Tibial Spine Fracture and Physical Therapy Protocol: Difference between revisions
Ruchi Desai (talk | contribs) No edit summary |
Ruchi Desai (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Ruchi Desai|Ruchi Desai ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Ruchi Desai|Ruchi Desai ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div>{{Condition}} | ||
== '''Introduction''' == | == '''Introduction''' == | ||
| Line 33: | Line 34: | ||
Standard imaging for tibial spine fractures include anteroposterior(AP) and lateral radiographs. Lateral radiographs should be true lateral radiographs which are particularly useful to assess degree of displacement and type of fracture. CT scan is useful in better assessment of fracture anatomy and degree of communition . MRI is useful in outlining the non-osseous concomitant injuries like meniscal injury, cartilage injury and other ligamentous injury. | Standard imaging for tibial spine fractures include anteroposterior(AP) and lateral radiographs. Lateral radiographs should be true lateral radiographs which are particularly useful to assess degree of displacement and type of fracture. CT scan is useful in better assessment of fracture anatomy and degree of communition . MRI is useful in outlining the non-osseous concomitant injuries like meniscal injury, cartilage injury and other ligamentous injury. | ||
[[File:Xray of right knee.jpg|center|thumb|350x350px|Right knee x-ray AP & Lateral view showing tibial spine avulsion fracture]] | [[File:Xray of right knee.jpg|center|thumb|350x350px|Right knee x-ray AP & Lateral view showing tibial spine avulsion fracture]] | ||
{{Condition}} | |||
=== Post-Operative Rehabilitation === | === Post-Operative Rehabilitation === | ||
Revision as of 06:07, 30 July 2023
Clinically Relevant Anatomy
[edit source]
add text here relating to clinically relevant anatomy of the condition
Mechanism of Injury / Pathological Process
[edit source]
add text here relating to the mechanism of injury and/or pathology of the condition
Clinical Presentation[edit source]
add text here relating to the clinical presentation of the condition
Diagnostic Procedures[edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit source]
add appropriate resources here
References[edit source]
Introduction[edit | edit source]
Tibial spine fracture (also called Tibial Eminence Fracture) is a break at the top of the tibia bone in the lower leg near the knee as a result of high amounts of tension placed upon the anterior cruciate ligament (ACL). This type of injury is most common in
1) children ages 8 to 14 years of age.
2) The incidence of these fractures is higher among adolescent girls due to their inherent skeletal immaturity.
3) It has also been proposed that injury occurs secondary to greater elasticity of ligaments in young people.
4) It can occur during a sporting event or direct trauma with a hyperextension injury causes an avulsion fracture occurring at the tibial eminence while the ACL is spared.
This type of force causes the ACL to pull on the tibial spine. Because the bones of children this age still have open growth plates, the ACL is stronger than the tibial spine and can pull away from the bone (avulse), causing a fracture.
Classification and Management for Tibial spine fracture[edit | edit source]
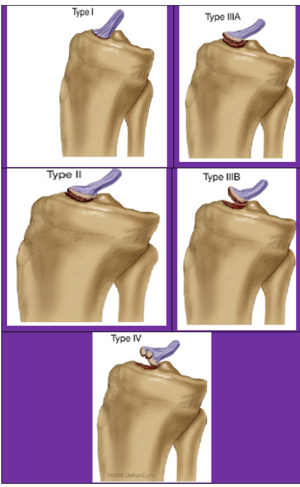
Under the Meyers and McKeever system (with modifications by Zaricznyj) injuries are classified into four main types:
- Type I is the minimal displacement of an avulsed fragment: This injury is treated conservatively by closed reduction, where the tibia is set into place without a surgical incision. and then the knee is immobilized in a long-leg cast or a fracture brace set at 10 to 20 degrees of knee flexion. Fixed flexion is recommended due to the fact that full extension may place excessive tension on the ACL and popliteal artery. Immobilization is then recommended for approximately 6 weeks depending on the patient's age, healing rate, and radiological findings.
- Type II classification is the displacement of half of the anterior third of the ACL insertion causing a posterior hinge: In most cases, closed reduction and immobilization may be attempted after aspirating knee haemarthrosis. Knee extension allows femoral condyles to reduce the displaced fragment. If acceptable reduction is achieved conservative management should be continued. If there is persistent superior displacement of the fragment seen in the x-ray then it is preferable to do arthroscopic reduction and internal fixation because chances for soft tissue entrapment at the fracture site are high.
- Type III is the complete separation of the avulsion site:
- Type IV was later added by Zariczynj to include comminuted fractures of the tibial spine: Type III & Type IV Treatment of displaced tibial spine avulsion fractures has evolved over a period of time from conservative management to open reduction and internal fixation to arthroscopic reduction and internal fixation. Various methods of fixation are used in the operative treatment of these fractures varying from retrograde wires /screws, antegrade screws, sutures, suture anchors, and a recently described suture bridge and K wire and tension band wiring technique.
Clinical Presentation[edit | edit source]
- Swelling
- Inability to weight bear
- Bruising
- Reduced knee range of movement (ROM)
- History of trauma
- Pain
Imaging[edit | edit source]
Standard imaging for tibial spine fractures include anteroposterior(AP) and lateral radiographs. Lateral radiographs should be true lateral radiographs which are particularly useful to assess degree of displacement and type of fracture. CT scan is useful in better assessment of fracture anatomy and degree of communition . MRI is useful in outlining the non-osseous concomitant injuries like meniscal injury, cartilage injury and other ligamentous injury.
Clinically Relevant Anatomy
[edit source]
add text here relating to clinically relevant anatomy of the condition
Mechanism of Injury / Pathological Process
[edit source]
add text here relating to the mechanism of injury and/or pathology of the condition
Clinical Presentation[edit source]
add text here relating to the clinical presentation of the condition
Diagnostic Procedures[edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit source]
add appropriate resources here
References[edit source]
Post-Operative Rehabilitation[edit | edit source]
Tibial eminence fractures have excellent prognosis. Previously, prolonged immobilization may lead to arthrofibrosis and a permanent loss of full extension. Therefore, earlier rehabilitation is crucial as it encourages a faster recovery and prevents the development of secondary complications. Rehabilitation is similar to ACL tear protocols and which has been described in below table.
| Goals | Brace | Weight Bearing | ROM | Exercises | |
|---|---|---|---|---|---|
| Phase -I
(0-6 Weeks) |
|
|
|
|
|
| Phase II: (Weeks 7-12) |
|
|
|
| |
| Phase III: (Weeks 13-18) |
| ||||
| Phase IV: (Months 5-6 )- Return to Sport |
|