Hemorrhagic Stroke: Intracerebral Hemorrhage: Difference between revisions
No edit summary |
(text, sections, images, refs) |
||
| Line 9: | Line 9: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File:Stroke | [[File:Stroke hemorrhagic.jpg|right|frameless|475x475px]] | ||
15% of acute strokes are hemorrhagic strokes which are caused by | |||
Intracerebral hemorrhage (ICH) is the most disabling and deadly form of stroke. | |||
15% of acute strokes are hemorrhagic strokes which are caused by an acute hemorrhage. There are two main types of hemorrhagic strokes 1. intracerebral hemorrhage (ICH) and 2. subarachnoid hemorrhage which accounts for about 5% of all strokes. This page relates to ICH ie bleeding within the brain tissue itself — a life-threatening type of stroke which deprives the brain of oxygen and blood supply<ref>Tadi P, Lui F. [https://www.ncbi.nlm.nih.gov/books/NBK535369/ Acute Stroke (Cerebrovascular Accident)]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535369/ (last accessed 31.12.2019)</ref>. | |||
* Intracerebral hemorrhage (ICH) is a devastating event, carrying a very high morbidity and mortality rate that have not changed over the last 30 years. | * Intracerebral hemorrhage (ICH) is a devastating event, carrying a very high morbidity and mortality rate that have not changed over the last 30 years. | ||
* Hypertension and age-related amyloid angiopathy are the strongest risk factors for ICH, but smoking, anticoagulation with warfarin, excessive alcohol intake and cocaine also increase risk.<ref name=":0">Rymer MM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188453/ Hemorrhagic stroke: intracerebral hemorrhage]. Missouri medicine. 2011 Jan;108(1):50.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188453/ (last accessed 31.12.2019)</ref> | * Hypertension and age-related amyloid angiopathy are the strongest risk factors for ICH, but smoking, anticoagulation with warfarin, excessive alcohol intake and cocaine also increase risk.<ref name=":0">Rymer MM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188453/ Hemorrhagic stroke: intracerebral hemorrhage]. Missouri medicine. 2011 Jan;108(1):50.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188453/ (last accessed 31.12.2019)</ref> | ||
| Line 20: | Line 23: | ||
ICH are almost invariably associated with hypertension and are presumed by many to be the result of weakening of arterial walls by the trauma of an excessive pulse pressure. The most common sites of involvement are: | ICH are almost invariably associated with hypertension and are presumed by many to be the result of weakening of arterial walls by the trauma of an excessive pulse pressure. The most common sites of involvement are: | ||
(1) the region of the putamen-external capsule in the distribution of the lenticulostriate branches of the middle cerebral artery (50%) | (1) the region of the putamen-external capsule in the distribution of the lenticulostriate branches of the middle cerebral artery (50%) . The putamen (a common site for hypertensive bleed) is involved in learning and motor control, including speech articulation, and language functions, reward, cognitive functioning, and addiction.<ref>Ghandili M, Munakomi S. [[Neuroanatomy, Putamen.]] InStatPearls [Internet] 2019 May 30. StatPearls Publishing.Available from: https://www.ncbi.nlm.nih.gov/books/NBK542170/ (last accessed 1.1.2020)</ref> | ||
(2) the thalamus in the distribution of the small penetrating vessels from the posterior cerebral and posterior communicating arteries (10%); | (2) the thalamus in the distribution of the small penetrating vessels from the posterior cerebral and posterior communicating arteries (10%); | ||
| Line 32: | Line 35: | ||
== Mechanism of Injury / Pathological Process == | == Mechanism of Injury / Pathological Process == | ||
* Hypertensive vascular change - ICH is usually caused by ruptured vessels that are degenerated due to long-standing hypertension the arteries showing prominent degeneration of the media and smooth muscles. Less frequently fibrinoid necrosis of the sub-endothelium with micro-aneurysms and focal dilatations may occur. | * Hypertensive vascular change - ICH is usually caused by ruptured vessels that are degenerated due to long-standing hypertension the arteries showing prominent degeneration of the media and smooth muscles. Less frequently fibrinoid necrosis of the sub-endothelium with micro-aneurysms and focal dilatations may occur. | ||
* Cerebral amyloid angiopathy - CAA is characterized by the deposition of amyloid-β peptide at capillaries, arterioles, and small- and medium-sized arteries in the cerebral cortex, leptomeninges, and cerebellum . CAA in the cerebral small vessel leads to sporadic ICH in elderly people, commonly associated with variations in the gene encoding apolipoprotein E epsilon 2 and 4 in chromosome 19 . Duplication of the APP locus on chromosome 21 is also found in families with familial early-onset Alzheimer disease and CAA. CAA-related ICHs occur mainly in the elderly subjects while a rare familial syndrome may manifest in relatively young patients | * Cerebral amyloid angiopathy - CAA is characterized by the deposition of amyloid-β peptide at capillaries, arterioles, and small- and medium-sized arteries in the cerebral cortex, leptomeninges, and cerebellum . CAA in the cerebral small vessel leads to sporadic ICH in elderly people, commonly associated with variations in the gene encoding apolipoprotein E epsilon 2 and 4 in chromosome 19 . Duplication of the APP locus on chromosome 21 is also found in families with familial early-onset Alzheimer disease and CAA. CAA-related ICHs occur mainly in the elderly subjects while a rare familial syndrome may manifest in relatively young patients.<ref name=":2">An SJ, Kim TJ, Yoon BW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5307940/ Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update]. Journal of stroke. 2017 Jan;19(1):3. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5307940/ (last accessed 31.12.2019)</ref> | ||
* The mass effect of the primary bleeding may cause lesions to migrate and dissect through less-dense white matter and into the ventricles resulting in increased intracranial pressure. A hematoma incites local edema and neuronal damage in the adjacent brain parenchyma which typically lasts from 5 days to 2 weeks, with the largest increase in edema occurring in the first 72 hours. Thrombin within the hematoma plays a central role in promoting perihematomal edema. Hemoglobin and its products, heme and iron, are potent mitochondrial toxins leading to cell death.<ref name=":0" /> | |||
In aging individuals, and especially in those with Alzheimer's Disease, amyloid deposition may occur in the penetrating cortical vessels, making the vessels more friable and subject to hemorrhage. Typically, the hemorrhage is lobar (i.e., immediately subcortical) and the likelihood that amyloid angiopathy is the etiology of the hemorrhage is increased if there is no past history of hypertension.<ref name=":1" /> | In aging individuals, and especially in those with Alzheimer's Disease, amyloid deposition may occur in the penetrating cortical vessels, making the vessels more friable and subject to hemorrhage. Typically, the hemorrhage is lobar (i.e., immediately subcortical) and the likelihood that amyloid angiopathy is the etiology of the hemorrhage is increased if there is no past history of hypertension.<ref name=":1" /> | ||
| Line 78: | Line 81: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Sudden onset of focal neurological deficit which progresses over minutes to hours is the major presenting feature of ICH. The nature of the deficits reflects the location of the initial bleeding and subsequent edema. | |||
Common associated features include - Seizures, vomiting, headache, and diminished level of consciousness. NB. Both headache and diminished level of conscious are ''uncommon'' in acute ischemic strokes<ref name=":0" />. | |||
The majority of patients with primary ICH develop measurable lesion expansion over the initial few hours. The degree of hematoma growth is an independent determinant of mortality and functional outcome.<ref name=":0" /><br> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
The early risk of neurological deterioration and cardiopulmonary instability in ICH is high, making urgent diagnosis and management critical. | |||
* History is critical as it is important to know whether there is any history of trauma, hypertension, excessive use of alcohol, any use of drugs either by prescription or recreation that could play a role eg cocaine, warfarin, aspirin, clopidogrel, or any hematologic disorder. | |||
* Physical examination - priority is to assess vital signs and determine if intubation is required for safety during imaging. | |||
* It is important to determine if acute myocardial injury is a risk in patients with severely elevated blood pressure (BP) | |||
# [[CT Scans|CT]] head scanning is the major test in use to differentiate between acute ICH, SAH (subarachnoid haemorrhage), and ischemic stroke. It is an extremely sensitive test to detect both ICH and SAH and to identify the size and location of the hemorrhage. Hematoma expansion, highly associated with clinical deterioration and poor outcomes, is evident in nearly 40% of cases within the first 3 hours after onset of symptoms is also well-documented with CT scanning<ref name=":0" /> | |||
# CT with contrast and CT angiography (CTA) may identify associated aneurysms, tumors and underlying AVMs | |||
# [[MRI Scans|MR]] scanning is more sensitive for AVMs | |||
# Digital subtraction angiography (DSA) is the gold standard for identification of aneurysms and AVMs. | |||
== Prognosis == | |||
Known poor prognostic factors of ICH include <ref name=":2" /> | |||
# large hematoma volume, | |||
# hematoma expansion, | |||
# intraventricular hemorrhage, | |||
# infra-tentorial location, | |||
# old age, | |||
# contrast extravasation on CT scan (spot sign) | |||
# use of anticoagulation. | |||
* The volume of the ICH and the clinical grade on the Glasgow Coma Scale on admission are the most powerful predictors of 30-day mortality. | |||
* Hemispheric lesions >30 cc have a high mortality rate. | |||
* Patients with GCS <9 and hematoma >60 cc have a 90% mortality rate. | |||
* Intraventricular involvement with associated hydrocephalus predicts a mortality rate of 43% at 30 days. | |||
* Brainstem hemorrhages, even when small, carry a poor prognosis. Age over 80 years also carries a higher risk of mortality.<ref name=":0" /> | |||
== Management | == Management == | ||
see [[Stroke Medical Management]] | |||
== | == Physiotherapy Assessment and Treatment Approaches == | ||
see [[Stroke: Assessment]] and [[Stroke: Physiotherapy Treatment Approaches]] | |||
== | == Recovery == | ||
Early mobilization and involvement of the neuro-rehabilitation team is essential to maximizing recovery. People with severe ICH have the potential to do better than those with severe ischemic stroke. | |||
== References == | == References == | ||
Revision as of 07:38, 1 January 2020
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (1/01/2020)
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Introduction[edit | edit source]
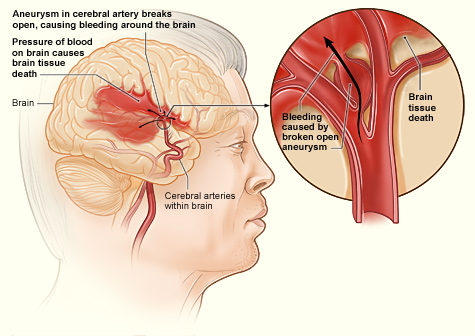
Intracerebral hemorrhage (ICH) is the most disabling and deadly form of stroke.
15% of acute strokes are hemorrhagic strokes which are caused by an acute hemorrhage. There are two main types of hemorrhagic strokes 1. intracerebral hemorrhage (ICH) and 2. subarachnoid hemorrhage which accounts for about 5% of all strokes. This page relates to ICH ie bleeding within the brain tissue itself — a life-threatening type of stroke which deprives the brain of oxygen and blood supply[1].
- Intracerebral hemorrhage (ICH) is a devastating event, carrying a very high morbidity and mortality rate that have not changed over the last 30 years.
- Hypertension and age-related amyloid angiopathy are the strongest risk factors for ICH, but smoking, anticoagulation with warfarin, excessive alcohol intake and cocaine also increase risk.[2]
- At one year, mortality ranges from 51% to 65% depending on the location of the hemorrhage. Half of these deaths occur in the first two days and at six months, only 20% of patients are expected to be independent.
- The incidence of hemorrhage increases exponentially with age and is higher in men than in women[2].
Clinically Relevant Anatomy[edit | edit source]
ICH are almost invariably associated with hypertension and are presumed by many to be the result of weakening of arterial walls by the trauma of an excessive pulse pressure. The most common sites of involvement are:
(1) the region of the putamen-external capsule in the distribution of the lenticulostriate branches of the middle cerebral artery (50%) . The putamen (a common site for hypertensive bleed) is involved in learning and motor control, including speech articulation, and language functions, reward, cognitive functioning, and addiction.[3]
(2) the thalamus in the distribution of the small penetrating vessels from the posterior cerebral and posterior communicating arteries (10%);
(3) the cerebellum in the distribution of the deep penetrating branches of the superior cerebellar artery (10%); and
(4) the pons in the distribution of the paramedian branches of the basilar artery (10%).
The remaining 20% occur into the white matter of various lobes of the cerebral hemispheres.[4]
Mechanism of Injury / Pathological Process[edit | edit source]
- Hypertensive vascular change - ICH is usually caused by ruptured vessels that are degenerated due to long-standing hypertension the arteries showing prominent degeneration of the media and smooth muscles. Less frequently fibrinoid necrosis of the sub-endothelium with micro-aneurysms and focal dilatations may occur.
- Cerebral amyloid angiopathy - CAA is characterized by the deposition of amyloid-β peptide at capillaries, arterioles, and small- and medium-sized arteries in the cerebral cortex, leptomeninges, and cerebellum . CAA in the cerebral small vessel leads to sporadic ICH in elderly people, commonly associated with variations in the gene encoding apolipoprotein E epsilon 2 and 4 in chromosome 19 . Duplication of the APP locus on chromosome 21 is also found in families with familial early-onset Alzheimer disease and CAA. CAA-related ICHs occur mainly in the elderly subjects while a rare familial syndrome may manifest in relatively young patients.[5]
- The mass effect of the primary bleeding may cause lesions to migrate and dissect through less-dense white matter and into the ventricles resulting in increased intracranial pressure. A hematoma incites local edema and neuronal damage in the adjacent brain parenchyma which typically lasts from 5 days to 2 weeks, with the largest increase in edema occurring in the first 72 hours. Thrombin within the hematoma plays a central role in promoting perihematomal edema. Hemoglobin and its products, heme and iron, are potent mitochondrial toxins leading to cell death.[2]
In aging individuals, and especially in those with Alzheimer's Disease, amyloid deposition may occur in the penetrating cortical vessels, making the vessels more friable and subject to hemorrhage. Typically, the hemorrhage is lobar (i.e., immediately subcortical) and the likelihood that amyloid angiopathy is the etiology of the hemorrhage is increased if there is no past history of hypertension.[4]
Risk Factors[edit | edit source]
Risk factors of intracerebral hemorrhage[5]
| Modifiable risk factors |
| Hypertension |
| Current smoking |
| Excessive alcohol consumption |
| Decreased Low-density lipoprotein cholesterol, low triglycerides |
| Anticoagulation |
| Use the antiplatelet agent |
| Sympathomimetic drugs (Cocaine, heroin, amphetamine, PPA and ephedrine) |
| Non-modifiable risk factor |
| Old age |
| Male sex |
| Asian ethnicity |
| Cerebral amyloid angiopathy |
| Cerebral microbleeds |
| Chronic kidney disease |
| Other factors suggested to be related the risk |
| Multi-parity |
| Poor working conditions (blue-collar occupation, longer working time) |
Clinical Presentation[edit | edit source]
Sudden onset of focal neurological deficit which progresses over minutes to hours is the major presenting feature of ICH. The nature of the deficits reflects the location of the initial bleeding and subsequent edema.
Common associated features include - Seizures, vomiting, headache, and diminished level of consciousness. NB. Both headache and diminished level of conscious are uncommon in acute ischemic strokes[2].
The majority of patients with primary ICH develop measurable lesion expansion over the initial few hours. The degree of hematoma growth is an independent determinant of mortality and functional outcome.[2]
Diagnostic Procedures[edit | edit source]
The early risk of neurological deterioration and cardiopulmonary instability in ICH is high, making urgent diagnosis and management critical.
- History is critical as it is important to know whether there is any history of trauma, hypertension, excessive use of alcohol, any use of drugs either by prescription or recreation that could play a role eg cocaine, warfarin, aspirin, clopidogrel, or any hematologic disorder.
- Physical examination - priority is to assess vital signs and determine if intubation is required for safety during imaging.
- It is important to determine if acute myocardial injury is a risk in patients with severely elevated blood pressure (BP)
- CT head scanning is the major test in use to differentiate between acute ICH, SAH (subarachnoid haemorrhage), and ischemic stroke. It is an extremely sensitive test to detect both ICH and SAH and to identify the size and location of the hemorrhage. Hematoma expansion, highly associated with clinical deterioration and poor outcomes, is evident in nearly 40% of cases within the first 3 hours after onset of symptoms is also well-documented with CT scanning[2]
- CT with contrast and CT angiography (CTA) may identify associated aneurysms, tumors and underlying AVMs
- MR scanning is more sensitive for AVMs
- Digital subtraction angiography (DSA) is the gold standard for identification of aneurysms and AVMs.
Prognosis[edit | edit source]
Known poor prognostic factors of ICH include [5]
- large hematoma volume,
- hematoma expansion,
- intraventricular hemorrhage,
- infra-tentorial location,
- old age,
- contrast extravasation on CT scan (spot sign)
- use of anticoagulation.
- The volume of the ICH and the clinical grade on the Glasgow Coma Scale on admission are the most powerful predictors of 30-day mortality.
- Hemispheric lesions >30 cc have a high mortality rate.
- Patients with GCS <9 and hematoma >60 cc have a 90% mortality rate.
- Intraventricular involvement with associated hydrocephalus predicts a mortality rate of 43% at 30 days.
- Brainstem hemorrhages, even when small, carry a poor prognosis. Age over 80 years also carries a higher risk of mortality.[2]
Management[edit | edit source]
Physiotherapy Assessment and Treatment Approaches[edit | edit source]
see Stroke: Assessment and Stroke: Physiotherapy Treatment Approaches
Recovery[edit | edit source]
Early mobilization and involvement of the neuro-rehabilitation team is essential to maximizing recovery. People with severe ICH have the potential to do better than those with severe ischemic stroke.
References[edit | edit source]
- ↑ Tadi P, Lui F. Acute Stroke (Cerebrovascular Accident). Available from: https://www.ncbi.nlm.nih.gov/books/NBK535369/ (last accessed 31.12.2019)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Rymer MM. Hemorrhagic stroke: intracerebral hemorrhage. Missouri medicine. 2011 Jan;108(1):50.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6188453/ (last accessed 31.12.2019)
- ↑ Ghandili M, Munakomi S. Neuroanatomy, Putamen. InStatPearls [Internet] 2019 May 30. StatPearls Publishing.Available from: https://www.ncbi.nlm.nih.gov/books/NBK542170/ (last accessed 1.1.2020)
- ↑ 4.0 4.1 DISORDERS OF THE NERVOUS SYSTEM - REEVES & SWENSON Chapter 27. Cerebrovascular disorders Available from:https://www.dartmouth.edu/~dons/part_3/chapter_27.html#chpt_27_ICH (last accessed 31.12.2019)
- ↑ 5.0 5.1 5.2 An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. Journal of stroke. 2017 Jan;19(1):3. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5307940/ (last accessed 31.12.2019)