Ultrasound in Wound Healing: Difference between revisions
No edit summary |
No edit summary |
||
| Line 47: | Line 47: | ||
The aim is to produce a thermal effect for vasodilation and increased tissue oxygen levels.<br>The ultrasound head should be 1.5 or 2 times the size of the area to be treated. Aqueous medium is applied to the transducer and is moved in a slow circular motion around the treated area. 2-3 minutes completes per zone, 3 times per week.<br> | The aim is to produce a thermal effect for vasodilation and increased tissue oxygen levels.<br>The ultrasound head should be 1.5 or 2 times the size of the area to be treated. Aqueous medium is applied to the transducer and is moved in a slow circular motion around the treated area. 2-3 minutes completes per zone, 3 times per week.<br> | ||
== Application to Wound == | == Application to Wound == | ||
'''Parameters''' | '''Parameters''' | ||
20% duty cycle, 3MHz with intensity at 0.3-0.5 W/cm squared. | 20% duty cycle, 3MHz with intensity at 0.3-0.5 W/cm squared. | ||
The aim is to stimulate protein synthesis and increase cell proliferation. | The aim is to stimulate protein synthesis and increase cell proliferation. | ||
The dressings should be removed and wound should be debrided of dressing residue and foreign debris. Apply a hydrogel sheet over the wound, removing any air bubbles. | The dressings should be removed and wound should be debrided of dressing residue and foreign debris. Apply a hydrogel sheet over the wound, removing any air bubbles. | ||
[[Image:Hydrogel.jpg|thumb|left]]The ultrasound head should be 1.5 or 2 times the size of the treated area. If the area is large, treatment can be completed in sections with 1-2 minutes per zone. Ultrasound medium is applied to the transducer and in contact with the hydrogel sheet. <br>Acute wounds can be treated 1-2 times per day | [[Image:Hydrogel.jpg|thumb|left]]The ultrasound head should be 1.5 or 2 times the size of the treated area. If the area is large, treatment can be completed in sections with 1-2 minutes per zone. Ultrasound medium is applied to the transducer and in contact with the hydrogel sheet. <br>Acute wounds can be treated 1-2 times per day and then continued 2-3 times per week.<br> | ||
== Application to restart inflammatory phase in chronic wounds == | == Application to restart inflammatory phase in chronic wounds == | ||
Revision as of 22:56, 15 March 2015
Ultrasound Therapy for Wound Healing
Ultrasound[edit | edit source]
Therapeutic ultrasound is utilized by physical therapists to deliver a high-frequency mechanical vibration to facilitate healing at a cellular level. The application of ultrasound can be helpful in the reduction of inflammation, reducing pain and the healing of injuries and wounds.
Effects on the Phases of Wound Healing [edit | edit source]
[edit | edit source]
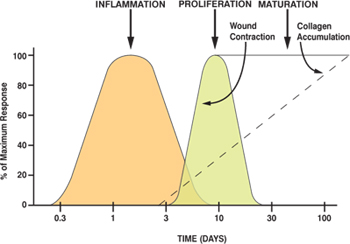
Inflammatory Phase[edit | edit source]
The normal acute inflammatory response occurs after the initial clotting response with vasodilation and invasion of white blood cells to the area which in return, initiated repair (Sussman & Bates-Jensen, 2012). Within the white blood cells are mast cells which undergo degranulation and release histamine and other chemical mediators to form a coagulated gel in the injured area.
When ultrasound is applied in this phase, it enhances the degranulation of mast cells resulting in the release of histamine and other mediators that attract fibroblasts and endothelial cells to the injured area. This will later result in the formation of collagen-containing vascular granulation tissue ((Sussman & Bates-Jensen, 2012). Early intervention with ultrasound should result in an accelerated acute inflammatory phase, moving to a more quick entry into the proliferative phase and improving comfort of the patient in this phase.
Proliferative Phase[edit | edit source]
In this phase, Ultrasound stimulates fibroblast migration and proliferation to secrete collagen, improving tensile strength of the healing connective tissues. The production of vascular endothelial growth factor and angiogenesis are also promoted by the application of ultrasound in this phase (Sussman & Bates-Jensen, 2012). In the end, there is an accelerated process of wound contraction as ultrasound may cause the early development of Myofibroblasts. Low-intensity, non-thermal ultrasound within 72 hours following an injury can promote wound contraction which should result in a smaller scar ((Sussman & Bates-Jensen, 2012).
Epithelialization phase[edit | edit source]
Application of Ultrasound to the peri-wound area stimulates the release of growth factors needed to regenerate epithelial cells, further protecting the body from infection and reinstate skin integrity (Sussman & Bates-Jensen, 2012).
Maturation or Remodeling Phase[edit | edit source]
The response to ultrasound in this stage is dependent on if therapy was initiated in the inflammatory phase. Application of thermal ultrasound during this phase affects the collagen extensibility and enzyme activity and therefore also improves tensile strength of the healing tissue (Sussman & Bates-Jensen, 2012).
Suggested Frequencies[edit | edit source]
Dermal Wounds – 3MHz
Deep lacerations or Periwound Skin – 1Mhz
Application to Periwound Tissue[edit | edit source]
Parameters
1MHz, continuous mode with intensity at 1 – 1.5 W/ cm squared.
The aim is to produce a thermal effect for vasodilation and increased tissue oxygen levels.
The ultrasound head should be 1.5 or 2 times the size of the area to be treated. Aqueous medium is applied to the transducer and is moved in a slow circular motion around the treated area. 2-3 minutes completes per zone, 3 times per week.
Application to Wound[edit | edit source]
Parameters
20% duty cycle, 3MHz with intensity at 0.3-0.5 W/cm squared.
The aim is to stimulate protein synthesis and increase cell proliferation.
The dressings should be removed and wound should be debrided of dressing residue and foreign debris. Apply a hydrogel sheet over the wound, removing any air bubbles.
The ultrasound head should be 1.5 or 2 times the size of the treated area. If the area is large, treatment can be completed in sections with 1-2 minutes per zone. Ultrasound medium is applied to the transducer and in contact with the hydrogel sheet.
Acute wounds can be treated 1-2 times per day and then continued 2-3 times per week.
Application to restart inflammatory phase in chronic wounds[edit | edit source]
Parameters
1Mhz, 0.5 W/cm squared at 20% duty cycle applied to peri-wound area
The ultrasound head should be 1.5 or 2 times the size of the area to be treated. Aqueous medium is applied to the transducer and is moved in a slow circular motion around the treated area. 2-3 minutes completes per zone, 3 times per week.
Precautions and Contraindications[edit | edit source]
• Contraindicated over eyes, genital areas, abdominal area and exposed neural tissue
• Should be avoided in cases of thromboembolic diseases
• Avoided in patients with pacemakers
• Precautions should be taken with sensory impairments
• Ultrasound should be terminated if there is increased pain
What Researchers Say[edit | edit source]
Ernst (1998) completed a systematic review of 5 studies that utilized ultrasound therapy for patients with leg ulcers, chronic leg <g class="gr_ gr_155 gr-alert gr_gramm Punctuation only-ins replaceWithoutSep" id="155" data-gr-id="155">ulcers</g> and pressure sores. They used low-dose (low intensity) ultrasound which proved to be effective as an adjunct to promote wound healing. This has been also confirmed by other systematic reviews.
Kavros, Miller and Hanna (2007) evaluated the role of noncontact low-intensity, low-frequency ultrasound in the treatment of a non-healing leg and foot ulcer with chronic limb ischemia. Ultrasound therapy was administered 3 times per week for 5 minutes, each treatment. Results showed an increase in the rate of healing when coupled with standard wound care.
References[edit | edit source]
Al‐Kurdi, D., Bell‐Syer, S. E., & Flemming, K. (2008). Therapeutic ultrasound for venous leg ulcers. The Cochrane Library.
Baker, K., Robertson, V., & Duck, F. (2010). A Review of Therapeutic Ultrasound. Journal Of Womenʼs Health Physical Therapy, 34(3), 111-118. doi:10.1097/jwh.0b013e31820089ba
Ernst E (1995). Ultrasound for cutaneous wound healing phlebology 10(1): 2-4.
Kavros, S. J., Miller, J. L., & Hanna, S. W. (2007). Treatment of ischemic wounds with noncontact, low-frequency ultrasound: the Mayo Clinic experience, 2004-2006. Advances in skin & wound care, 20(4), 221-2
Sussman, C., & Bates-Jensen, B. (2012). Wound care: A collaborative practice for manual health professionals. Fourth edition. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health.