Tularemia: Difference between revisions
Dana Collins (talk | contribs) No edit summary |
Dana Collins (talk | contribs) No edit summary |
||
| Line 11: | Line 11: | ||
== Prevalence == | == Prevalence == | ||
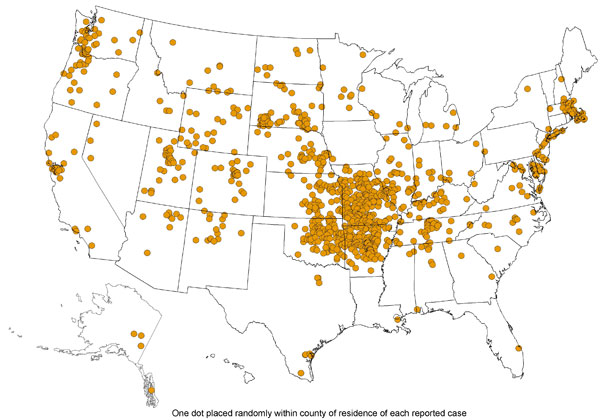
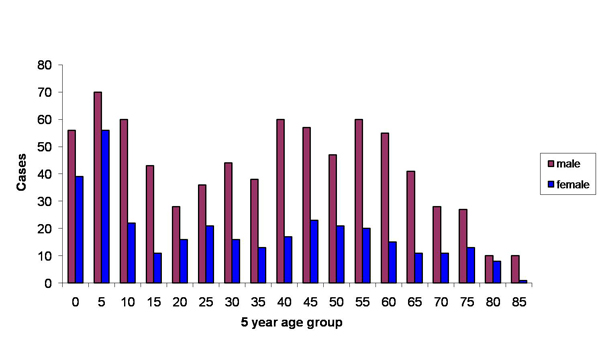
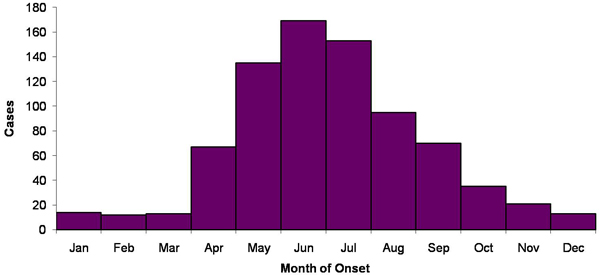
The prevalence of Tularemia in the United States depends on the geographical location and the time of year. During the spring and summer months (May-September), there is a rise in reported cases. South-Central, Pacific Northwest, and parts of the East Coast have the highest incidence of Tularemia. While the population most effected is young males 5-9 years old and those > 75 years old.<ref name="E">Hayes E, Marshall S, Dennis D. Tualremia--United States,1990-2000. www.cdc.gov/mmwr/preview/mmwrhtml/mm5109a1.htm. February 20, 2011.</ref><br> | The prevalence of Tularemia in the United States depends on the geographical location and the time of year. During the spring and summer months (May-September), there is a rise in reported cases. South-Central, Pacific Northwest, and parts of the East Coast have the highest incidence of Tularemia. While the population most effected is young males 5-9 years old and those > 75 years old.<ref name="E">Hayes E, Marshall S, Dennis D. Tualremia--United States,1990-2000. www.cdc.gov/mmwr/preview/mmwrhtml/mm5109a1.htm. February 20, 2011.</ref><br> | ||
[[Image:Tularemia_Image_1.jpg]]<br> | |||
[[Image:Tularemia_Image_2.jpg]]<br> | |||
[[Image:Tularemia_Image_3.jpg]]<br> | |||
The above images from: http://www.cdc.gov/tularemia/statistics/.<br> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Revision as of 00:44, 17 March 2011
Original Editors - Dana Collins from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Tularemia, named after the infectious gram-negative bacterium Francisella tularensis, is a zoonotic disease. A zoonotic disease is one that is spread from animal to human. This spread may be directly i.e. handling contaminated meat or through a carrier i.e. a tick. It is also known as “Ohara’s disease”, “rabbit fever”, “deer-fly fever”,[1] “market’s men disease”, “meat-cutter’s disease”, “glandular type of tick fever”, “water rat-trappers’ disease”. It is highly infectious, <10 organisms causing severe disease in both humans and animals.[2] There are 4 sub-types of the bacterium, the most common in the United States are Type A, tularenis, and Type B, holarctica. It is on the Center for Disease Control’s list of bioterroism threats.
Prevalence[edit | edit source]
The prevalence of Tularemia in the United States depends on the geographical location and the time of year. During the spring and summer months (May-September), there is a rise in reported cases. South-Central, Pacific Northwest, and parts of the East Coast have the highest incidence of Tularemia. While the population most effected is young males 5-9 years old and those > 75 years old.[3]
The above images from: http://www.cdc.gov/tularemia/statistics/.
Characteristics/Clinical Presentation[edit | edit source]
add text here
Associated Co-morbidities[edit | edit source]
add text here
Medications[edit | edit source]
add text here
Diagnostic Tests/Lab Tests/Lab Values[4][edit | edit source]
There are numerous ways to test for F. tularensis:
• Gold Standard: Bacteriologic Culture[2]
• Most Common: Serology[2]
• PCR of sample ulcer
• Direct Stains
• Blood Culture
• Direct Fluorescent Antibody Stain
• Slide Agglutination
• Antimicrobial Susceptibility
• Biochemical Identification
• Enviornmental Specimen Evaluation
• Chest X-ray
Etiology/Causes[edit | edit source]
add text here
Systemic Involvement[edit | edit source]
add text here
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1xy-1_DjTDyg-yCxbAyHc37zdTAK3fTd5nhb8khoKmGON3zYjN|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ Wilson M, Lountzis N, Ferringer T. Zoonoses of dermatologic interest. Dermatologic Therapy. 2009;22:367-378. http://onlinelibrary.wiley.com/doi/10.1111/j.1529-8019.2009.01248.x/abstract. Accessed February 2011.
- ↑ 2.0 2.1 2.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedF - ↑ Hayes E, Marshall S, Dennis D. Tualremia--United States,1990-2000. www.cdc.gov/mmwr/preview/mmwrhtml/mm5109a1.htm. February 20, 2011.
- ↑ CIDRAP. Tularemia: Current, comprehensive information on pathogenesis, microbiology, epidemiology, diagnosis, treatment, and prophylaxis. http://www.cidrap.umn.edu/cidrap/content/bt/tularemia/biofacts/tularemiafactsheet.html. Updated March 16, 2010. Accessed February 2011.