Wrist and Hand Examination
Let me know if you need any assistance.Be the first to edit this page and have your name permanently included as the original editor, see the editing pages tutorial for help.
|
Original Editor - Your name will be added here if you created the original content for this page. Lead Editors - Your name will be added here if you are a lead editor on this page. Read more. |
Subjective[edit | edit source]
Thorough history taking is an important first step in treating the patient. Each physical therapist will develop their own style and technique, but a good interview will include the basic elements discussed below.
History
[edit | edit source]
Clinical Presentation
- Mechanism of the injury-How the injury occurred and what was the cause.
- Location of the pain
- Timeline-When is the pain at its worse and when is it relieved?
- Presence and location of numbness and tingling.
- Aggravating and relieving factors.
- Were any diagnostic test/imaging performed and what were the results?
Red Flags
[edit | edit source]
This section deals with screening the patient for possible serious pathologies that could cause wrist or hand pain. These conditions could warrant a referral, or consultation.
Infections
- Heat
- Swelling
- Pain
- Redness
- Inflammation
Fracture/dislocation:
Top five physical findings which are most useful in screening for wrist fracture.[1]
- Localized tenderness (Sensitivity [Sn] 94%)
- Pain on active motion (Sn 97%)
- Pain on passive motion (Sn 94%)
- Pain on grip (Sn 71%)
- Pain on supination (Sn 68%)
- Bottom line: Any one of the above findings associated with a history of trauma should be sent for radiographs
Colles fracture
Scaphoid fracture
Additional potentially serious conditions
Peripheral Vascular Disease
Peripheral Neuropathy:
- Hx: Older age, >65. The risk is same for men/women.
- Risk factors include hypertension, hypercholesterolemia, obesity, diabetes, and smoking. Commonly affects lower extremity over upper extremity.
Upper extremity nerve injuries involving
- Median
- Radial
- Ulnar
Differential Diagnosis
[edit | edit source]
Carpal Tunnel Syndrome
Anterior Interosseous Syndrome
Posterior Interousseous Syndrome
Fractures
Osteoarthritis
- First Carpometacarpal Osteoarthritis
- Hand and Wrist Osteoarthritis
Radial Tunnel Syndrome
Compression of the Ulnar nerve at Guyon’s canal
Non-specific wrist pain (mechanical wrist pain)
- Can include wrist strain, sprain, joint dysfunction, repetitive injuries or h/o trauma without specific identified diagnosis.
Trigger Finger
Complex Regional Pain Syndrome
Triangular Fibrocartilaginous Complex
Dupuytren’s Contracture
Outcome Measures
[edit | edit source]
- DASH:
- Quick DASH
- Symptom Severity Scale
- Patient Specific Functional Scale
Objective[edit | edit source]
Observation[edit | edit source]
Vital Signs
Posture
- During the posture examination the physical therapist should examine from the lateral, posterior, and anterior views looking at the position of the cervical and thoracic spine along with the shoulder, elbow, forearm, wrist, and hand.
- Carrying angle
- Shoulder height
- Muscle girth or presence of atrophy
Swelling
Muscle wasting
- Median Nerve (depending on area impingement)
- Muscle wasting in the first three and fingers and half the fourth fingers on radial side of the hand. The muscle involved LOAF) are:
- Lumbricals
- Oppenens pollicis
- Adbuctor pollicis brevis,
- Flexor pollicis brevis
Radial Nerve (depending on area of impingement)
- Common muscles that are affected by radial nerve entrapment are primarily on the dorsal aspect of the hand.
- Supinator
- Extensor carpi ulnaris
- Extensor digitorum communis
- Extensor digiti quinti
- Abductor pollicis longus
- Extensor pollicis brevis
- Extensor indicis propius
Ulnar Nerve (depending on area of impingement)
- Muscle wasting in the hand for the ulnar nerve occurs primarily in the fifth and half the fourth fingers, in the hypothenar area. The muscles that are affected are:
- Abductor digiti minimi
- Opponens digiti minimi
- Flexor digiti minimi
- 3rd and 4th lumbrical
- 1st -3rd palmar interosseous
- 1st – 4th dorsal interosseous
- Flexor pollicis brevis
- Adductor digiti minimi
Screen Proximal Joints
When examining a patient with a distal upper extremity condition it is advisable for the therapist to screening proximal structures to determine if they are involved in the patient’s clinical presentation. Below are some common ways physical therapists may screen these proximal structures.
- Cervical
- Accessory motion testing
- ROM with over pressures
- ULNT1(Upper limb neurodynamic test[2]
- Shoulder
- Passive ROM with overpressure
- Active ROM of glenohumeral, acromioclavicular, sternoclavicular
- Muscle strength testing
- Assess for glenohumeral internal rotation deficit (GIRD)
- Elbow
- Passive ROM, active ROM with over pressure
- Muscle strength testing
[edit | edit source]
Functional Tests
[edit | edit source]
The goals of functional tests are to obtain and quantify an asterisk to assess/reassess after intervention is performed. Which impairments could be underlying their inability to perform the functional task? Some examples are turning a door knob, holding a key, initial pain free grip or key grip.
Palpation[edit | edit source]
Wrist/hand
- Extensor Pollicus Brevis/Abductor Pollicus Longus tendons
- Scaphoid
- Guyon’s canal
- Distal to lister’s tubercle
- Lunotriquetral joint/fovea for Triangular Fibrocartilaginous Complex
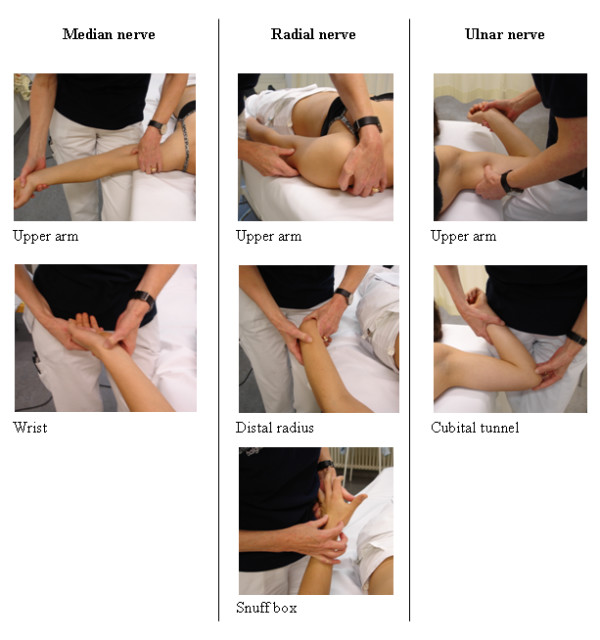
Upper Extremity Nerve Palpation:
To reproduce symptoms if a peripheral nerve entrapment diagnosis is suspected positive response is increase in pain or symptoms elicited different from the unaffected arm.
Good reliability (Kappa =.593)[3]
- To palpate the 3 major nerves of the upper extremity refer to the figure below.
- Median: Position patient supine, 90 degrees of shoulder abduction and elbow extension. Palpate medially to the bicep (mid humeral). Palpate distally at wrist.
- Radial: Upper arm (0 degrees of abduction, palpate proximal to the lateral epicondyle), distal radius, and snuffbox
- Ulnar: Upper arm (medial mid humeral area, shoulder 90 degrees of abduction, elbow 120 degrees of flexion) and cubital tunnel
Adapted from Schmid et al 2009
Neurologic Assessment
[edit | edit source]
Reflexes
- C5-C7
Myotomes
- C5-T1
Dermatomes
- C5-T1
Movement Testing[edit | edit source]
If patient is pain free to end range, the physical therapist may choose to apply overpressure.
- Wrist
- Flexion/Extension
- Radial/Ulnar deviation
- 1st CMC
- Extension
- Abduction
- Opposition
- Metacarpal-phalangeal (MCP)
- Flexion
- Extension
- Abduction/Adduction
- Inter-phalangeal (IP)/Distal IP/Proximal IP
- Flexion
- Extension
Muscle Strength test of the wrist and hand
- Wrist flexion/extension
- Forearm pronation and supination
- Grip strength
- Key and pinch grip strength
Special Tests[edit | edit source]
The physical therapist may elect to perform various special tests during the physical examination of an individual with wrist or hand complaints. Below are potential tests that may be utilized categorized by possible diagnosis or tissue involvement.
- Neurodynamic tests
- Median nerve bias (Upper limb tension test 1 [ULTT] /UpperLimb Tension Test 2a)
- Radial nerve bias (ULTT2b)
- Ulnar nerve bias (ULTT3)
- Carpal compression test
- Tinel’s test
- Wrist-ratio index
DeQuervain’s syndrome
- Finkelstein’s test
- Palpation radial styloid
- Resisted 1st digit extension for pain provocation
References[edit | edit source]
1. Cevik AA, Gunal I, Manisali M, et al. Evaluation of physical findings in acute wrist trauma in the emergency department. Ulus Travma Acil Cerrahi Derg. 2003;9(4):257-261.
2. Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28(1):52-62.
3. Schmid AB, Brunner F, Luomajoki H, et al. Reliability of clinical tests to evaluate nerve function and mechanosensitivity of the upper limb peripheral nervous system. BMC Musculoskelet Disord. 2009;10:11.
- ↑ Cevik AA, Gunal I, Manisali M, et al. Evaluation of physical findings in acute wrist trauma in the emergency department. Ulus Travma Acil Cerrahi Derg. 2003;9(4):257-261.
- ↑ Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28(1):52-62.
- ↑ Schmid AB, Brunner F, Luomajoki H, et al. Reliability of clinical tests to evaluate nerve function and mechanosensitivity of the upper limb peripheral nervous system. BMC Musculoskelet Disord. 2009;10:11.