Communication in Healthcare
Introduction[edit | edit source]
Ineffective Communication[edit | edit source]
Mental Health[edit | edit source]
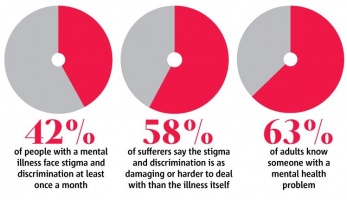
Providing treatment and care for patients suffering from mental disorders is emotionally demanding and requires a high level of communication [10]. Aggression, confusion, and suicidal and self-harming behaviours are common symptoms of mental illness which AHP’s have reported as challenging to communicate about with patients [5] [6] [11]. A study investigating the management of patients with mental health disorders found that a healthcare provider's perception of a patient as a possible ‘time waster’ affected the quality of care that the patient received [9]. A study on the challenges of treating mental health co-morbidities in acute settings found that even if a practitioner was formally educated on mental illness, they were not immune to feelings of negative stigma towards patients [5]. The inability of healthcare providers to empathise with patients, especially with those having self-harming behaviours, was another major barrier to effective communication [7] [11]. Strensrud, Mjaaland and Finset analysed questionnaires sent to GP’s to rate their confidence in communicating with patients suffering from severe mental illness[12]. It was found that empathy was scored very low on self-appraisal and very high in areas which they believed specific training was necessary [12]. Time constraints, lack of knowledge about mental illness and frustration were also found to contribute to ineffective communication between patient and healthcare provider [5] [9] [11]. A study investigating the management of patients with mental health disorders found a consensus from the AHP’s that their needs to be formal training in communicating with patients who have mental health disorders in order to help healthcare staff provide better care for their specific needs [8]. In summary, the negative stigma associated with mental illness appears to be a major barrier to effective communication and treatment for this population.
Obesity [edit | edit source]
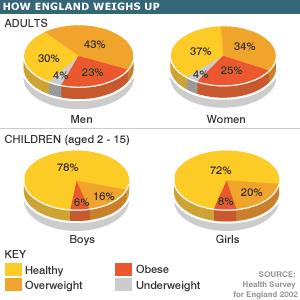
The World Health Organization reports that in 2008, over 1.4 billion adults over the age of 20 were considered overweight or obese [13]. The various comorbidities associated with obesity such as type 2 diabetes, cardiovascular disease, osteoarthritis and certain
types of cancer, suggest that AHPs will encounter obese patients in a variety of settings [14] [13]. There is a recognized need to discuss obesity with patients to promote health and well being, however, many AHPs are often uncomfortable communicating the need for weight loss to their patients [15] [16]. General practitioners (GP) are often in the front line of patient contact, however, only 42% of overweight patients are advised by their GP to lose weight [15]. Therefore, more than half of the patients that would benefit from a weight loss conversation do not get the assistance they need from their healthcare provider.
Effective communication between AHPs and patients is essential and can influence the effectiveness of any conversations regarding weight loss [16]. A focus group of physicians identified negative stigma and insufficient knowledge as major barriers to initiating the weight loss conversation, as well as frustration, lack of counselling skill and time constraints [15]. Negative stigma, also referred to in this context as weight stigma, exists between AHPs and obese patients with the perception that they are unable or unwilling to change their behaviours because they do not possess self-control [17][18]. Furthermore, many AHPs believed that managing obesity was the responsibility of the patient and was not necessary to have medical intervention [19]. This perception predisposes the AHP to be less active in the provision of weight-loss conversations as well as in counselling the patient on how to change their behaviours [19]. AHPs with insufficient knowledge about weight loss methods or techniques feel uncomfortable approaching the conversation and tend to avoid it completely [18]. In this case, AHP's may advise the patient that they may want to consider losing weight and give them pamphlets on obesity, however the conversation often never takes place [18]. The AHPs own perceptions of their weight will influence their willingness to part-take in a weight loss conversation [20]. A survey of 500 physicians found that those with a BMI between 20-25, what is considered normal, were more likely to initiate a weight loss conversation [20]. Finally, patients and AHPs often believe that the current weight issue occur from different causes and this can be a source of frustration when trying to initiate behavioural changes [18].
End of Life[edit | edit source]
Discussions regarding death and terminal illness are a difficult challenge for patients, family members and AHPs. As AHPs often try to protect their patients from bad news, end of life discussions are often avoided [21]. Fallowfield illustrated the fact that health professionals often argue that patients hearing the reality of their illness are at risk of losing hope, becoming depressed and not making the most of their remaining time[21]. However, it was also found that patients with anxiety and depression due to their terminal illness have been inadequately informed about their condition in primary care [22]. Therefore, it is evident that conversations about terminal illnesses should not be avoided to improve patient anxiety and acceptance regarding their condition.
A lack of knowledge and skill in relaying information about terminal illness and death is a major barrier to effective communication between AHPs and terminal patients [23]. Student AHPs reported that discussing issues regarding terminal illness with patients to be difficult and uncomfortable, stating they lacked the appropriate communication training [24]. The study examined students with formal training in communicating terminal illness and found these students were more confident in addressing these sensitive issues [24]. Therefore, education can positively influence an AHPs self-efficacy with regards to initiating conversations with patients about their terminal illness. The health professional being sensitive to the appropriate time to open a discussion regarding this sensitive topic is also a crucial skill when dealing with those with terminal illnesses [25]. A second barrier is an AHP’s discomfort with discussing death to a patient or their family members [26]. According to an interview conducted by Curtis and Patrick, one physician identified this barrier as, “an elephant in the room that you do not want to talk about”[26]. Whether it is AHP discomfort or attempts to protect the patient, ambiguous statements regarding terminal illness can result in negative psychological consequences [21]. Therefore, AHPs should strive to fully inform patients about their condition and prognosis, to allow the patient and their families to cope with and accept their situation[21].
Sexual Activity[edit | edit source]
Sexuality and intimacy are components of patients lives which are often avoided, overlooked and under-treated when rehabilitating patients.[27]Sex is a topic of conversation which is commonly avoided both by health professionals and patients as many people are not comfortable discussing sexual issues openly. When this topic arises in a health care setting, both health care professionals and patients can find the topic an embarrassing and difficult one to discuss.[27] Orthopaedic, respiratory, surgical, oncology and general practice are a few of the healthcare areas in which the patient may raise concerns about sexuality.[28] Although there is a need for a conversation between patients and professionals regarding sexuality and intimacy in variety of areas, many AHP's and patients are still uncomfortable discussing the topic. [27] A survey of 170 patients who attended a GP appointment found that 35% of the males and 42% of the females had some form of sexual dysfunction.[29] However, only 2% of the GP notes recorded that a discussion about sexuality had taken place even though 70% of the patients perceived that the GP was the person with whom they should discuss their sexual health.[29]
The barriers to communicating about sexual health between patients and professionals have been found to be lack of time, embarrassment and lack of knowledge.[30] Time constraints is the most commonly reported barrier to communication about sexual health.[29][27] AHPs have referred to the conversation as 'opening a can of worms' and state that once the conversation has started you have to see it all the way through no matter how limited your time or resources.[29] The fact that sexual health takes specialist knowledge has also resulted in some AHPs feeling ill-prepared to address patient concerns.[27] Studies have shown that health professionals’ skills and attitudes are addressed during professional education and training courses, however dedicated courses are usually poorly attended.[30] Although dedicated courses exist to address these barriers, many AHPs report that they would rather not ask about sexual health unless the patient raises any concerns.[30] However, this may be problematic as a study by the Association of Reproductive Health Professionals found that 68% of patients did not approach the topic of sex with health professionals for fear of being embarassed.[31] Participants have also reported being surprised when sexual activity was mentioned as they had not previously considered it as a problematic physical activity.[28] This supports the need for health professionals to initiate a conversation regarding sexual health.
Violence and Aggressive Behaviour[edit | edit source]
The traumatic nature of situations in which healthcare professionals often become involved may cause interactions with patients and their loved ones to become fraught with tension [32]. It is common in these situations for frustration, anxiety, uncertainty and helplessness to escalate into more aggressive and dangerous behaviours [32]; [33]. Research suggests that verbal and physical violence in healthcare settings has not only become common, but has become an accepted part of certain healthcare professions, particularly for emergency department (ED) nurses [34]. While a probable explanation for this phenomenon is that ED staff deal with the most urgent and serious medical incidents, it has been shown that they are not isolated in their exposure to violent and aggressive behaviours (VAB) [34]. One study [35] found that 22% of radiographers, 19% of doctors, 10% of occupational therapists and 17% of physiotherapists had been assaulted within the last year. Although the UK government has introduced a zero tolerance policy towards VAB in all NHS settings, the incidence has only increased[36]. Therefore, there is a need for all AHPs to acquire the skills to de-escalate and cope with violent and aggressive patients and their family members.
Hahn et al. (2012) reported that VAB was often managed by AHPs through either urging the person to stop their behaviour or by leaving the scene[37]. These approaches are in accordance with zero tolerance policy, but have been demonstrated to be ineffective in combating VAB[37]. Communication using de-escalation strategies were found to be much more effective in coping with patients who are becoming aggressive [37]. However, barriers such as fear, frustration, empathy and lack of skill or knowledge prevent AHPs from communicating with disgruntled patients[32]; [33]. A survey of 64 AHP students found that more than half were involved in an incident of VAB, with 94% stating they did not feel adequately prepared to handle such a situation[38]. Empathy is a barrier to communication often overlooked when dealing with violent or aggressive patients [32]. Although some factors leading to aggressive behaviours are within the patients control, such as alcohol consumption, many environmental factors can cause anxiety, helplessness and frustration which can make the patient more prone to aggression[32]. Therefore, professionals dealing with aggressive patients must be sensitive and empathetic to any environmental factors. ED nurses with greater than ten years experience are most prone to being the recipient of patient aggression[37]. It is theorised that becoming accustomed to their daily routine has made ED nurses less sensitive and empathetic to specific patient needs and contributing to the environmental factors causing patient aggression[37].
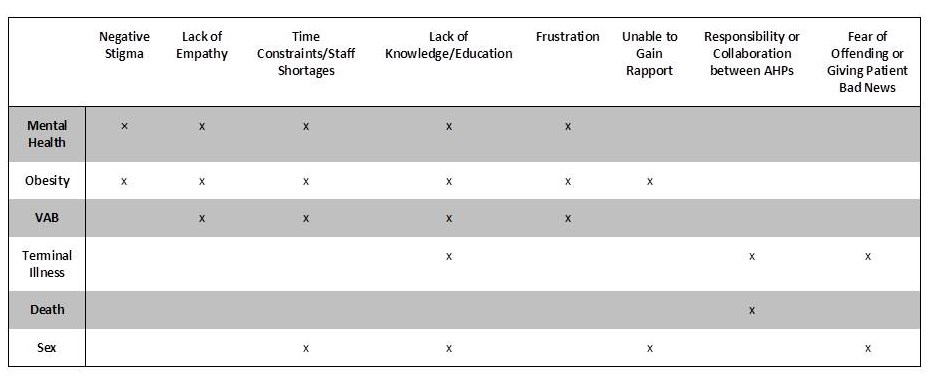
Emerging themes: Common Issues in Communication[edit | edit source]
Effective Communication: Strategies and Techniques[edit | edit source]
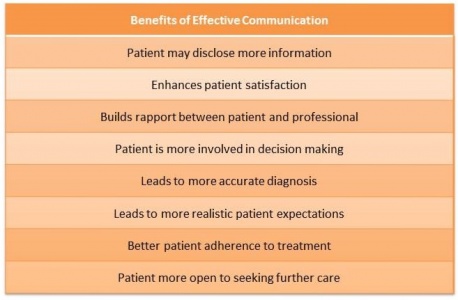
It is commonly thought that physician- patient communication within the NHS has been generally adequate and of no cause for concern. In recent years however, the number of NHS complaints have risen to a staggering 174,872 between 2013/2014 [39]. The onus of these complaints has been predominantly put on the breakdowns in communication and lack of satisfactory bedside manner of healthcare professionals. Physicians have often been criticised as being ‘cold’ or having a lack of empathy. This can stem from a number of reasons including first contact with the patient, lack of discussion of patient problems, lack of communication skills on part of the physician and/or the patient, or the general lack of patient involvement in the provision of care [40] Research has proven that effective physician – patient communication not only improves emotional health of patients but also aids in symptom resolution, functional and physiological status and pain control [40]. With these substantial influences on patient health outcomes, the importance of effective communication is further highlighted.
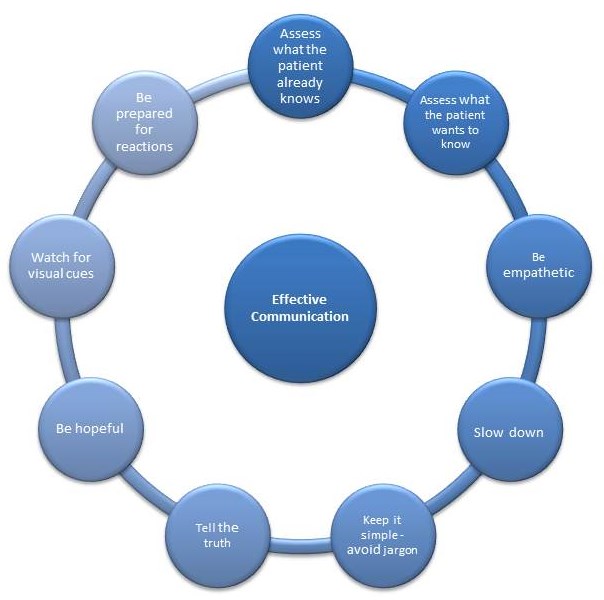
Techniques to Effective Communication[edit | edit source]
Barriers[edit | edit source]
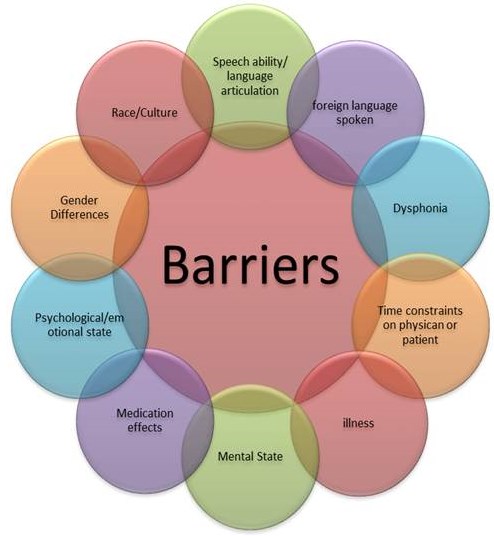
The choices of questions, words, silences, tones and facial expressions used by the clinician can greatly influence their relationship with a patient. The misuse of these interpersonal and communicative skills can become barriers not only to physician-patient relationship but also to the effectiveness of the treatment.The image below represents a number of barriers which may be experienced.
Motivational Interviewing [edit | edit source]
Motivational interviewing (MI) is a cognitive-behavioural technique, which aims to help patients identify and change behaviours that may be putting them at risk of developing health problems or may be hindering the management of an ongoing condition [44]. MI is to understand the patients perspective, accepting their motivation, or lack of motivation for changing and helping them find solutions to change [45].
MI has 5 basic principles that should be undertaken to carry out change. These are:
- Expressing empathy – by demonstrating empathy, a real and understanding picture is conveyed of what the person is going through. It shows that you are interested, accepting and understanding to the patient.
- Avoiding argument – Arguments are unproductive and need to be avoided, and resistance to change can be increased as a consequence of arguments
- Supporting self-efficacy – Believing in ones ability to change
- Developing discrepancy – The patient needs to have goals to work towards. These goals shouldn’t be forced on the patient, they should come up with them themselves
- Rolling with resistance – a skilful technique that can help change a persons’ perspective. Ideas should be offered, but not imposed, and statements can be lightly challenged but not argued [44].
Some examples of these can include praising an obese patient that has lost weight or by asking a patient what they can achieve, or what they’d like to achieve from their overall goal [45].
There are several steps of MI that allow the process to work, which includes:
- Establishing rapport – this is the basis of trust, an essential element to implement change in someone
- Setting the agenda – realistic targets set as chosen, not imposed upon, the patient. Stops them from attempting too much too soon. These change of programmes should be re-visited regularly.
- Assess readiness to change – Assessing their eagerness to change, will give an insight into their level of motivation.
- Readjust the focus – Identifies exactly what the patient wants help with, or what exactly they want to change
- Identify uncertainty - Can help identify areas for and against change
- Encourage self-motivation – By implementing a positive attitude in the patient, and encourage them to highlight success.[44]
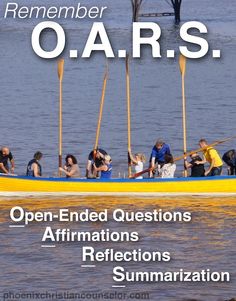
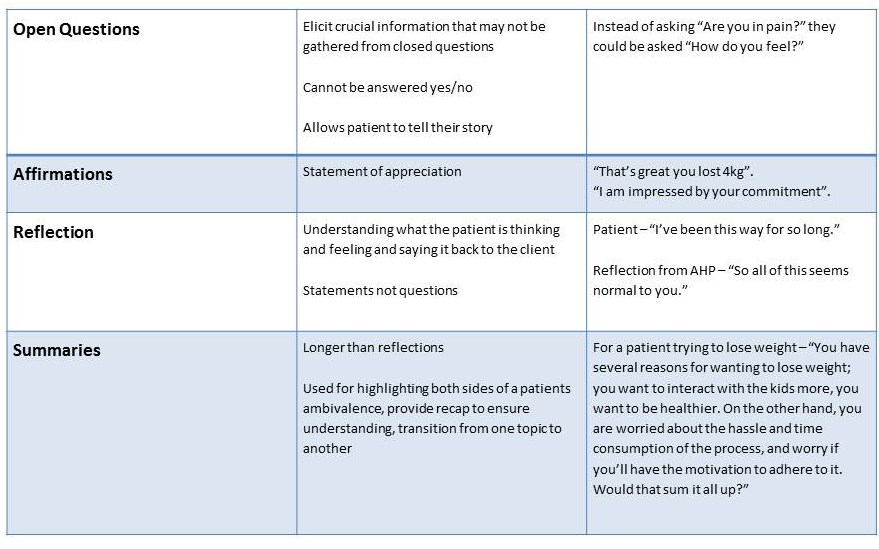
OARS,an acronym used for open-ended questions, affirmations, reflective listening and summaries are crucial components of effective communication, and equally important in MI. It has been shown to increase the patient-AHP bond and increase patient adherence, collaboration and satisfaction.[46]OARS includes many of the skills and principles outlines above and a good summary can be found in the table below.
Barriers this tool meets:
- Negative stigma
- Lack of empathy
- Unable to gain rapport
SPIKES[edit | edit source]
The delivery of bad news is a difficult challenge when working in health care environment, especially with established patient friendships and family involvement. Breaking bad news such as a poor prognosis, diagnosis, recurrence or transition to terminal care require a higher level of communication to ensure both patient and healthcare worker understand and deal with the circumstances appropriately. AHPs not trained regarding the correct communication strategy to use when delivering bad news may cause a patient to distort information, become overly optimistic and recruit a state of denial. The AHP may not deliver the news effectively to avoid causing the patient upset, or because the AHP is worried about being blamed for the treatment not having worked.
A study was conducted on a patient population with a terminal illness; they interviewed the patients regarding the first diagnosis of their illness[47]. The study focused on what the patients remembered to be an effective communication strategy recruited by their healthcare provider. Four main themes emerged from the qualitive study which the patients regarded as an important approach to breaking the news. These were:
- Health provider being well informed of their condition and upto date with recent research
- Health provider recommending treatment options and taking time to answer any questions
- An honest approach, giving the patient all valid information about their condition
- The health provider using simple term which made sense to the patient
Primarily the AHP should have the basic level of communication skills to use with their patient. The healthcare provider working with their terminally ill patient should ensure that the patient is familiar with their condition, question if the patient has health concerns which need addressing and/or if the patient may needs more information about their illness and treatment. The patient’s emotions should be addressed with an empathic, validated and clarified response. Often overlooked is the family/care giver’s input which needs to be established from the early stages of the patient’s treatment.
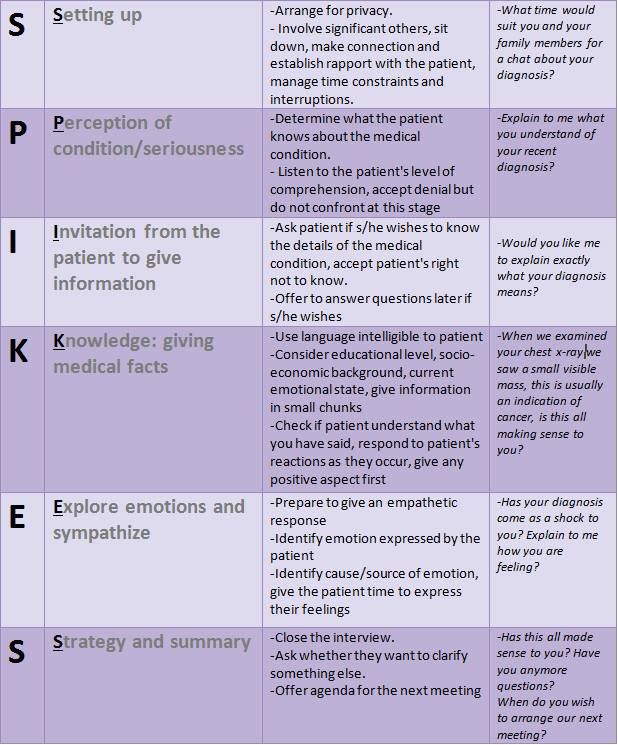
An effective strategy to respond to the important implications mentioned above is the recruitment of the SPIKES communication approach. SPIKES[48] (table 1.), is specifically designed to deal with breaking bad news to terminally ill patients. This protocol addresses issues such as a poor diagnosis, prognosis, and return of an illness, conversion to terminal care or even a medical error. This strategy has also proven to provide the healthcare messenger with an increased confidence in their ability to address negative information with their patient. The healthcare provider use the approach to plan communicating the news in the best way, which holds a reflective role to reduce anxiety or fear for the AHP. The SPIKES approach is a short, suitable to all conditions approach, which is easy to understand and follow.
Table 1. SPIKES communication protocol[48].
Back et al. [49] studied this communication strategy on a group of patients with a terminal illness. An audio recording of a healthcare worker breaking bad news to a fictional patient was used. The recording where the SPIKES strategy was recruited was favoured by the patients, and popular aspects of the recording were noted. The patients favoured how the healthcare providers using the strategy addressed the patient’s emotions; the empathetic response of the AHP was also valued by the patient. The AHP’s guidance and knowledge of future planning options was also presently addressed, not over-loading the patient with information or using confusing medical terms. The AHP’s ability to address positive strengths for that individual patient was also acclaimed.
De-escalation Strategies[edit | edit source]
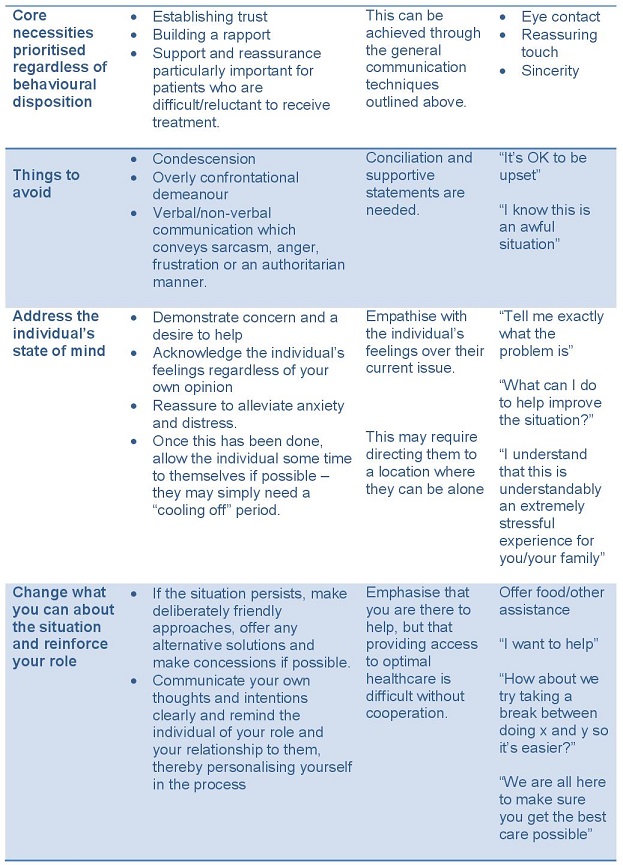
As previously stated, zero tolerance or any form of physical restraint in VAB situations is only going to result in an escalation of conflict in the healthcare environment[50]. As such the practise of avoiding interaction with individuals exhibiting VAB is more of a protective strategy for staff than a resolution for the developing issue[51]. Current research demonstrates that the most sound strategy for de-escalation of VAB involves early identification of potentially volatile situations and the use of effective interpersonal skills to talk down the individual in question[50]. These interpersonal skills consist of verbal and non-verbal communication of a willingness to collaborate with the aggrieved individual in search of an alternate solution to the current problem[52]. It is worth noting that these strategies place increased cognitive demand on AHPs working in an already demanding environment – a conscious decision must be made to address the developing situation before it gets out of hand. Wand and Coulson (2006) recommend the following hierarchy of interventions for VAB[50]:
Barriers this tool meets:
- Lack of empathy
- Lack of education
- Frustration
A major barrier to the above interventions is that often in these situations a stand-off can occur between the individual and the AHP. Before physical restraint is used to ensure the safety of everyone proximal to the scene, a coordinated team effort should be made to calm the individual down, as a demonstration of team unity protects individual AHPs from being singled out and has been shown to effective in getting VA individuals to back down [53].
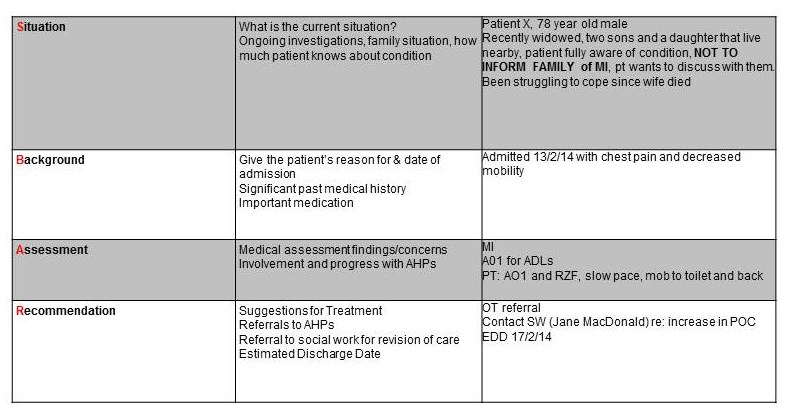
Situation Background Assessment Recommendation[edit | edit source]
The Situation Background Assessment Recommendation (SBAR) tool is designed to improve communication between healthcare professionals, clinicians and nursing staff and increase patient safety. The tool was originally designed for military and aviation use, and has since been adapted for healthcare settings.[54] Different Health Boards have adapted the SBAR for different uses. Within the acute setting, SBAR can be used as a handover tool, for information sharing between staff at the beginning of a shift and when transferring a patient between wards or hospitals.[55] SBAR can also aid communication between primary and secondary care providers by including an SBAR tool within discharge/referral letters. Houston et al., found this technique allowed for vital information to be shared in a clear and concise manner between health professionals, improving the communication between primary and secondary care.[56] Velji et al., stated that staff in a rehabilitation setting found that an adapted SBAR tool was useful for both individual and team communications.[57] SBAR allows for information to be shared in a timely and effective manner which is crucial due to the time constraints and pressures faced by healthcare staff. By using the SBAR, all staff have the opportunity to find out previous medical assessments and recommendations from other healthcare professionals, collated in one place rather than having to seek relevant information from individuals previously involved in the patients’ healthcare.
Different health boards use different formats, some have daily hand outs available to staff, while others prefer just to have tool outline displayed so that the staff can use it as a reference when communicating with other staff members.[54] Regardless of the format, the content communicated remains the same.
Barriers this tool meets:
· Time Constraints/Shortages
· Responsibility/Collaboration between AHPs
Case Studies: Real Life Situations[edit | edit source]
Case Study: Terminal Illness and Denial[edit | edit source]
Mr. X was diagnosed with stage II nasopharyngeal cancer with lymph node metastasis three years before a readmission to hospital following poor health. The second admission to hospital concluded the cancer had spread to his lungs and liver resulting in a poor prognosis. Mr. X had denied the initial cancer diagnosis to his family, and had refused any follow up treatment offered to him.
Case Study 2: Aggressive Abusive Patient[edit | edit source]
Case Study 3[edit | edit source]
References[edit | edit source]
- ↑ Health and Care Professional Council. Professionalism in Healthcare Professionals. 2014; Available at: http://www.hcpc-uk.org/assets/documents/10003771Professionalisminhealthcareprofessionals.pdf. Accessed November 13, 2014.
- ↑ 2.0 2.1 2.2 Ha J, Longnecker N. Doctor-patient communication: a review. Ochsner Journal; 2010: 10(1): 38-43
- ↑ Mehnert A, Lehman C, Cook U. Difficult communication situations in doctor-patient interactions. Federal health journal; 2012; 2(12): 111-116
- ↑ Mental Health Foundation. What is mental health problems? 2014; Available at: http://www.mentalhealth.org.uk/help-information/an-introduction-to-mental-health/what-are-mental-health-problems/. Accessed November 21, 2014.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Giandinoto J, Edward K. Challenges in acute care of people with co-morbid mental illness. British Journal of Nursing 2014;23(13):728-732.
- ↑ 6.0 6.1 6.2 Zolnierek CD, Clingerman EM. A medical-surgical nurse's perceptions of caring for a person with severe mental illness. J Am Psychiatr Nurses Assoc 2012 Jul-Aug;18(4):226-235.
- ↑ 7.0 7.1 7.2 Happell B, Scott D, Platania‐Phung C, Nankivell J. Should we or shouldn't we? Mental health nurses' views on physical health care of mental health consumers. International journal of mental health nursing 2012;21(3):202-210.
- ↑ 8.0 8.1 Kaufman E, McDonnell M, Cristofalo M, Ries R. Exploring barriers to primary care fo patients with severe mental illness: frontline patient and provider accounts. Issues in mental health nursing 2012; 33(3): 172-180.
- ↑ 9.0 9.1 9.2 Goode D, Melby V, Ryan A. Management of patients with mental health needs: Debbie Goode and colleagues assess whether staff are prepared to offer person-centred care to all people who present to emergency departments. Emergency Nurse 2014;22(5):32-37.
- ↑ National Institute for Health and Care Excellence. Self-harm: The short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. 2014; Available at:http://www.nice.org.uk/guidance/cg16/chapter/1-guidance. Accessed November 6, 2014.
- ↑ 11.0 11.1 11.2 Kool N, vanMeijel B, Koekkoek B, vanderBijl J, Kerkhof A. Improving communication and practical skills in working with inpatients who self-harm: a pre-test/post-test of the effects of training programme. Biomed central psychiatry; 2014: 14(64).
- ↑ 12.0 12.1 Stensrud T, Mjaaland T, Finset A. Communication and mental health in general practice: physicians' self-perceived learning needs and self-efficacy. Mental Health Family Medicine; 2012: 9(3): 201-209
- ↑ 13.0 13.1 World Health Organization. Obesity and Overweight. 2014; Available at: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 11/08, 2014.
- ↑ You L, Sadler G, Majumdar S, Burnett D, Evans C. Physiotherapists' perceptions of their role in the rehabilitation management of individuals with obesity. Physiotherapy Canada 2012;64(2):168-175.
- ↑ 15.0 15.1 15.2 Ferrante JM, Piasecki AK, Ohman‐Strickland PA, Crabtree BF. Family physicians' practices and attitudes regarding care of extremely obese patients. Obesity 2009;17(9):1710-1716.
- ↑ 16.0 16.1 National Institute for Health and Care Excellence. Obesity: Guidance on the prevention, identification,assessment and management of overweight and obesity in adults and children. 2006; Available at: http://www.nice.org.uk/guidance/cg43/chapter/1-guidance. Accessed 11/08, 2014.
- ↑ Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity 2013;21(10):2146-2152.
- ↑ 18.0 18.1 18.2 18.3 Teixeira FV, Pais-Ribeiro JL, Maia, Ângela Rosa Pinho da Costa. Beliefs and practices of healthcare providers regarding obesity: a systematic review. Revista da Associação Médica Brasileira 2012;58(2):254-262.
- ↑ 19.0 19.1 Epstein L, Ogden J. A qualitative study of GPs' views of treating obesity. British Journal of General Practice 2005;55(519):750-754.
- ↑ 20.0 20.1 Bleich SN, Bennett WL, Gudzune KA, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity 2012;20(5):999-1005.
- ↑ 21.0 21.1 21.2 21.3 Fallowfield LJ, Jenkins VA, Beveridge HA. Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med 2002 Jul;16(4):297-303.
- ↑ Rose JH, Radziewicz R, Bowmans KF, O'Toole EE. A coping and communication support intervention tailored to older patients diagnosed with late-stage cancer. Clin Interv Aging 2008;3(1):77-95.
- ↑ Black K. Health care professionals' death attitudes, experiences, and advance directive communication behavior. Death Stud 2007;31(6):563-572.
- ↑ 24.0 24.1 Hjörleifsdóttir E, Carter DE. Communicating with terminally ill cancer patients and their families. Nurse Educ Today 2000;20(8):646-653.
- ↑ Clayton JM, Butow PN, Tattersall MH. When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. J Pain Symptom Manage 2005;30(2):132-144.
- ↑ 26.0 26.1 Curtis JR, Patrick DL. Barriers to Communication About End‐of‐Life Care in AIDS Patients. Journal of general internal medicine 1997;12(12):736-741
- ↑ 27.0 27.1 27.2 27.3 27.4 Hordern A, Grainger M, Hegarty S, Jefford M, White V, Sutherland G. Discussing sexuality in the clinical setting: the impact of a brief training program for oncology health professionals to enhance communication about sexuality. Asia-Pacific Journal of Clinical Oncology 2009;5(1): 270-277
- ↑ 28.0 28.1 Brandenburg U, Bitzer J. The challenge of talking about sex: The importance of patient-physican interaction. Maturitas 2009;63(2): 124-127
- ↑ 29.0 29.1 29.2 29.3 Gott M, Galena E, Hinchliff S, Elford, H.“Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Family Practice 2004;21(5): 528-536.
- ↑ 30.0 30.1 30.2 Macdowall W, Parker R, Nanchahal K, Ford C, Lowbury R, Robinson A, Sherrard J, Martins H, Fasey N, Wellings K. ‘Talking of sex’: Developing and piloting a sexual health communication tool for use in primary care. Patient Education and Counselling 2010;81; 332-337.
- ↑ Association of Reproductive Health Professionals.Talking to patients about sexuality and sexual health. https://www.arhp.org/publications-and-resources/clinical-fact-sheets/sexuality-and-sexual-health (accessed 13 October 2014).
- ↑ 32.0 32.1 32.2 32.3 32.4 Duxbury J, Whittington R. Causes and management of patient aggression and violence: staff and patient perspectives. J Adv Nurs 2005;50(5):469-478.
- ↑ 33.0 33.1 Swain N, Gale C. A communication skills intervention for community healthcare workers: Perceived patient aggression is reduced. Int J Nurs Stud 2014.
- ↑ 34.0 34.1 Pich J, Hazelton M, Sundin D, Kable A. Patient‐related violence against emergency department nurses. Nurs Health Sci 2010;12(2):268-274.
- ↑ Whittington R, Shuttleworth S, Hill L. Violence to staff in a general hospital setting. J Adv Nurs 1996;24(2):326-333.
- ↑ National Audit Office. A Safer Place to Work: Protecting NHS Hospital and Ambulance Staff from Violence and Aggression. 2003; Available at: http://www.nao.org.uk/report/a-safer-place-to-work-protecting-nhs-hospital-and-ambulance-staff-from-violence-and-aggression/. Accessed November 2nd, 2014.
- ↑ 37.0 37.1 37.2 37.3 37.4 Hahn S, Hantikainen V, Needham I, Kok G, Dassen T, Halfens RJ. Patient and visitor violence in the general hospital, occurrence, staff interventions and consequences: a cross‐sectional survey. J Adv Nurs 2012;68(12):2685-2699.
- ↑ Stubbs B, Rayment N, Soundy A. Physiotherapy students’ experience, confidence and attitudes on the causes and management of violent and aggressive behaviour. Physiotherapy 2011;97(4):313-318
- ↑ Workforce and Facilities Team, Health and Social Care Information Centre (HSCIC). 2014; Available at: http://www.hscic.gov.uk/catalogue/PUB14705/data-writ-comp-nhs-2013-2014-rep.pdf. Accessed 25/11, 2014.
- ↑ 40.0 40.1 Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995 May 1;152(9):1423-1433.
- ↑ 41.0 41.1 41.2 Travaline JM, Ruchinskas R, D'Alonzo GE,Jr. Patient-physician communication: why and how. J Am Osteopath Assoc 2005 Jan;105(1):13-18.
- ↑ Ong LM, De Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med 1995;40(7):903-918.
- ↑ Haskard KB, White MK, Williams SL, DiMatteo MR, Rosenthal R, Goldstein MG. Physician and patient communication training in primary care: effects on participation and satisfaction [corrected] [published erratum appears in HEALTH PSYCHOL 2009 Mar;28(2):263]. Health Psychol 2008 09;27(5):513-522.
- ↑ 44.0 44.1 44.2 Bundy C. Changing behaviour: using motivational interviewing techniques. J R Soc Med 2004;97 Suppl 44:43-47.
- ↑ 45.0 45.1 Pollak KI, Alexander SC, Coffman CJ, Tulsky JA, Lyna P, Dolor RJ, et al. Physician communication techniques and weight loss in adults: Project CHAT. Am J Prev Med 2010;39(4):321-328.
- ↑ Borrelli B, Riekert KA, Weinstein A, Rathier L. Brief motivational interviewing as a clinical strategy to promote asthma medication adherence. J Allergy Clin Immunol 2007;120(5):1023-1030.
- ↑ Parker PA, Baile WF, de Moor C, Lenzi R, Kudelka AP, Cohen L. Breaking bad news about cancer: patients' preferences for communication. J Clin Oncol 2001 Apr 1;19(7):2049-2056
- ↑ 48.0 48.1 Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000;5(4):302-311.
- ↑ Back AL, Trinidad SB, Hopley EK, Arnold RM, Baile WF, Edwards KA. What patients value when oncologists give news of cancer recurrence: commentary on specific moments in audio-recorded conversations. Oncologist 2011;16(3):342-350.
- ↑ 50.0 50.1 50.2 Wand TC, Coulson K. Zero tolerance: a policy in conflict with current opinion on aggression and violence management in health care. Australasian Emergency Nursing Journal 2006;9(4):163-170.
- ↑ Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabilitation nursing 2010;35(5):177-184.
- ↑ Davidson R, Mills M. Cancer patients’ satisfaction with communication, information and quality of care in a UK region. European journal of cancer care 2005;14(1):83-90.
- ↑ Kao L, Moore G. The violent patient: clinical management, use of physical and chemical restraints, and medicolegal concerns. Emerg Med Prac 1999;1(6):1-24.
- ↑ 54.0 54.1 NHS. SBAR-Situation-Background-Assessment-Recommendation 2009. http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/sbar_-_situation_-_background_-_assessment_-_recommendation.html (accessed 12 November 2014)
- ↑ Powell SK.SBAR – It’s Not Just Another Communication Tool.Professional Care Management 2007;12(4):195-196. http://journals.lww.com/professionalcasemanagementjournal/Citation/2007/07000/SBAR_It_s_Not_Just_Another_Communication_Tool.1.aspx (accessed 12 November 2014)
- ↑ Houston N, Mondoa C. Using SBAR to improve clinical communication between cardiology outpatients and primary care teams. NHS Quality Improvement Scotland 2009. http://yhhiec.org.uk/wp-content/uploads/2011/10/Using-SBAR-to-improve-clinical-communication-between-cardiology-outpatients-and-primary-care-teams-PSC-2010-68.pdf (accessed 12 November 2014)
- ↑ Velji K, Baker GR, Fancott C, Anderoli A, Boaro N, Tardi G, Aimone E, Sinclair L. Effectiveness of an Adapted SBAR Communication Tool for a Rehabilitation Setting [online]. Healthcare Quarterly 2008;11(3):72. http://www.longwoods.com/content/19653 (accessed 12 November 2014).