Understanding Red Flags in Patellofemoral Pain
Top Contributors - Carin Hunter, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Red flags are an important aspect of our assessments, but this often is overlooked in a patient with knee pain. Red flags are
We need to know what might be a red flag for patient safety and for correct referral to the appropriate place. If there has been any trauma to the knee it is advisable to make sure the correct investigations have been carried out. This could mean imaging or special tests.
Non-Traumatic Masquerading Conditions[edit | edit source]
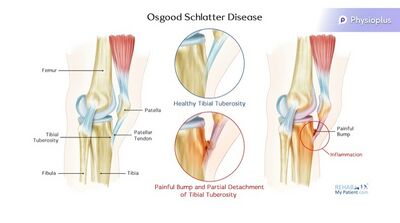
Osgood Schlatters[edit | edit source]
Signs and Symptoms:
- This condition is common in the 11-15 year old age group.
- prevalent in kids that do lots of quads dominant sports, so running, and kicking and jumping
- obvious bump at the tibial tubercle
- Pain specific to tibial tubercle
- inflammation and elevation of the growth plates in the tibial tuberosity, so the proximal tibia
- Can be confirmed on MRI to show level of inflammation
- Pain worsen to a point that it can prevent any participation in sport
Treatment:
- Education
- Activity modification - eliminate least fav sport, change playing position to a less active one to decrease load
- NSAIDS
- Ice Massage(Symptomatic relief)
- Address overload
- extrinsic factors
- load management of sport
- footwear
- landing technique
- intrinsic factors
- muscle length
- muscle strength
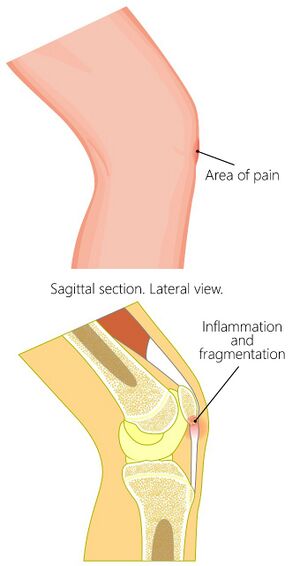
Sinding-Larsen-Johansson Disease[edit | edit source]
Signs and Symptoms:
- inflammation at the growth plate of the distal pole of the patella
- most likely to be seen at times of aggressive growth/growth spurts
- treatment tactics that I ask parents to do is to track growth because they're more likely to manage it well at times of aggressive growth with their activity modification.
- Pain worsen to a point that it can prevent any participation in sport
Treatment:
- Education
- Activity modification - eliminate least fav sport, change playing position to a less active one to decrease load
- NSAIDS
- Ice Massage(Symptomatic relief)
- Address overload
- extrinsic factors
- load management of sport
- footwear
- landing technique
- intrinsic factors
- muscle length
- muscle strength
Knee Effusion[edit | edit source]
A child should not have a knee effusion
Effusion very often leads to patellofemoral pain
A knee effusion in a child should always be investigated
Possible Causes:
- Systemic autoimmune disease, for example juvenile arthritis
- Infective arthritis
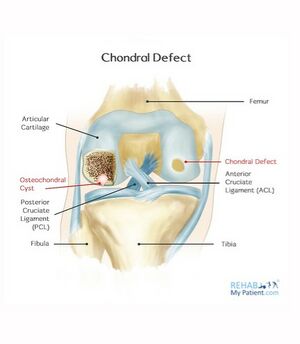
- Osteochondritis Dissecans
Osteochondritis Dissecans/Osteochondral Defect[edit | edit source]
cartilage and some of the subchondral bone can break off and float in the joint, which irritates the synovium, which in turn causes the effusion
Autoimmune Disease Red Flags:
- Multiple joint involvement
- Joint was stiff on waking
- Fatigue
- Infective arthritis red flags:
- Temperature
- Recent Illness
Osteochondritis Dissecans Treatment:
- Possible debridement/knee washed out
- Review, ideally, the OCDs, the osteochondral defects, with MRI. And what they're looking for there is how stable are the margins of the osteochondral defect and where are they? Are they in a very weight-bearing zone or not? And with respect to the stability, the margins, I think about it a bit like a divot on a golf course. So, sometimes you might have a really clean bit of grass, the soil has been removed, and it's not all crumbling in. So, that's a stable situation. And then we might have a divot on a golf course where the grass and soil has been removed and the soil is just crumbling in, and that would be an unstable OCD and there
- Possible surgical resection ly they might need to resect back to a stable margin.
- Monitor bone oedema around these defects, which over time, serially scanned, you're looking for those to decrease. So, from a
- physiotherapy point of view, we're looking at load management. Understanding, for example, in the patellofemoral joint if we've got a trochlear OCD, then we're not going to be wanting to do lots of deep loaded flexion, for example. So, message there without a doubt, do not sit on a child with an effused knee
Always refer a child with a knee effusion for further investigations to establish an underlying cause
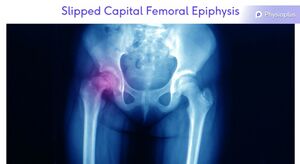
Slipped Capital Femoral Epiphysis[edit | edit source]
Okay, let's keep going with the teenagers. So, the next one is not common in terms of referring pain to the knee, but I have seen it, so I want to have it on my list and that is slipped epiphysis. So, now right up to the proximal femur, and we know that that area can refer to anteromedial knee. And the patient that I recall came to me with anteromedial knee pain, no hip pain but the position of the limb, the rotation of the limb, it was shortened, was all completely wrong. And I couldn't have immediately said it slipped epiphysis, but I knew that there was something going on at the hip and had an urgent review with one of my surgical colleagues. So, be on your guard for that.
Others[edit | edit source]
Less common but more serious:
- Systemic Auto-Immune Disease
- Slipped Epiphysis
- FAI
- Leukaemia
- Metastatic Neuroblastoma
- Primary Bone Tumour
- Red Flags
- Night pain
- Weight loss
- Malaise
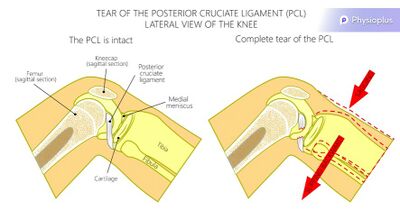
PCL Rupture[edit | edit source]
Can be caused by a blow to the front of the knee
can present with PFJ pain only
Assess all ligaments to see if surgery is necessary
Quadriceps rehabilitation
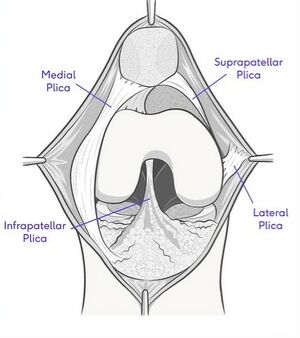
Synovial Plica[edit | edit source]
a plica is a fold in the synovial membrane
common
normally asymptomatic
Can be palpated anteromedially, perhaps next to the superior half of the patella, you can feel a little ridge and you can even sort of flick over them, palpate them. But the key thing is, is it painful? And is it their pain if you flick over it and it's painful? And also, occasionally, they can get trapped into the patellofemoral joint,
Can become impinged or inflamed and sore.
Use of a local anaesthetic diagnostically , and if they're injected with local anaesthetic and their pain goes off, well, we've got our answer that the plica is relevant. We can then potentially bathe their plica in steroid, which can decrease the inflammation, the thickening enough, hopefully to break the cycle and then with good quality rehab that they're nice and strong and their patella is sitting well, hopefully they will see the back of it. If they have the local anaesthetic, maybe the
steroid, and the diagnosis is made and confirmed, but it comes back, then they might be one of the few candidates that needs the plica resected. And I certainly, fairly recently, had an ultramarathon runner who was performing at national level and the surgeon laughed with me and said, "Oh, you know, normally I wouldn't touch a plica and particularly in an elite athlete, but I really do think, actually, it might be relevant, and can you have a look?" And I agreed. And she had the surgery, and she was great. So, there are cases where it's relevant, but it is few and far between.
Rehabilitation
Plica resection if necessary
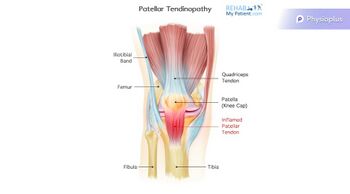
Patella Tendinopathy[edit | edit source]
Treated with heavy resistance loading or eccentric decline loading
| Patella Tendinopathy | Patellofemoral Pain | |
|---|---|---|
| Aggravating Factors | Being still
Early morning |
Being still if knee at end of range flexion |
| Description of Pain | Pinpoint to proximal tendon | Vague |
| Effect of Excercise | Pain decreases as tendon warms up | Worsens with repetitive load |
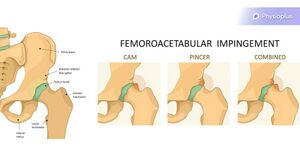
FAI[edit | edit source]
Has been known to refer pain to the anteromedial knee
looking at their pain response, particularly with the quadrant - flexion, adduction, internal rotation - those kinds of movements. Does it reproduce their knee pain?
Assessment Tools[edit | edit source]
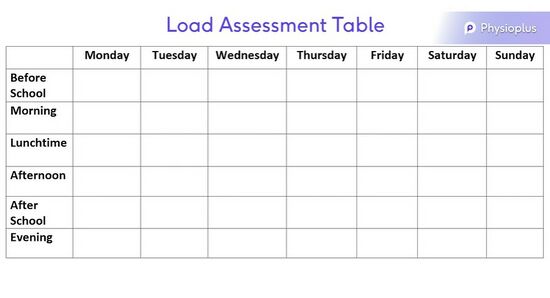
Load Assessment Table for Growth Tracking - Track volume of exercise in a week