penicillin-binding protein, PBP2a, is produced.) | |||
*Cefoxitin Disk Screen Test<br> | |||
Typically the broth test and agar test are the main tests for detecting MRSA, and the cefoxitin disk screen test can be used as a back-up test. <br>• Detecting oxacillin/methicillin resistance can be difficult because of the presence of multiple populations (susceptible and resistant) may coexist within one culture of staphylococci.<br>• Oxacillin and cefoxitin are tested instead of methicillin because methicillin isn’t as readily available in the US as it once was. Oxacillin detects subpopulations well and cefoxitin activates mecA gene better, making it a more accurate test than other using oxacillin.<br>• Methicillin and oxacillin are in the same class of drugs. Methicillin has historically been the drug of choice for detecting resistance, hence the name MRSA. Even though the preferred drug of choice for testing has changed, the name had remained the same.<br>According to Centers for Disease Control and Prevention, there are additional tests to detect oxacillin/methicillin resistance but the most common and reliable tests have been listed above. | |||
== Physical Therapy Management == | |||
= | MRSA is not primarily managed by physical therapy. Instead it is the physical therapist’s role to identify comorbidities that are inhibiting functional activity and treat the patient’s symptoms. When treating a patient with MRSA, it’s important for the physical therapist to know proper disinfecting techniques to prevent the spread of the disease. Precautions to be taken when treating a patient with MRSA include but are not limited to:<ref>Centers for Disease Control and Prevention. Cleaning & Disinfecting Athlete Facilities. http://www.cdc.gov/mrsa/community/environment/athletic-facilities.html (accessed 8 April 2016).</ref><ref>Centers for Disease Control and Prevention. Laundry. http://www.cdc.gov/mrsa/community/environment/laundry.html (accessed 8 April 2016).</ref><ref name="Medline">MedlinePlus Medical Encyclopedia. MRSA. https://www.nlm.nih.gov/medlineplus/ency/article/007261.htm (accessed 7 April 2016).</ref> | ||
*Buy disinfectants that are registered by the Environmental Protection Agency (EPA) | |||
*Note how to properly apply each product, how long it needs to be left on the surface, if the surface needs to be rinsed prior, if it’s only for specific surfaces, etc. | |||
*Laundering specific clothes, towels and linens separately would be appropriate but not always necessary – wash and dry in the warmest temperate recommended on each piece of linen individually | |||
*All surfaces ad equipment that came in contact with the patient should be cleaned, sometimes individual equipment for the patient with MRSA may be necessary if equipment cannot be properly cleaned | |||
*Use barriers between the patient’s skin and surface when possible | |||
*Physical therapist should wash body parts immediately after making contact with patient’s skin | |||
*Patient should keep all open wounds clean and covered at all times until healed<br> | |||
There has also been evidence to support the use of low-frequency ultrasound on bacteria, including MRSA. According to an article posted in 2010, low-frequency ultrasound delivered at 35 kHz reduced colony forming units of bacteria and alters colonial characteristics of MRSA.<ref>Conner-Kerr T, Alston G, Stovall A, Vernon T, Winter D, Meixner J et al. The Effects of Low-frequency Ultrasound (35kHz) on Methicillin-resistant Staphylococcus aureus (MRSA) in vitro. Ostomy Wound Manage. 2010;56(5):32–42. http://www.o-wm.com/content/effects-low-frequency-ultrasound-35-khz-methicillin-resistant-staphylococcus-aureus-mrsa-vit (accessed 9 April 2016).</ref> | |||
== | === Differential Diagnosis === | ||
The differential diagnosis for MRSA includes the following infections:<ref>Staphylococcus Aureus Infection Differential Diagnoses [Internet]. Emedicine.medscape.com. 2016.&nbsp;http://emedicine.medscape.com/article/971358-differential (accessed 6 April 2016).</ref><br>• Bacteremia<br>• Chemical burns<br>• Impetigo<br>• Juvenile Idiopathic Arthritis<br>• Streptococcal Infections<br>• Kawasaki Disease<br>• Leptospirosis<br>• Parvovirus B19 Infection | |||
Further screening should be done to rule out such diseases. | |||
== | === '''Outcomes''' === | ||
* The majority of data indicate that MRSA increases mortality and morbidity in seniors, nursing home patients and those with organ dysfunction. | |||
* Individuals with end-stage liver disease, renal insufficiency and those admitted to the ICU have high mortality rates when there is an associated MRSA infection. | |||
* The mortality rates vary from 5-60%, depending on the patient population and site of infection. | |||
* More patients with MRSA are now undergoing surgery, and in at least 40% of patients, a central line was the cause of the infection. | |||
* About 60% of patients do acquire MRSA within 48 hours despite having no healthcare risks<ref name=":0" /><br> | |||
== Case Reports/ Case Studies == | |||
Hörner A, Hörner R, Salla A, Nunes M, Garzon L, Rampelotto R et al. [http://www.scielo.br/pdf/spmj/v133n5/1516-3180-spmj-2013-79400715.pdf Staphylococcal scalded skin syndrome in a premature newborn caused by methicillin-resistant Staphylococcus aureus: case report. Sao Paulo Med J. 2015;133(5):450-453].<br> | |||
Braich P, Aggarwal S, Mukhtar, BA S, Almeida D. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612473/pdf/JCHIMP-5-28769.pdf Nonsocomial Keratitis Caused by Methicillin-Resistant Staphylococcus Aureus : Case Report and Preventative Measures. Journal of Community Hospital Internal Medicine Perspectives. 2015;5(5).]<br> | |||
== References == | == References == | ||
<references /><br> | |||
<references /> | |||
[[Category: | [[Category:Medical]] | ||
[[Category:Global Health]] | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Conditions]] | |||
[[Category:Communicable Diseases]] | |||
Latest revision as of 08:43, 5 January 2022
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kory Reynolds, Sarah Tassinari, Lucinda hampton, Elaine Lonnemann, 127.0.0.1, Kim Jackson, Evan Thomas, WikiSysop and Nupur Smit Shah
Introduction[edit | edit source]
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium that causes infections in different parts of the body. It's tougher to treat than most strains of staphylococcus aureus -- or staph -- because it's resistant to some commonly used antibiotics. R image - scanning electronic microscope of MRSA and a dead neutrophil.
MRSA infection is one of the leading causes of hospital-acquired infections and is commonly associated with significant morbidity, mortality, length of stay, and cost burden. MRSA infections can be further divided into hospital-associated (HA-MRSA) infections and community-associated (CA-MRSA) infections. They differ not only in respect to their clinical features and molecular biology but also to their antibiotic susceptibility and treatment[1]
The bacteria from which MRSA arises, staphylococcus aureus, is found in the skin and in the nostrils of one third of all people whom do not show any symptoms of having been exposed to the bacteria. These carriers of the bacteria are then exposing the bacteria to all of the items that they touch as well as expelling it into the air where it will remain until the item is next cleaned.[2]
Prevention[edit | edit source]
Prevention and control of MRSA infections include necessary infection-control steps like strict hand hygiene and adequate contact precautions. Hand hygiene means washing hands with soap and water or an alcohol-based cleanser before and after contact with patients who have MRSA infection. Contact precautions include the use of gowns, gloves, and possibly masks during clinical encounters with patients with MRSA infection. Infection control also may include keeping patients in isolated rooms or the same rooms of other patients who have an MRSA[1] infection.[2]
Etiology[edit | edit source]
Methicillin resistance has occurred in S. aureus by mutation of a penicillin-binding protein, a chromosome-encoded protein. This type of resistance is transferred between S. aureus organisms by bacteriophages. This is one of the only medically relevant examples of chromosome-mediated drug resistance by phage transduction.[1]
Epidemiology[edit | edit source]
The history of MRSA infection goes back to 1961 when it was first described. Since then, the incidence and prevalence of MRSA infection have been increasing dramatically across the United States. Recently, some population studies have hinted at reducing HA-MRSA incidences in the United States but at the expense of a growing prevalence of CA-MRSA. The reported incidence of MRSA infection ranges from 7% to 60%.
Risk Factors
- The commonly associated risk factors for MRSA infection are prolonged hospitalization, intensive care admission, recent hospitalization, recent antibiotic use, MRSA colonization, invasive procedures, HIV infection, admission to nursing homes, open wounds, hemodialysis, and discharge with long-term central venous access or long-term indwelling urinary catheter.
- A higher incidence of MRSA infection is also seen among healthcare workers who come in direct contact with patients infected with this organism.
- Although advancing age by itself is not considered a risk factor for MRSA infection, age more than 65 years is a significant risk factor for hospitalization.
- Living in an area with a high prevalence of CA-MRSA or admission to a hospital with a high prevalence of HA-MRSA also is considered a significant risk factor for MRSA colonization.[1]
Pathophysiology[edit | edit source]
The key reason for MRSA resistance to beta-lactam antibiotics is due to the presence of the mecA gene sequence, which is known to generate transpeptidase PB2a that lowers the affinity of the organism to bind to beta-lactam antibiotics.[1]
Clinical Presentation[edit | edit source]
MRSA can cause a range of organ-specific infections, the most common being the skin and subcutaneous tissues, followed by invasive infections like osteomyelitis, meningitis, pneumonia, lung abscess, and empyema. Infective endocarditis caused by MRSA is associated with an increased morbidity and mortality compared to any other organism and is linked to intravenous drug abuse.
Skin and soft tissue infections (SSTI): CA-MRSA is a predominant organism associated with SSTIs like cellulitis, necrotizing fasciitis, and diabetic foot ulcers. It also is increasingly associated with more invasive disease than those due to non-MRSA. More frequently these infections are multidrug-resistant leading to frequent recurrence, increased hospitalization, and mortality.
Bone and joint infection: Staphylococci are the most common cause of bone and joint infections. MRSA can cause osteomyelitis of spine, long bones of upper and lower extremities by extension of local infection from a wound or as a part of hematogenous infection. Similarly, MRSA can cause septic arthritis of both native and prosthetic joints.
Pneumonia: Staphylococcal pneumonia - CA-MRSA can cause life-threatening necrotizing pneumonia in otherwise healthy individuals. It is characterized by severe respiratory symptoms, high fevers, hemoptysis, and hypotension. It rapidly progresses to sepsis and septic shock with leukopenia and elevated C-reactive protein. Multilobar cavitating alveolar infiltrates in a clinical setting like this is consistent with CA-MRSA infection.
MRSA is also a leading cause of hospital-acquired and ventilator-associated pneumonia.
Bacteremia: Bacteremia due to S. aureus has been reported to be associated with mortality rates of 15% to 60%. MRSA bacteremia is commonly seen in intensive care unit patients with central line insertions. Infective endocarditis is associated with MRSA bacteremia and should be ruled out in any patient with MRSA in the bloodstream. The outcomes related to MRSA bacteremia are worse than other MRSA infections because of the decreased response to vancomycin in these patients.
Endocarditis: MRSA is an important cause of bacterial endocarditis which can cause mortality in about a third of the infected patients (30-37%). Right-sided MRSA endocarditis is commonly associated with intravenous drug use and intravenous catheters. Patients with tricuspid valve vegetations may have septic pulmonary emboli causing nodular infiltrates and cavitating lesions in the lungs. Similarly, patients with involvement of mitral and aortic valves may have secondary infections in distant foci such as bones and joints, kidneys, brain, and other organs. It is important to take history and perform a thorough examination of these patients combined with necessary labs and radiological tests.[1]
Characteristics[edit | edit source]
• Chest pain
• Cough
• Shortness of breath
• Fatigue
• Fever and chills
• General ill feeling
• Headache
• Rash
• Wounds that do not heal
Differences in Characteristics Between HA-MRSA and CA-MRSA[3]
| Characteristic | HA-MRSA | CA-MRSA |
| Site of Infection | Bacteraemia, wound infections, respiratory tract, urinary tract | Mainly skin (abscesses, cellulitis, furunculosis |
| Risk Factors | Indwelling devices, catheters, lines, hemodialysis, prolonged hospitalization, long-term antibiotic use | Close physical contact, abrasion injuries, poor hygiene |
| Transmission | Person-to-person (healthcare staff, visitors, patients), environment-to-person (hospital equipment | Person-to-person (contact sports), environment-to-person (shared facilities, shared sports equipment) |
Medical Management[edit | edit source]
The selection of empiric antibiotic therapy for the treatment of MRSA infection depends on the type of disease, local S. aureus resistance patterns, availability of the drug, side effect profile, and individual patient profile.
SSTIs: For most uncomplicated SSTIs suspected of MRSA infection, empirical treatment is with oral antibiotics like trimethoprim/sulfamethoxazole, tetracyclines, such as doxycycline or minocycline, and clindamycin.
Parenteral antibiotics are indicated for invasive SSTIs or with signs of systemic involvement, inadequate response to oral therapy, or if an SSTI occurs adjacent to an indwelling device.
Intravenous vancomycin is the drug of choice for most MRSA infections seen in hospitalized patients. It can be used both as empiric and definitive therapy as most MRSA infections are susceptible to vancomycin. There are sporadic cases of vancomycin-resistant MRSA.
Daptomycin is a suitable parenteral alternative when vancomycin is not available or not being tolerated. Other short-acting options include ceftaroline and telavancin. Long-acting treatment options include dalbavancin and oritavancin. Regardless of the initial empiric antibiotic choice, subsequent therapy should be tailored based on the careful review of culture and susceptibility data.
The duration of therapy for treatment of MRSA SSTIs may range from 5 to 14 days depending on the extent of infection and response to treatment.[2]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Clinical Laboratories for MRSA, according to the Clinical and Laboratory Standards Institute (CLSI)[4]
Broth Microdultion Testing with the addition of one of the following:
- A plate containing 6 μg/ml of oxacillin in Mueller-Hinton agar supplemented with 4% NaCl as alternative methods of testing for MRSA
- Latex Agglutination Test for PBP2 - tests for the mecA gene (Staphylococcal resistance to oxacillin/methicillin happens when an altered penicillin-binding protein, PBP2a, is produced.)
- Cefoxitin Disk Screen Test
Typically the broth test and agar test are the main tests for detecting MRSA, and the cefoxitin disk screen test can be used as a back-up test.
• Detecting oxacillin/methicillin resistance can be difficult because of the presence of multiple populations (susceptible and resistant) may coexist within one culture of staphylococci.
• Oxacillin and cefoxitin are tested instead of methicillin because methicillin isn’t as readily available in the US as it once was. Oxacillin detects subpopulations well and cefoxitin activates mecA gene better, making it a more accurate test than other using oxacillin.
• Methicillin and oxacillin are in the same class of drugs. Methicillin has historically been the drug of choice for detecting resistance, hence the name MRSA. Even though the preferred drug of choice for testing has changed, the name had remained the same.
According to Centers for Disease Control and Prevention, there are additional tests to detect oxacillin/methicillin resistance but the most common and reliable tests have been listed above.
Physical Therapy Management[edit | edit source]
MRSA is not primarily managed by physical therapy. Instead it is the physical therapist’s role to identify comorbidities that are inhibiting functional activity and treat the patient’s symptoms. When treating a patient with MRSA, it’s important for the physical therapist to know proper disinfecting techniques to prevent the spread of the disease. Precautions to be taken when treating a patient with MRSA include but are not limited to:[5][6][7]
- Buy disinfectants that are registered by the Environmental Protection Agency (EPA)
- Note how to properly apply each product, how long it needs to be left on the surface, if the surface needs to be rinsed prior, if it’s only for specific surfaces, etc.
- Laundering specific clothes, towels and linens separately would be appropriate but not always necessary – wash and dry in the warmest temperate recommended on each piece of linen individually
- All surfaces ad equipment that came in contact with the patient should be cleaned, sometimes individual equipment for the patient with MRSA may be necessary if equipment cannot be properly cleaned
- Use barriers between the patient’s skin and surface when possible
- Physical therapist should wash body parts immediately after making contact with patient’s skin
- Patient should keep all open wounds clean and covered at all times until healed
There has also been evidence to support the use of low-frequency ultrasound on bacteria, including MRSA. According to an article posted in 2010, low-frequency ultrasound delivered at 35 kHz reduced colony forming units of bacteria and alters colonial characteristics of MRSA.[8]
Differential Diagnosis[edit | edit source]
The differential diagnosis for MRSA includes the following infections:[9]
• Bacteremia
• Chemical burns
• Impetigo
• Juvenile Idiopathic Arthritis
• Streptococcal Infections
• Kawasaki Disease
• Leptospirosis
• Parvovirus B19 Infection
Further screening should be done to rule out such diseases.
Outcomes[edit | edit source]
- The majority of data indicate that MRSA increases mortality and morbidity in seniors, nursing home patients and those with organ dysfunction.
- Individuals with end-stage liver disease, renal insufficiency and those admitted to the ICU have high mortality rates when there is an associated MRSA infection.
- The mortality rates vary from 5-60%, depending on the patient population and site of infection.
- More patients with MRSA are now undergoing surgery, and in at least 40% of patients, a central line was the cause of the infection.
- About 60% of patients do acquire MRSA within 48 hours despite having no healthcare risks[1]
Case Reports/ Case Studies[edit | edit source]
Hörner A, Hörner R, Salla A, Nunes M, Garzon L, Rampelotto R et al. Staphylococcal scalded skin syndrome in a premature newborn caused by methicillin-resistant Staphylococcus aureus: case report. Sao Paulo Med J. 2015;133(5):450-453.
Braich P, Aggarwal S, Mukhtar, BA S, Almeida D. Nonsocomial Keratitis Caused by Methicillin-Resistant Staphylococcus Aureus : Case Report and Preventative Measures. Journal of Community Hospital Internal Medicine Perspectives. 2015;5(5).
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Siddiqui AH, Koirala J. Methicillin resistant Staphylococcus aureus (MRSA). Available from:https://www.ncbi.nlm.nih.gov/books/NBK482221/ (last accessed 7.3.2020)
- ↑ 2.0 2.1 2.2 Robinson J, Edgley A, Morrell J. MRSA care in the community: why patient education matters. British Journal of Community Nursing. 2014;19(9):436-441. http://dx.doi.org.libproxy.bellarmine.edu/10.12968/bjcn.2014.19.9.436 (accessed 2 April 2016).
- ↑ Millar B, Loughrey A, Elborn J, Moore J. Proposed definitions of community-associated meticillin-resistant Staphylococcus aureus (CA-MRSA). Journal of Hospital Infection. 2007;67(2):109-113. http://eds.b.ebscohost.com.libproxy.bellarmine.edu/ehost/detail/detail?vid=14&sid=71ee6b7e-199d-4adc-8e31-bc94eca59a09%40sessionmgr113&hid=112&bdata=JmxvZ2luLmFzcCZzaXRlPWVob3N0LWxpdmUmc2NvcGU9c2l0ZQ%3d%3d#AN=105828672&db=cin20 (accessed 2 April 2016).
- ↑ Centers for Disease Control and Prevention. Laboratory Testing for MRSA. http://www.cdc.gov/mrsa/lab/ (accessed 8 April 2016).
- ↑ Centers for Disease Control and Prevention. Cleaning & Disinfecting Athlete Facilities. http://www.cdc.gov/mrsa/community/environment/athletic-facilities.html (accessed 8 April 2016).
- ↑ Centers for Disease Control and Prevention. Laundry. http://www.cdc.gov/mrsa/community/environment/laundry.html (accessed 8 April 2016).
- ↑ MedlinePlus Medical Encyclopedia. MRSA. https://www.nlm.nih.gov/medlineplus/ency/article/007261.htm (accessed 7 April 2016).
- ↑ Conner-Kerr T, Alston G, Stovall A, Vernon T, Winter D, Meixner J et al. The Effects of Low-frequency Ultrasound (35kHz) on Methicillin-resistant Staphylococcus aureus (MRSA) in vitro. Ostomy Wound Manage. 2010;56(5):32–42. http://www.o-wm.com/content/effects-low-frequency-ultrasound-35-khz-methicillin-resistant-staphylococcus-aureus-mrsa-vit (accessed 9 April 2016).
- ↑ Staphylococcus Aureus Infection Differential Diagnoses [Internet]. Emedicine.medscape.com. 2016. http://emedicine.medscape.com/article/971358-differential (accessed 6 April 2016).