Total Shoulder Arthroplasty
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Search Databases: Cochrane Library, CINAHL PLUS with full text, Medline with full text, Proquest, Google Scholar. Search dates: 10/25/10-11/13/10.
Search terms: Total Shoulder Arthroplasty, Shoulder Arthroplasty, Shoulder Surgery AND Rehab, Reverse Shoulder Arthroplasty, Shoulder Replacement, Shoulder surgery AND complications
Definition/Description[edit | edit source]
Total shoulder arthroplasty, or TSA, is a procedure used to replace the diseased or damaged ball and socket joint of the shoulder with a prosthesis made of polyethylene and metal components. The “ball” is the proximal head of the humerus and the “socket” refers to the concave depression of the scapula referred to as the glenoid.[1][2]
A reverse total shoulder arthroplasty, or rTSA, refers to a similar procedure in which the prosthetic ball and socket that make up the joint are reversed to treat certain complex shoulder problems.[3][4][5]
Epidemiology /Etiology[edit | edit source]
The first record of shoulder arthroplasty was performed in 1894 by the French surgeon, Jean Pean.[2] The original implant consisted of a platinum and rubber implant for the glenohumeral joint. Charles Neer is credited with the advancement of modern TSA, developing more modern prostheses for surgical procedures beginning in the 1950’s.[2][5][1]
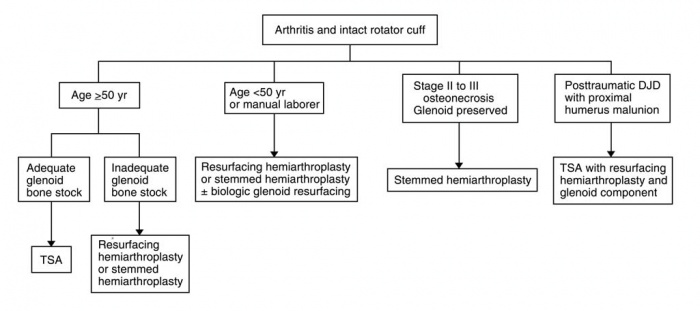
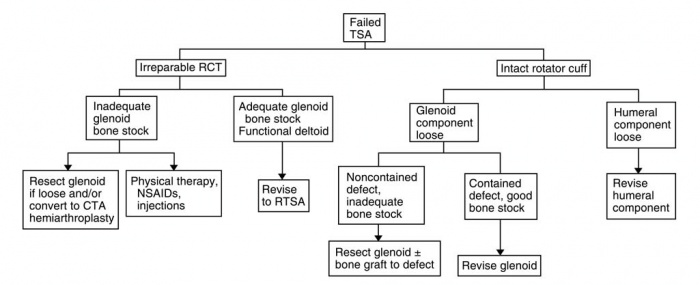
There are approximately 23,000 shoulder replacement surgeries performed each year compared to 400,000 knee replacements, and 343,000 hip replacements.[6] This is largely due to the relative complexity of the anatomy and biomechanics of the shoulder joint. Because of the complexity of the region, there are multiple variations in prostheses and surgical procedures that are performed depending on the tissues that are implicated. Since Neer’s initial design in 1951, more than 70 different shoulder systems have been designed for shoulder reconstruction arthroplasty.[7] The earliest shoulder replacement procedures were limited to treating proximal humeral fractures, but current implications for shoulder arthroplasty include: primary osteoarthritis, posttraumatic arthritis, inflammatory arthritis, osteonecrosis of the humeral head and neck, pseudoparesis caused by rotator cuff deficiency, and previous failed shoulder arthroplasty. Understanding the different prosthetic options and indications for each impairment is important for all practitioners in the health care continuum. Algorithms have been developed to assure each patient is matched with the correct procedure and fitted with the right prosthetic option. Below are examples from Wiater and Fabing detailing the method for selecting the proper procedure.
Medical Management (current best evidence)[edit | edit source]
There are 3 main categories of shoulder reconstruction surgery: Hemiarthroplasty, total shoulder arthroplasty (TSA), and reverse total shoulder arthroplasty (rTSA).
Hemiarthroplasty
Hemiarthroplasty involves the humeral articular surface being replaced with a stemmed humeral component coupled with a prosthetic humeral head component. Hemiarthroplasty is indicated when either the humerus alone is implicated, or the glenoid is not fit to support a prosthetic. Indications include: arthritic conditions involving both the humeral head and osteonecrosis without glenoid involvement, however the most common indication for this procedure are severe fractures of the proximal humerus. An optional technique is a resurfacing hemiarthroplasty that does not require a stemmed component inserted into the long shaft of the humerus, rather the humeral head is simply resurfaced with a prosthetic component. This procedure has proven effective at managing arthritic conditions of the shoulder and is favorable for young, athletic patients with worries of loosening prosthetic components.[7][8]
Total Shoulder Arthroplasty
In TSA, the current components of the glenoid are either a pegged or keeled high-molecular weight polyethylene cemented component.[2] These become fixated by allowing bony ingrowth through the pourous ends of the component. For some shoulders with inferior bone quality, metal backing is used to increase the durability and fixation of the polyethylene component.[2][5] Controversy stills exists as to the stress effects metal backing can potentially cause on the joint.
The humeral component consists of the artificial metal humeral head attached to a metaphyseal stem that is either fully cemented, proximally cemented, of press-fit into the humeral shaft.[2][5] Harris et al. Found no difference in comparing micromotion between fully and proximally cemented techniques.[9]
Indications for TSA include: osteoarthritis, inflammatory arthritis, osteonecrosis involving the glenoid, and posttraumatic degenerative joint disease. The patient must also have an intact rotator cuff complex, or else other prosthetic techniques would be implicated. A prospective study by Barrett et al. found that 47 or 50 patients treated with TSA had significant decreases in pain and increases in range of motion compared to presurgical measurements.[10] A 2004 study by Collins et al. compared conventional TSA with Hemiarthroplasty and although both groups showed significant decreases in pain from pretreatment measurements, the TSA group demonstrated more increases in ROM.[11]
There are several variations to the TSA procedure. Resurfacing total shoulder arthroplasty involves replacing the deteriorated bone surface of the humeral head and does not require a stemmed component inserted into the long axis of the humerus. Because there is no stemmed humeral component, this technique is becoming a popular option. Levy and Copeland compared cementless resurfacing TSA’s with standard stemmed prostheses and found comparable results.[12] An alternative for the active individual is the TSA with Biologic Glenoid Resurfacing. This procedure involves a TSA humeral component coupled with glenoid resurfacing using a form of biologic tissue (fascia lata, anterior shoulder capsule, Achilles tendon, menisci) and studies have shown comparable results to conventional TSA.
Comparison of published studies show some disagreement whether TSA is a superior treatment to hemiarthroplasty for patients with primary osteoarthritis. A meta-analysis by Radnay et al. found significantly greater pain relief, forward elevation, gain in forward elevation, gain in external rotation, and patient satisfaction with TSA compared with hemiarthroplasty in a total of 1,952 patients.[13]
Reverse Total Shoulder Arthroplasty
rTSA involves a stemmed-humeral component containing a polyethylene humerosocket replacing the humeral head, and a highly polished metal ball known as a glenosphere replacing the socket, or glenoid. One can think of this as the “ball and socket” components being switched. This allows for better fixation of the prosthetic parts and increased stability of the joint. An rTSA currently is indicated for patients suffering from osteoarthritis or compound fractures of the humerus, in conjunction with a deficiency of the rotator cuff complex. Matsen et al. also states that an rTSA should be considered for patients whose shoulder problems cannot be managed using a conventional TSA (Matsen 2006). Several features make the rTSA more compatible for certain patient populations. The deep concavity of the humeral articular component, as well as the simplicity of the glenoid component, allow for better fixation of the prosthesis and fewer problems with component loosening. Compensation for rotator cuff dysfunction is made with the rTSA that typically is left unmanaged in conventional TSA. Several long term studies have been done on the procedure with positive results.[14][3] Early studies found both high complication and revision rates, 50 and 60 percent respectively, however a 2007 retrospective study by Wall et al. found a complication rate of only 19%. The authors of this study also suggest that rTSA can be used for a larger population of patients receiving a shoulder replacement, not just those with rotator cuff arthropathy. Early evidence suggests that RTSA is a viable option for certain patient populations with more research needed in comparisons with TSA and Hemiarthroplasty.
Complications[edit | edit source]
add text here
Post Surgical Presentation/Precautions[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Expected Outcomes[edit | edit source]
Many factors have an impact on the outcomes of the postsurgical patient; they include preoperative health status, preoperative shoulder function, age, gender, and social environment (Wilcox 2005). Longevity of the prosthesis, strength, ROM, patient-reported surveys and patient reports of pain compared to preoperative measures are commonly used as outcome measures when studies are performed. Some studies use the Simple Shoulder Test (SST) to track patient progress. Since there is no universally accepted functional outcome measure for TSA it makes it difficult to compare outcomes across studies. The etiological cause for TSA appears to be the greatest indicator for prognosticating success rates postoperatively.
- Osteoarthritis: TSA is the most successful option for pain relief and restoration of function in patients with OA who have failed conservative treatment(Wilcox). It also has the largest success rates with most series reporting 90%-95% of patients to be eventually pain-free post surgery. Most of these patients should expect to achieve acceptable functional ROM, defined as 140° of forward flexion.
- Rheumatoid Arthritis: Although patients with RA might have more complicated surgical procedures, patients with advanced RA can benefit greatly from TSA(Wilcox). A study by Stewart and Kelly concluded that TSA provided reliable long term pain relief with ROM and functional improvements, although outcomes were mainly focused on surgical results such as component loosening (Stewart 97). A comparable increase in ROM is not to be expected with RA patients compared to OA and rehab should focus on performing functional activities below 90°, as they may not achieve full overhead motion.
- Rotator Cuff Arthroplasty: ROM and functional outcomes of patients with cuff tear arthropathy following TSA are also typically less than patients undergoing TSA for Osteoarthritis. Most of these patients do not achieve forward flexion greater than 90°(Wilcox). Generally pain relief is still achieved but with a high rate of component loosening. It has been recommended by several studies that these patients would be better suited for a reverse total shoulder arthroplasty with loss of rotator cuff function.
- Proximal Humeral Fractures: Due to the variability in humeral fractures, it is difficult to establish baseline functional outcome measures for this subset of patients. Various studies have found forward flexion to be between 92° and 102° postoperatively, with a significant decrease in pain. It is important to also consider the underlying fracture type, as this may dictate the following course of rehab.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
Total shoulder arthroplasty has become a viable option for patients with advanced shoulder dysfunction due to a variety of different etiologies. This procedure, along with the newer reverse total shoulder arthroplasty, can help relieve pain and increase function in patients when indicated. Postsurgical rehabiliation for these patients is key to obtaining successful outcomes. There is currently limited evidence and guidelines regarding postsurgical rehabilitation, therefore each patient should be evaluated on a case by case basis in strong collaboration with the patient’s other healthcare providers.
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
- ↑ 1.0 1.1 Wilcox R, Arslanian L, Millett P. Rehabilitation following total shoulder arthroplasty. The Journal Of Orthopaedic And Sports Physical Therapy [serial online]. December 2005;35(12):821-836.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Gregory T, Hansen U, Emery R, Augereau B, Amis A. Developments in shoulder arthroplasty. Proceedings Of The Institution Of Mechanical Engineers. Part H, Journal Of Engineering In Medicine [serial online]. January 2007;221(1):87-96.
- ↑ 3.0 3.1 Matsen Iii F, Boileau P, Walch G, Gerber C, Bicknell R. The reverse total shoulder arthroplasty. Instructional Course Lectures [serial online]. 2008;57:167-174.
- ↑ Boudreau S, Boudreau E, Higgins L, Wilcox R. Rehabilitation following reverse total shoulder arthroplasty. The Journal Of Orthopaedic And Sports Physical Therapy [serial online]. December 2007;37(12):734-743.
- ↑ 5.0 5.1 5.2 5.3 Keller J, Bak S, Bigliani L, Levine W. Glenoid replacement in total shoulder arthroplasty. Orthopedics [serial online]. March 2006;29(3):221-226.
- ↑ Shoulder Joint Replacement. American Academy of Orthopaedic Surgeons Web site. http://orthoinfo.aaos.org/topic.cfm?topic=A00094. Accessed November 11, 2010.
- ↑ 7.0 7.1 Wiater J, Fabing M. Shoulder arthroplasty: prosthetic options and indications. The Journal Of The American Academy Of Orthopaedic Surgeons [serial online]. July 2009;17(7):415-425.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedkelley - ↑ Harris, T.E., Jobe, C.M., Dai Q.G. Fixation of proximal humeral protheses and rotational micromotion. Journal of Shoulder and Elbow Surgery, 2000, 9(3), 205-210.
- ↑ Barrett W, Franklin J, Jackins S, Wyss C, Matsen F. Total shoulder arthroplasty. The Journal Of Bone And Joint Surgery. American Volume [serial online]. July 1987;69(6):865-872.
- ↑ Collins D, Harryman D, Wirth M. Shoulder arthroplasty for the treatment of inflammatory arthritis. The Journal Of Bone And Joint Surgery. American Volume [serial online]. November 2004;86-A(11):2489-2496.
- ↑ Levy O, Copeland SA: Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg 2004;13:266-271.
- ↑ Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS: Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: A systematic review. J Shoulder Elbow Surg 2007;16:396-402.
- ↑ Wall B, Nové-Josserand L, O'Connor D, Edwards T, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. The Journal Of Bone And Joint Surgery. American Volume [serial online]. July 2007;89(7):1476-1485.