Understanding Red Flags in Patellofemoral Pain: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 25: | Line 25: | ||
inflammation and elevation of the growth plates in the tibial tuberosity, so the proximal tibia | inflammation and elevation of the growth plates in the tibial tuberosity, so the proximal tibia | ||
Can be confirmed on MRI to show level of | Can be confirmed on MRI to show level of inflammation | ||
Pain worsen to a point that it can prevent any participation in sport | Pain worsen to a point that it can prevent any participation in sport | ||
| Line 81: | Line 81: | ||
Osteochondritis Dissecans | Osteochondritis Dissecans | ||
==== Osteochondritis Dissecans ==== | ==== Osteochondritis Dissecans/Osteochondral Defect ==== | ||
cartilage and some of the subchondral bone can break off and float in the joint, which irritates the synovium, which in turn causes the effusion | cartilage and some of the subchondral bone can break off and float in the joint, which irritates the synovium, which in turn causes the effusion | ||
Autoimmune disease red flags: | |||
Multiple joint involvement | Multiple joint involvement | ||
| Line 98: | Line 98: | ||
Recent Illness | Recent Illness | ||
==== | Osteochondritis Dissecans Treatment: | ||
Possible debridement/knee washed out | |||
Review, ideally, the OCDs, the osteochondral defects, with MRI. And what they're looking for there is how stable are the margins of the osteochondral defect and where are they? Are they in a very weight-bearing zone or not? And with respect to the stability, the margins, I think about it a bit like a divot on a golf course. So, sometimes you might have a really clean bit of grass, the soil has been removed, and it's not all crumbling in. So, that's a stable situation. And then we might have a divot on a golf course where the grass and soil has been removed and the soil is just crumbling in, and that would be an unstable OCD and there | |||
Possible surgical resection ly they might need to resect back to a stable margin. | |||
Monitor bone oedema around these defects, which over time, serially scanned, you're looking for those to decrease. So, from a | |||
physiotherapy point of view, we're looking at load management. Understanding, for example, in the patellofemoral joint if we've got a trochlear OCD, then we're not going to be wanting to do lots of deep loaded flexion, for example. So, message there without a doubt, do not sit on a child with an effused knee | |||
Always refer a child with a knee effusion for further investigations to establish an underlying cause | |||
==== Slipped Capital Femoral Epiphysis ==== | |||
==== Others ==== | ==== Others ==== | ||
Systemic Auto-Immune Disease | Less common but more serious:Systemic Auto-Immune Disease | ||
Slipped Epiphysis | Slipped Epiphysis | ||
| Line 113: | Line 127: | ||
Primary Bone Tumour | Primary Bone Tumour | ||
== Assessment Tools == | Red Flags | ||
Night pain | |||
Weight loss | |||
Malaise | |||
== PCL Rupture ==== Assessment Tools == | |||
Load Assessment Table for Growth Tracking - Track volume of exercise in a week | Load Assessment Table for Growth Tracking - Track volume of exercise in a week | ||
Revision as of 07:38, 15 August 2022
Top Contributors - Carin Hunter, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Why do we need to know red flags?
Safety
Directing patients to the right place
If there has been trauma to the knee - always make sure the correct imaging/investigations have been done.
Non-Traumatic Masquerading Conditions[edit | edit source]
Young people[edit | edit source]
Osgood Schlatters[edit | edit source]
11-15 years olds
prevalent in kids that do lots of quads dominant sports, so running, and kicking and jumping
obvious bump at the tibial tubercle
Pain specific to tibial tubercle
inflammation and elevation of the growth plates in the tibial tuberosity, so the proximal tibia
Can be confirmed on MRI to show level of inflammation
Pain worsen to a point that it can prevent any participation in sport
Treatment:Education
Activity modification - eliminate least fav sport, change playing position to a less active one to decrease load
NSAIDS
Ice Massage(Symptomatic relief)
Address overload
extrinsic
load management of sport
footwear
landing technique
intrinsic factors
muscle length
muscle strength
Sinding-Larsen-Johansson Disease[edit | edit source]
inflammation at the growth plate of the distal pole of the patella
most likely to be seen at times of aggressive growth/growth spurts
treatment tactics that I ask parents to do is to track growth because they're more likely to manage it well at times of aggressive growth with their activity modification.
Pain worsen to a point that it can prevent any participation in sport
Treatment:activity modification
Knee Effusion[edit | edit source]
A child should not have a knee effusion
Effusion very often leads to patellofemoral pain
A knee effusion in a child should always be investigated
Possible Causes:
systemic autoimmune disease, juvenile arthritis
infective arthritis
Osteochondritis Dissecans
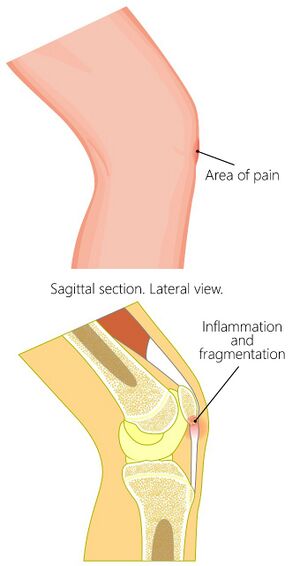
Osteochondritis Dissecans/Osteochondral Defect[edit | edit source]
cartilage and some of the subchondral bone can break off and float in the joint, which irritates the synovium, which in turn causes the effusion
Autoimmune disease red flags:
Multiple joint involvement
Joint was stiff on waking
Fatigue
Infective arthritis red flags:
Temperature
Recent Illness
Osteochondritis Dissecans Treatment:
Possible debridement/knee washed out
Review, ideally, the OCDs, the osteochondral defects, with MRI. And what they're looking for there is how stable are the margins of the osteochondral defect and where are they? Are they in a very weight-bearing zone or not? And with respect to the stability, the margins, I think about it a bit like a divot on a golf course. So, sometimes you might have a really clean bit of grass, the soil has been removed, and it's not all crumbling in. So, that's a stable situation. And then we might have a divot on a golf course where the grass and soil has been removed and the soil is just crumbling in, and that would be an unstable OCD and there
Possible surgical resection ly they might need to resect back to a stable margin.
Monitor bone oedema around these defects, which over time, serially scanned, you're looking for those to decrease. So, from a
physiotherapy point of view, we're looking at load management. Understanding, for example, in the patellofemoral joint if we've got a trochlear OCD, then we're not going to be wanting to do lots of deep loaded flexion, for example. So, message there without a doubt, do not sit on a child with an effused knee
Always refer a child with a knee effusion for further investigations to establish an underlying cause
Slipped Capital Femoral Epiphysis[edit | edit source]
Others[edit | edit source]
Less common but more serious:Systemic Auto-Immune Disease
Slipped Epiphysis
FAI
Leukaemia
Metastatic Neuroblastoma
Primary Bone Tumour
Red Flags
Night pain
Weight loss
Malaise
PCL Rupture ==== Assessment Tools[edit | edit source]
Load Assessment Table for Growth Tracking - Track volume of exercise in a week