Wrist and Hand Osteoarthritis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 50: | Line 50: | ||
<br>• Laboratory markers such as rheumatoid factor (RF) and erythrocyte sedimentation rate (ESR). Blood tests are not required but recommended to exclude potential coexisting diseases<sup>4</sup>. | <br>• Laboratory markers such as rheumatoid factor (RF) and erythrocyte sedimentation rate (ESR). Blood tests are not required but recommended to exclude potential coexisting diseases<sup>4</sup>. | ||
<br> | |||
<br><br> | |||
<br>Risk Factors<sup>4</sup>:<br>• female gender<br>• increasing age over 40<br>• menopausal status<br>• family history<br>• obesity<br>• higher bone density<br>• greater forearm mm strength<br>• joint laxity<br>• prior hand injury<br>• occupational and recreation-related usage | |||
Altman Diagnostic Criteria 1990 (Sn .92, Sp .98)<sup>7</sup><br>• Presence of hand pain, aching, or stiffness plus<br>• hard tissue enlargement of at least 2 of 10 selected joints<br>• plus less than 3 swollen metacarpophalangeal joint<br>• plus either hard tissue enlargement of at least 2 distal interphalangeal<br>• joints or deformity of at least 1 of 10 selected joints<br><br> | |||
== Outcome Measures == | == Outcome Measures == | ||
Revision as of 23:30, 17 March 2011
Let me know if you need any assistance.Be the first to edit this page and have your name permanently included as the original editor, see the editing pages tutorial for help.
|
Original Editor - Your name will be added here if you created the original content for this page. Lead Editors - Your name will be added here if you are a lead editor on this page. Read more. |
Clinically Relevant Anatomy and Epidemiology
[edit | edit source]
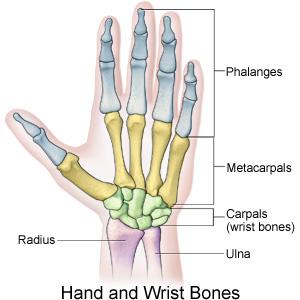
The wrist and hand are composed of 27 bones: 8 bones of the wrist, 5 metacarpals and 14 bones of the phalanges. In this degenerative disorder, the articular cartilage wears away, exposing the bones. Cartilage is an elastic connective tissue whose purpose is to allow for a smooth, gliding motion between joints1.
Incidence:
• Most common musculoskeletal disorder worldwide affecting the hands
• Age
o Incidence increases after 55 in women
o Rate of progression increases with age2
• Gender
o More common and more severe in women
• Observed sex differences become evident after menopause3
o The typical locations of degeneration in patients with osteoarthritis are the distal and interphalangeal joints of the hand4
• Genetics
o Women
• Gene mutations that code for collagen II may increase the risk of developing early OA
• Role of human leukocyte antigen (HLA) types regarding the risk of OA remains much debated
• Handedness
o HOA mostly occurs on the dominant hand5
Prevalence:
• Continuing to increase as the majority of our population increases
Pathological Process
[edit | edit source]
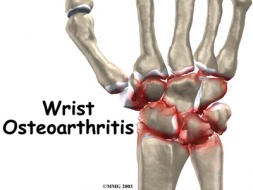
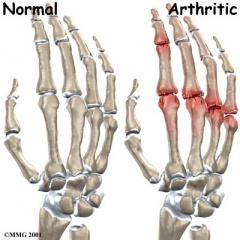
Osteoarthritis is a disorder of the entire synovial joint organ and involves more structures than articular cartilage. The tissue changes that occur in the hand and wrist are a result of imbalance between catabolic and anabolic repair activity2. Current evidence states that the subchondral bone may be the primary etiologic agent in osteoarthritis and joint cartilage is simply the final target of the process. Periarticular bone changes occur very early in the development of OA and these changes can be segregated into distinct patterns based on the anatomic location and pathogenic mechanisms6. There is a progressive increase in subchondral plate thickness, alterations in the architecture of subchondral trabecular bone, formation of new bone at joint margins (osteophytes), and development of sub chondral bone cysts. Once the pathology reaches the articular cartilage, the cartilage thins and the joint space narrows. This causes sclerosis of the subchondral bone due to the new mechanical load placed on the affected joint2.
Clinical Presentation4[edit | edit source]
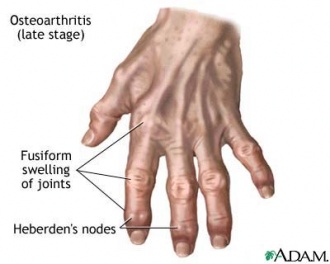
• Pain
• Swelling
• Stiffness, particularly in the mornings
Pain, swelling and stiffness primarily targeted to DIP, PIP, thumb base, index and middle MCP joints.
• Muscle weakness
• Difficulty gripping and twisting objects (doorknobs)
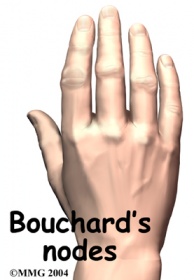
• Presence of Heberden (on distal IP joints) or Bouchard nodes (on proximal IP joints) or bony enlargements.
* clinical hallmark*
Diagnostic Procedures[edit | edit source]
• Diagnosis difficult to make due to the number of joints involved, the broad spectrum of severity and possible subsets of criteria which may exist.
• Imaging:
o Radiographs (gold standard). Note joint space narrowing; osteophytes; subchondral bone: sclerosis, cysts, erosion4;
• Kellgren-Lawrence grading allows a wide range of interpretations for each grade, reducing inter-observer reliability
• Verbruggen and colleagues suggest an easy and reproducible scoring method, using numeric scores for radiographs5
o MRI
o Scintigraphy
Use of radiographs is the form of imaging most seen clinically.
• Laboratory markers such as rheumatoid factor (RF) and erythrocyte sedimentation rate (ESR). Blood tests are not required but recommended to exclude potential coexisting diseases4.
Risk Factors4:
• female gender
• increasing age over 40
• menopausal status
• family history
• obesity
• higher bone density
• greater forearm mm strength
• joint laxity
• prior hand injury
• occupational and recreation-related usage
Altman Diagnostic Criteria 1990 (Sn .92, Sp .98)7
• Presence of hand pain, aching, or stiffness plus
• hard tissue enlargement of at least 2 of 10 selected joints
• plus less than 3 swollen metacarpophalangeal joint
• plus either hard tissue enlargement of at least 2 distal interphalangeal
• joints or deformity of at least 1 of 10 selected joints
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.