Wallenberg Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
Some common symptoms of Wallenberg Syndrome include<ref name="Nicholson" /><ref name="day">Day GS, Swartz RH, Chenkin J, Shamji AI, Frost DW. Lateral medullary syndrome: a diagnostic approach illustrated through case presentation and literature review. CJEM. 2014 Mar 1;16(02):164-70.</ref><ref name="GARD">Genetic and Rare Diseases Information Centre: Wallenberg Syndrome. https://rarediseases.info.nih.gov/diseases/9263/wallenberg-syndrome (accessed 6 May 2017).</ref>[[Image:Clinical Picture.png|thumb|right|400x400px|Clinical Picture based on Location (Nicholson, 2009).]]: | Some common symptoms of Wallenberg Syndrome include<ref name="Nicholson" /><ref name="day">Day GS, Swartz RH, Chenkin J, Shamji AI, Frost DW. Lateral medullary syndrome: a diagnostic approach illustrated through case presentation and literature review. CJEM. 2014 Mar 1;16(02):164-70.</ref><ref name="GARD">Genetic and Rare Diseases Information Centre: Wallenberg Syndrome. https://rarediseases.info.nih.gov/diseases/9263/wallenberg-syndrome (accessed 6 May 2017).</ref>[[Image:Clinical Picture.png|thumb|right|400x400px|Clinical Picture based on Location (Nicholson, 2009).]]: | ||
• Vertigo<br>• Nausea and vomiting<br>• Difficulty with balance and ambulation<br>• Difficulty maintaining sitting posture<br>• Blurry vision<br>• Horizontal or rotational nystagmus<br>• Crossed hemisensory disturbance<br>• Ipsilateral reduction in pain | • Vertigo<br>• Nausea and vomiting<br>• Difficulty with balance and ambulation<br>• Difficulty maintaining sitting posture<br>• Blurry vision<br>• Horizontal or rotational nystagmus<br>• Crossed hemisensory disturbance<br>• Ipsilateral reduction in pain & temperature sensation over the face<br>• Contralateral reduction in pain & temperature sensation over trunk<br>• Hoarseness<br>• Poor gag reflex<br>• Ataxia<br>• Dysphonia<br>• Dysphagia<br>• Diplopia<br>• Hiccups<br>• Horner's syndrome (constricted pupil & drooping eyelid)<br>• Bradycardia <br> | ||
= Epidemiology/Etiology/Prognosis = | = Epidemiology/Etiology/Prognosis = | ||
Revision as of 01:52, 7 May 2017
Introduction [edit | edit source]
According to the National Institute of Neurological Disorders and Stroke, Wallenberg Syndrome (aka Lateral Medullary Syndrome) is a neurological condition caused by a blockage of the vertebral artery (VA) or posterior inferior cerebellar artery (PICA), ultimately leading to infarction of the lateral medulla [1]. Stroke occurring in this region of the brainstem often leads to a variety of impairments, as patients typically present with motor, sensory, cognitive, perceptual, speech and language deficits. Wallenberg Syndrome was first described in 1808 by Gaspard Vieusseux. However, a more detailed description was given in 1895 by Adolf Wallenberg himself, which highlighted this condition as an infarction of the lateral medulla oblongata following occlusion of the VA/PICA[2].
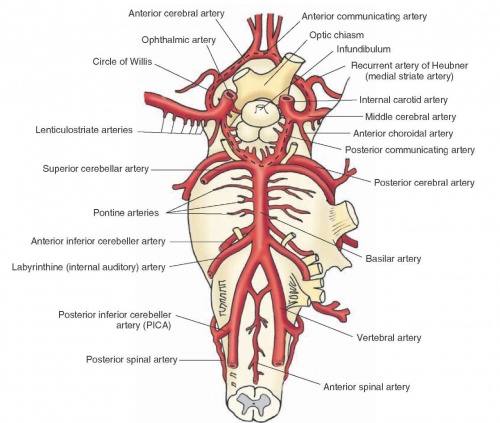
Clinically Relevant Anatomy[edit | edit source]
The VA runs along the ventro-lateral aspect of the brainstem supplying the medulla. The VA branches off to form PICA which runs dorsally and crosses over/supplies the lateral medulla on its way to the cerebellum. Structures that make up the lateral medulla include the inferior cerebellar peduncle, vestibular nuclei, trigeminal nucleus and tract, spinothalamic tract, descending sympathetic fibres, nucleus ambiguus and nucleus solitarius[3].
Clinical Presentation
[edit | edit source]
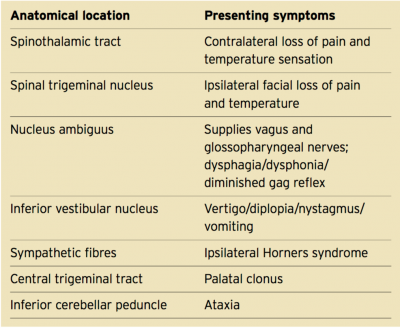
Due to the very compressed placement of nuclei and tracts within the lateral medulla, Wallenberg Syndrome (resulting from a stroke in the VA or PICA) often leads to abnormalities in many systems, including: vestibulo-cerebellar, sensory, bulbar, respiratory, and autonomic[2]. Clinical presentations vary dependent on which specific nucleii and fibres are involved.
Some common symptoms of Wallenberg Syndrome include[3][4][5]
:
• Vertigo
• Nausea and vomiting
• Difficulty with balance and ambulation
• Difficulty maintaining sitting posture
• Blurry vision
• Horizontal or rotational nystagmus
• Crossed hemisensory disturbance
• Ipsilateral reduction in pain & temperature sensation over the face
• Contralateral reduction in pain & temperature sensation over trunk
• Hoarseness
• Poor gag reflex
• Ataxia
• Dysphonia
• Dysphagia
• Diplopia
• Hiccups
• Horner's syndrome (constricted pupil & drooping eyelid)
• Bradycardia
Epidemiology/Etiology/Prognosis[edit | edit source]
A study reviewing 25 cases of Wallenberg Syndrome found the incidence to be highest in middle-aged men at 55.06 years of age[2]. The greatest risk factor for Wallenberg Syndrome is currently believed to be atherosclerosis, which is often linked to a history of hypertension, diabetes, and smoking[4]. The most common cause of Wallenberg Syndrome is stroke in the VA or PICA of the brainstem. However, a number of other conditions have been found to be associated with Wallenberg Syndrome, including metastatic cancer, hematoma, aneurysm of the VA, head-injury, arteriovenous malformation, multiple sclerosis, and mechanical trauma/injury to the VA in the neck[1]. The long-term outlook varies quite substantially, with some individuals seeing a decrease in symptoms within weeks, whereas others may have symptoms persist for years[5]. With appropriate treatment, clinical monitoring, and post-stroke care, the prognosis for recovery remains positive. Majority of patients have minimal deficits at six months, and over 85% have been found to attain functional independence with ambulation within a year[4]. Overall, researchers have yet to confidently determine why this type of stroke occurs.
Diagnosis[edit | edit source]
Medical Management[edit | edit source]
All patients with suspected Wallenberg Syndrome should receive immediate care and neuroimaging, in order to exclude differential diagnoses and to screen for any contraindications to suggested stroke therapies[1]. In most cases, patients are initially prescribed medication, in order to combat chronic/long-lasting pain. Blood-thinners, such as heparin or warfarin, can also be prescribed to lessen the blockage in the arteries leading to the lateral medulla[1]. This is also an important component of preventing future blood-clots from forming, which would occlude the lateral medulla. In extreme cases with large blockages, surgery can sometimes be performed to remove the clot (although rarely performed due to the difficulty accessing this area of the brain).
Physiotherapy Management[edit | edit source]
Considering that Wallenberg Syndrome is most commonly the result of a stroke in the lateral medulla, this condition is managed using traditional stroke rehabilitation protocols, individualized to each particular patient.
The primary goal of any post-stroke rehabilitation program should be:
a.) Prevent complications
b.) Minimize impairments
c.) Maximize independence & function
Physical therapy can play an essential role in helping those with Wallenberg Syndrome regain their functional independence and community reintegration. Training should be extremely meaningful, engaging, and challenging. Instead of following a redundant mechanistic approach to rehabilitation, practitioners should instead use graded real-life activities that are purposeful and meaningful to the individual client[6]. As a result, treatment of Wallenberg Syndrome varies depending on the deficits shown by the client. In many cases of Wallenberg Syndrome, speech, language, and swallowing therapy may be beneficial[6].Treatment should focus on task-oriented training, environmental adaptation, and motor retraining in order to combat movement/balance deficits. Furthermore, it has been found that electrical stimulation has a beneficial effect on improving muscle strength and balance in patients with stroke[6]. Current best evidence supports the use of electrical stimulation for the facilitation of motor recovery, and should be incorporated early on in the rehabilitation program[6].
Reference[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 National Institute of Neurological Disorders and Stroke: Wallenberg Syndrome. https://www.ninds.nih.gov/disorders/all-disorders/wallenbergs-syndrome-information-page (accessed 4 May 2017).
- ↑ 2.0 2.1 2.2 Srivastava M, Abeetha S, Srivastava S. Posterior inferior cerebellar artery syndrome (Wallenberg syndrome). International J. of Healthcare and Biomedical Research. 2015 Jan;3(02):76-9
- ↑ 3.0 3.1 Nicholson J, Paralkar U, Lawton G, Sigston P. Lateral medullary syndrome causing vocal cord palsy and stridor. Journal of the Intensive Care Society. 2009 Jul;10(3):218-9.
- ↑ 4.0 4.1 4.2 Day GS, Swartz RH, Chenkin J, Shamji AI, Frost DW. Lateral medullary syndrome: a diagnostic approach illustrated through case presentation and literature review. CJEM. 2014 Mar 1;16(02):164-70.
- ↑ 5.0 5.1 Genetic and Rare Diseases Information Centre: Wallenberg Syndrome. https://rarediseases.info.nih.gov/diseases/9263/wallenberg-syndrome (accessed 6 May 2017).
- ↑ 6.0 6.1 6.2 6.3 Chan IT. An evidence-based practice for the treatment of lateral medullary syndrome. Hong Kong Journal of Occupational Therapy. 2009 Dec 1;19(2):50-5.