The physiotherapist's role in the management of stress-related work absence in vocational rehabilitation
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Alix Maxwell, Lucy Camlin, Roxanne Sasha Ross, Laura Robertson, Kim Jackson, Hannah Radford, 127.0.0.1, Admin, Jane Hislop, Claire Knott and Amanda Ager
Introduction[edit | edit source]
The intention of this wiki is to provide an online self-directed learning tool on the topic of vocational rehabilitation for final year physiotherapy students and newly qualified physiotherapists. As this is such a wide topic, we have chosen to focus on the issue of stress-related work absence in vocational rehabilitation. There is a strong link between stress and sickness absence. Mental health conditions are increasingly prevalent and stress in the workplace is becoming more common with a 0.5% to 1.0% rise each year since 1992. Work-related stress is estimated to be the biggest occupational health problem in the UK, after musculoskeletal conditions such as back pain. Since 1995 the number of days lost to stress has more than doubled accounting for over 30% of all absences from work. This work absence is a major concern for both organisations and individuals and requires urgency in addressing it, (UK National Work Stress Network 2013;The Mental Health Foundation 2000).
By the end of this online resource you will have gained knowledge that will enable you to define stress and explain its impact on both the individual and those around them. You will also gain awareness of the policies, guidelines and recent research related to vocational rehabilitation. With the aid of this resource you will also gain understanding of the physiotherapists role in a vocational rehabilitation setting and more specifically the useful strategies employed by them in the management of stress.
To help aid the reader in their knowledge journey, a number of tasks in the form of quizzes, reflections, case studies and questions have been developed after each section in order to help the learner comprehend and consolidate the information read. Additionally, the resource provides the learner with an opportunity to further enhance their understanding the topics found in the resource through further reading material.
The material in this online resource has been developed in such a way that all styles of learning are accommodated. Diagrams and pictures for visual learners, videos for auditory learners and mind maps for kinaesthetic learners. If you don't know what learning style suits you best, click here to access the free online VARK Questionnaire.
The online resource will take approximately 10 hours to in total to complete. During these 10 hours your time will be spent navigating through the information provided in the various sections, accessing the suggested links and completing the recommended tasks.
Learning Outcomes[edit | edit source]
Aims
The aims of this wiki are:
1)To present a learning resource for Scottish final year physiotherapy students and newly qualified graduates which aims to develop their evidence-informed knowledge and understanding of vocational rehabilitation.
2)To present a learning resource for Scottish final year physiotherapy students and newly qualified graduates which aims to develop evidence-informed knowledge and understanding of vocational rehabilitation for stress-related work absence and promote in-depth exploration of the physiotherapist’s role in this area.
Learning Outcomes
Through completion of this wiki you will be able to:
1)Synthesise the main principles of vocational rehabilitation and critically analyse its role in achieving an optimum vocational outcome.
2)Explain the impact of stress and stress-related work absence on the individual.
3)Critically evaluate the role of the physiotherapist in the management of stress-related sickness absence/work loss in stress and how this relates to vocational rehabilitation settings.
4)Critically reflect on the challenges facing the physiotherapist in vocational rehabilitation.
These aims and learning outcomes have been derived using Blooms Taxonomy in order to ensure a learning resource at an adequate level for our target audience of final year physiotherapy students and newly qualified Band 5 Physiotherapists. Blooms Taxonomy, as shown below, aims to develop a higher level of thinking through a gradual pyramid approach of increasing difficulty (Adams 2015).
Learning Activity
Construct a mind map of what you already know about vocational rehabilitation and what you already know about stress.
Stress[edit | edit source]
Definition[edit | edit source]
There are numerous definitions of stress but no generally established medical definition, (Waddell & Burton 2006). However, according to the Health and Safety Executive (2012) stress is the negative response an individual exhibits when excessive pressure or demands are placed on them. Additionally, MIND (2015) define stress as a response to being put under pressure or situations that put an individual under pressure that if left unaddressed can result in psychological, physiological and behavioural changes to an individual.
Stress can be divided into two categories: Distress and Eustress. Distress is the negative response to stressors whereas eustress is the positive response to stressors. When an individual is distressed they experience negative psychological states such as frustration, low satisfaction and alienation that eventually result in work and social loss as well as negatively effects on their physical and mental well-being. Conversely, not all stress is bad for you. For instance when an individual experiences eustress they have positive psychological states such as meaningfulness, motivation, enthusiasm and participation that result in positive implications for both the individual's' well-being and performance.In additon to this, stress can have also have a positive effect on individuals when experienced in short intervals. Short-term exposure to stress has been found to boost the immune system, however, it is still important to be aware that long-term or chronic stress has an adverse effect on the immune system that eventually results in illness. Therefore, the important feature linked to stress is its chronic effect over time (Gardner and Fletcher 2006; Salleh 2008).
Predisposition to stress varies among individuals. An event that causes illness in one individual may not cause illness in another. Events are influenced by a number of background factors that lead to the manifestation of illness. Genetic vulnerability, coping style, type of personality and social support may all influence an individual’s susceptibility to stress. When faced with a problem, an individual assesses how serious the problem is and determines whether they have the necessary resources required to deal with the problem. If the seriousness of the problem outweighs the present resources, an individual may perceive themselves as being under stress. However, if the resources match or outweigh the problem an individual copes much better with the problem. It is this response system to situations that results in the differences in individual’s susceptibility to illness and overall well-being, (Salleh 2008).
Stress can be caused through various things happening in your life. It can result by either external factors in the environment or internal factors to the individual. Stress can also result as a consequence of real or perceived psychosocial pressures. Being under pressure, having too much or too little control over something or even worrying can trigger stress. Stressors are things that cause stress. Chronic stressors encountered in everyday life include work overload, financial difficulties or family problems. There are many other things that can cause stress but the aforementioned stressors are the ones most commonly encountered in everyday life. Although these stressors may occur independent from one another, most times they are interrelate. For instance, financial problems may have negative implications for both the individual and family. Additionally, research on the relationship between family problems and work have found that problems at home such as marital issues affect an individual's ability to perform adequately at work, conversely, pressure at work can affect an individual’s ability to function socially at home. Hence, even though a problem may root from work, family or finances, they may still have an overall impact in other areas of life and vice versa. With saying this it has been reported by employees that the single most stressful factor in their lives above finances and relationships was work, (MIND 2015; Salleh 2008; Bagwell 2000)
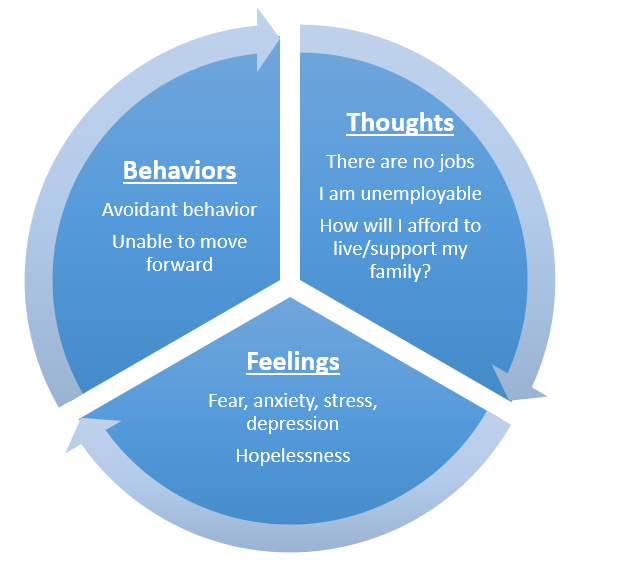
diagram*
Learning Activity
Using Rolfe's model of reflection, reflect on where stress is coming from in your life. What impact is it having on you and those around you? Are you coping with it? If so, how? If not, what's stopping you from coping with it?
Prevalence[edit | edit source]
Among the leading contributors to disease and disability burden globally are mental health problems, making 10.5% of the worldwide disease burden. In the United Kingdom, mental health problems are the single largest source of disability, accounting for 23% of total disease burdens (Kings Fund 2012).
About 1/4 of the general population will experience some kind of mental health problem in the course of a year. That is 1 in 4 British adults experiencing at least one mental disorder in any one year (John Cruddas 2014).
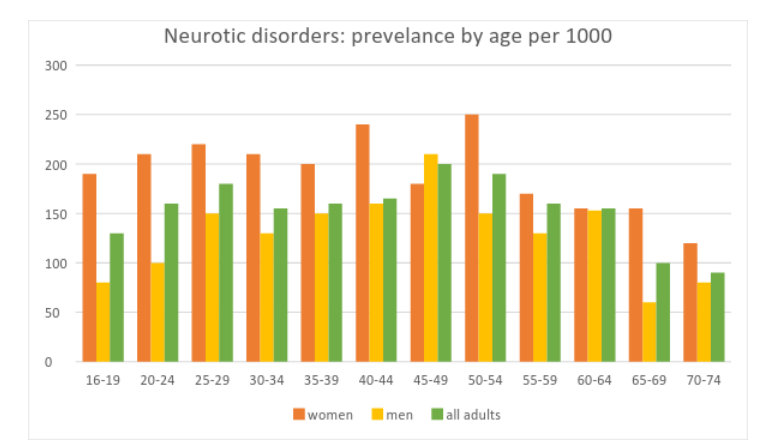
Women are more likely to be treated for mental health conditions than men, with 29% of women affected compared with 17% men.
Common mental health problems peak in middle age with 20-25% of people in the age group 45-54 years having a neurotic disorder. The figures fall as people grow older, with only 9.4% of people aged 70-74 years having a neurotic disorder compared with 16.4% of the general population.
About a third of the working population will have some mental symptoms at any one time in their lives. 1 in 3 British adults in the working age population will experience some kind of mental health problem. Of this, 1 in 6 people in the working age population will experience depression, anxiety or problems related to stress (UNISON 2015).
In 2013 the Labour Force Survey found that 131 million days were lost due to absence either as a result of sickness or injury. Mental health problems such as stress, anxiety and depression, musculoskeletal disorders and minor illnesses contributed to this number with 15 million, 31 million and 27 million, respectively.
According to the Chartered Institute of Personnel and Development (CIPD 2015) annual absent report:
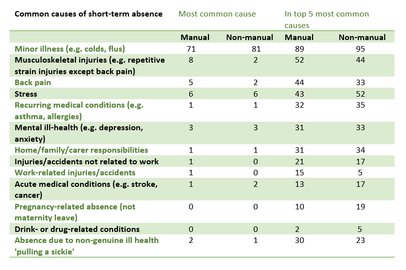
- The main causes of short term absence (≤ 4 weeks) were minor illness, musculoskeletal disorders and stress. Musculoskeletal disorders are more prevalent in manual workers and stress is more prevalent in non-manual works.
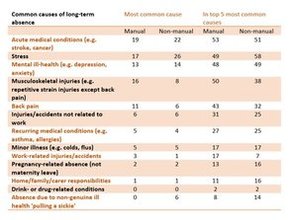
- The main causes of long term absence (≥ 4 weeks) were acute medical conditions, stress, mental ill health and musculoskeletal disorders.
- The median annual absence cost per employee across all organizations was £554. This cost varied in the different individual organizations, ranging from between £400 - £914, with the highest costs being in the public services.
According to the Labour Force Survey in 2013/14:
- The total number of cases of work-related stress, depression or anxiety was 487000 cases (39%) out of a total of 1241000 cases for all work-related illnesses.
- There was an estimated prevalence of 221000 male and 266000 female cases of work-related stress and an estimated incidence of 115000 male and 128000 female cases.
- The total number of working days lost due to work-related stress, depression or anxiety was 11.3 million, an average of 23 days per case of stress, depression or anxiety.
- Of the 11.3 million lost days, male workers accounted for approximately 5.4 million of those days while female worker accounted for approximately 5.9 million days
- The age 45-54 years had the highest incidence rate for all genders
Summary of findings from both mental health and stress statistics:
- The age group most affected is 45-54 years old.
- Women are more affected than men.
- The prevalence of stress higher in non-manual workers than in manual workers.
Although not a medical condition in itself, stress that is left unmanaged has been associated with stress-related mental and physical health problems such as anxiety, depression, cardiovascular disease and musculoskeletal pain, (CIPD 2011).
Learning Activity
Please complete this quiz based on the Prevalence section. Click here to access the quiz.
Impact[edit | edit source]
Although there is a collective opinion that mental health problems are caused by work, the relationship between the two is complex. While there is strong evidence that work is good for both mental and physical health, there is also evidence that mental well-being can be adversely affected by work.
Work-related stress may occur when individuals are faced with work demands or pressures they cannot cope with or have very little control over. The Health and Safety Executive (2015) defines stress as the negative response an individual exhibits when excessive pressure or demands are placed on them. Job stress is one of the top 10 work-related health problems and has increasingly been associated with the occurrence of mental health problems, cardiovascular disease and musculoskeletal disorder, (Waddell and Burton 2006; Habibi, Dehghan and Hassanzadeh 2014).
It is believed that the pathogenesis of physical disease is influenced by stress. Stress results in the production of adverse affective states which have a direct impact on the biological processes and behavioural patterns that predispose an individual to the risk of disease.
Stress can elicit the same responses that the body would produce if it were in physical danger. The body goes into ‘flight or fight’ mode, triggering the stress hormones adrenaline, noradrenaline and cortisol which in turn cause accelerated breathing, increased heart rate and dilation of blood vessels leading to increased blood pressure. In small amounts these responses are not harmful however when exposed to them for prolonged periods degenerative changes can occur within the body. Prolonged exposure to increased heart rate, blood pressure and stress hormones consequently lead to hypertension, arrhythmias, myocardial infarctions, or stroke (Torpy et al 2007). Furthermore, adrenaline can cause muscles to automatically contract and tense up in a biological response to stress as a means to protect the body from further harm. Prolonged exposure to muscle tension and muscle overuse causes the muscles to fatigue, tighten or degenerate, consequently increasing the risks of developing musculoskeletal disorders, (Lundberg 2002).
Stress can cause psychological changes that result in numerous adverse effects on an individual such as reduced competency, diminished initiative, reduced through flexibility, loss of accountability and reduced concern for both work colleagues and the organization as a whole. Additionally stress alters an individual’s physical state. The changes that occur in muscular structures can cause pain and discomfort resulting in an individual finding it difficult to sit at an office desk for the whole day or concentrate on work tasks due to lack of comfort. If stress is not managed immediately the physical and psychological effects of it that consequently lead to mental and physical changes can stop an individual from working at optimum capacity (Ongori and Agolla 2008).
diagram*
The conservation of an individual’s physical and mental health depends on their ability to adequately satisfy the demands they are confronted with. The greater an individual’s ability and control are over the exposed demands, the more effective the response produced will be. Conversely, when an individual is exposed to demands found to predominate their current knowledge and abilities they exhibit reduced capacity to work and perform their job adequately causing them to produce responses that are not effective (Negeliskii and Lautert 2011).
A major contributor to an organisation's profit and its existence is the amount of productivity delivered by employees. It is well established that excessive stress is detrimental to both an individual’s mental and physical well-being as well as productivity. With knowledge of this it can be recognised that stress is therefore a serious concern for organizations. Mental and physical changes can significantly influence an individual’s ability to work effectively which as a consequence can lead to increased absentee rates, increased turnover, sickness absence and work-related accidents. All of which negatively impact on an organization by decreasing its probability of success in competitive markets through reductions in overall productivity and service quality as well as increased expenditure on recruitment and selection costs as a result of turnover effects, (Ongori and Agolla 2008; Ekundayo 2014). Additionally, these factors cost the national economy an astounding amount of money annually through sickness absence which results in sick pay, staff turnover and loss of productivity. Furthermore, social welfare systems endure the costs of medical care and potential compensations in salary (Park 2007; Hauke et al 2011).
The problem of stress is clearly serious and urgent action is required to address it. Although there is a common view that mental health problems and stress are caused by work the relationship between the two is complex. While mental well-being can be affected adversely by work there is also strong evidence that work is good for both mental and physical health. Work has been found to provide individuals social status, social support, participation, a way to positively occupy time and personal achievement. All of which are at risk of being reduced or removed once an individual is out of work, (The Sainsbury Centre for Mental Health 2007; Waddell & Burton 2006). In addition to this, it has also been found that poorer physical and mental health have been linked to worklessness. From the evidence it can be concluded that work can be therapeutic in that it can transpose the negative health effects of being out of work. Hence through work targeted interventions like vocational rehabilitation, which aims to restore functional capacity for work, and physiotherapy, which also aims to restore functional ability as well as enhance an individual's well-being, individuals with health problems are helped to return to work. Although there is little to no evidence on the effectiveness of vocational rehabilitation interventions for stress management there is a strong association between work and good mental health and it is through this link vocational rehabilitation for stress management can be established, (Waddell, Burton & Kendall 2008).
Learning Activity
1. Define stress and work related stress.
2. We are aware that stress can result in musculoskeletal and cardiovascular problems. Name the physiological changes that occur to result in these problems.
3. What are the negative effects of stress on an individual's cognitive ability?
4. Why should stress be a serious concern for organizations?
Reflection for impact: Knowing that stress has adverse effects on both physical and mental wellbeing it is important that it is addressed. Have you ever encountered a patient who was suffering from work related stress? Did you address this? What did you do? What do you think you could have done/done differently?
Vocational Rehabilitation[edit | edit source]
The government policy ‘What Works, For Whom and When’ (2008) describes vocational rehabilitation as helping people with health problems stay at, return to and remain in work and this is unanimously the widespread definition. The Vocational Rehabilitation Association (2013) describes vocational rehab as any process which supports people with functional, physical, psychological, developmental, cognitive or emotional impairments to overcome obstacles to accessing, maintaining, or returning to work or another useful occupation. Vocational rehabilitation can be described as an idea or an approach, as much as it can an intervention (Connolly, 2011).
An effective vocational rehabilitation service should adopt a multi disciplinary approach, involving both healthcare professionals and employers. Vocational rehabilitation can also be practiced in a variety of settings. Primary healthcare settings can have a positive effect on occupational outcomes, either helping people with mild to moderate conditions return to work promptly or continue to offer treatment, education and help devise a return to work plan for a person who requires further assistance. Workplace interventions can also be highly beneficial. Many organisations have developed sickness absence and disability management programmes which efficiently cuts costs and enables return to work or the possibility of adapted working. More structured vocational rehabilitation programmes can also be followed for those with more severe cases. Vocational rehabilitation programmes can help to improve work outcomes for those in the early stages of claiming incapacity benefits. Incapacity benefit comes after a period of statutory sick pay and generally does not start until week 29 of sickness absence. However, many people are not employed at the time they start receiving benefits and they can often be faced with many barriers when trying to return to work. A person is likely to remain on benefits long term once they have been claiming for 1-2 years, meaning it is vital for vocational rehabilitation to play a part early on (Waddell et al 2008).
For many people these days, work is their key determinant of self worth, family income and esteem, as well as identity within the community and social fulfilment (Black 2008). Carol Black’s ‘Working for a healthier tomorrow’ review looking at the health of our working population suggests that the average UK employee is absent from work due to sickness for six days each year. Although these figures vary between workplaces, it is thought that these absences equate to an annual cost of around £598 per employer. Therefore, the estimated cost to the UK economy as a result of employee absence is around £100 billion annually- which is greater than the NHS annual budget (NICE 2009).
Healthcare understandably plays a vital role in Vocational rehabilitation, but ultimately, it is not effective without working closely alongside employers (Waddell et al 2008). There is strong supporting evidence that a proactive workplace approach to sickness and modified working is not only most effective but is also an effective cost saving method for the company, especially in larger enterprises.
Employers can have a key role in facilitating an employee’s early return to work following a sickness absence by having early, regular and sensitive contact during their leave, although around 40% or organisations have no sick leave management policy at all (Black 2008). This report also discusses the stigmas associated with absence from work due to disability and ill health, and states how this can also be a contributing factor in delaying a persons return to work. This is especially apparent in employees suffering from mental health conditions as organisations often fail to recognise their capabilities. There is significant evidence to suggest that the longer a person is absent from work due to ill health, the harder it is for them to make an effective return.
Although employment rates for those suffering from a disability or long term health condition are increasing, with employment rates in Britain being high when compared to most countries, 7% of the working population are still seeking incapacity benefits, while another 3% are off work sick at one given time (Black 2008).
Policies and Guidelines[edit | edit source]
Vocational Rehabilitation Policies[edit | edit source]
There are a number of policies and guidelines in relation to Vocational Rehab that provide a summary of key information which can be used to supplement your clinical practice.
Numerous documents have been established by The Scottish Government and the Department for Work and Pensions in order to support the importance and implementation of Vocational Rehabilitation.
Learning Activity
The following questions are based on the Healthy Working Lives: a Plan for Action document. You can access this document here.
Task:
1)Read Section 1 Background (pp.6-9)
2)Read Section 3 Building on Best Practice (pp 14-19) and answer the following questions:
- What services are currently available in Scotland? Are you aware of any that are not mentioned in the document?
- How do you feel these services affect you as a physiotherapist?
- Critically reflect on an experience you have had where knowledge of these policies may have changed your approach to your patient/treatment
3)Read Section 4 Supporting Employers (Pp. 20-25)
- Evaluate how the aims of this section will benefit you as a physiotherapist working in vocational rehabilitation
4)Read Section 5 Maximising Functional Capacity - Supporting Individuals (Pp. 26-30)
Learning Activity
Task 2 is based on the Building Capacity for Work: A UK framework for Vocational Rehabilitation document. Click here to access it.
Task:
1)Read the section titled ‘Vocational Rehabilitation: A Working Description’ where many varying definitions of vocational rehabilitation are listed and answer the following question. (Pp. 13-16)
- From your reading so far, what is your understanding of what vocational rehabilitation involves?
- Have you seen any examples of this whilst on placement?
2)Read the following section ‘Vocational Rehabilitation Drivers and Related Government Initiatives’ and have a think about the questions listed at the bottom of page 18. Can you relate these to any aspect of physiotherapy practice you’ve seen?
3)Read the final section on ‘Working to Achieve the Potential of Vocational Rehabilitation’ and critically reflect on the changes that Physiotherapists can make to get the most out of Vocational Rehabilitation.
Learning Activity
This task requires you to look at Vocational Rehabilitation: What Works, For Whom and When by Waddell, Burton and Kendall. Click here to access it.
Task:
1)Read 'What is Vocational Rehabilitation ' on pg. 10-12
- What is the main objective of vocational rehabilitation?
- Reflect on ways you can achieve this objective in your physiotherapy practice.
2)Read 'Delivery' on pg. 29-36
- What are the four types of vocational rehabilitation interventions?
- What is the main difference between primary health care interventions and 'structured' vocational rehabilitation interventions?
- Have you come across any of these interventions or any others not mentioned in the document whilst on clinical placement?
3)Read 'Timing and Coordination' on pg. 38-40
- When is vocational rehabilitation most effective?
- Why is the concept of early intervention central to vocational rehabilitation?
4)Read 'Healthcare, the workplace and vocational rehabilitation' on pg. 43-44
- What two things are necessary in order to produce effective return to work and vocational rehabilitation?
5)Read 'Evidence findings' on pg. 15-28
- From the mentioned health problems which of them is lacking Vocational Rehabilitation interventions?
- Which of the mentioned health problems is the largest growing cause of long term incapacity?
Learning Activity
For this task, please look at Co-ordinated, integrated and fit for purpose - A Delivery Framework for Adult Rehabilitation which can be accessed here.
http://www.gov.scot/resource/doc/166617/0045435.pdf
1)Read the foreword by Olivia Giles (pp 2-3).
- Critically reflect on this in relation to what you have already learned about vocational rehabilitation.
- Do you think anything else could be implemented to help people in similar situations to Olivia, looking to get back to what they did prior to illness?
2)Read section 3, paying particular attention to pages 14-16.
- What does this policy say about the definition of rehabilitation? Do you agree?
- What levels of management do you think are most appropriate within vocational rehabilitation? Why?
3)Read the section showing the future model for rehabilitation (pp 20-24).
4)Read pages 32-35 specific to vocational rehabilitation.
- Make notes on the key points you take from this.
Learning Activity
For this ask you should read Working for a Healthier Tomorrow by Dame Carol Black. You can access this document here. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/209782/hwwb-working-for-a-healthier-tomorrow.pdf
1)Read chapter 1, from pages 21-23
- What are the effects of ill-health and worklessness on families and children?
- Why is the health of the working age population important for everyone?
- This review identifies a new vision for the health of the working age population. What is this new vision and what are the three principle objectives associated with it?
2)Read chapter 3, pages 51-53 and 55-59
- What is the relationship between the workplace and an individuals health, safety and wellbeing?
- Why is an employees health of great concern to organizations?
- What strategies can be used to help support organizations in maintaining an employee's health, safety and wellbeing?
3)Read 'current care pathways and services' in chapter 5, also read pages 75-79
- Can you explain why early intervention for sickness absence is important?
- Reflect on incidences you have encountered on placement where early intervention would have been appropriate.
- What are the three key principles for effective early intervention?
- What is the 'fit for work' service and how does this service differ from the current service delivery.
4)Read chapter 7.
- What are the challenges faced by occupational health? Can you suggest any strategies for overcoming these barriers?
- What is the future vision for the working age health and what are the four fundamental principles that underpin it?
5)Read the Key challenges and recommendations for reform on pages 16-17
Vocational Rehabilitation Guidelines[edit | edit source]
NICE clinical guideline 19 (2009) provides a guideline on workplace health in long-term sickness absence and incapacity to work.
NICE recognized that employment enhances an individual’s health and wellbeing, conversely, it can also negatively impact on it with both employers and employees playing a part in an individual’s work absence. Hence this guideline was developed to help employers, employees, NHS professionals and other health professionals manage long term absence and incapacity.
The interventions recommended in this guideline aim to:
- decrease or prevent short-term sickness absence from becoming long-term
- aid employees currently on long-term sickness absence return to work
- decrease the number of recurring long-term sickness absences
- aid unemployed individuals or recipients of incapacity benefits return to work
For the purpose of this Wiki, as it is concentrating on management rather than assessment, recommendation 3 which is based on interventions and services is most appropriate. This recommendation is intended for employees experiencing long-term sickness absence or recurring short- or long-term sickness absence, particularly those with musculoskeletal disorders or mental health problems and it recommends:
- Coordinated and supported delivery of health, occupational or rehabilitation interventions/services
- arrangement for referrals to appropriate specialists or services including occupational health adviser,another professional specialising in occupational health, health and safety, rehabilitation, ergonomics or a physiotherapist.
- encouraging employees to contact occupational health service for any further advice and support required
- offering individuals with poor return to work prognosis one or more of the following ‘intensive’ interventions:
- referral to physiotherapy services or vocational rehabilitation
- counselling about a return to work
- workplace modifications
- offering individuals with good return to work prognosis short sessions of one or more of the following interventions:
- referral to a physiotherapist
- referral to psychological services
To read more on all 4 recommendations for assessment and management access:link
.
Realising work potential: Defining the Contribution of Allied Health Professionals to Vocational Rehabilitation in Mental Health Services: The Way Forward
Engaging in work and productive occupation has a positive influence on an individual's mental well-being. Hence, keeping people in work is a priority for the Scottish government and in 2010 they released the document ‘Realising Potential - An Action Plan for Allied Health Professionals in Mental Health’ which established a direct link between mental health and rehabilitation policy frameworks to get people back to work. They also identified early intervention as being key to this recovery.
This report is a follow up of Realising Potential and fulfils the pledge made by the Scottish government in realising potential to review current vocational rehabilitation models employed by Allied Healthcare Professionals in meeting the vocational needs of people with mental health problems and the provision of vocational rehabilitation across the 5 levels of healthcare.
This report identified the physiotherapists role in meeting the vocational needs of people with mental health problems as one that involves:
- assessing patients for appropriate walking aid and providing exercise programmes to improve confidence in regards to mobility issues for patients wishing to engage in volunteer role.
- joint working with occupational therapist in a community rehabilitation unit to improve fitness and promote weight loss in order to increase work tolerance.
- telephone based advice for occupational therapist supporting patients with heart disease to develop appropriate exercise routine to return patient to vocational role.
The report found that the best vocational rehabilitation model used by Allied Health Professionals is the Evidence Based Supported Employment and that the vocational rehabilitation service provision across the five levels of healthcare was mainly being provided in secondary and specialist mental health services. They suggested that Allied Healthcare Professionals should try reach those patients outside this level 3-4 spectrum to the ones that require earlier intervention.
From the findings of the reviewed vocational rehabilitation models and service provisions, 6 key principles were identified to help guide the development of AHP vocational rehabilitation service provisions and action points to help achieve these principles.
Task
Access the full report by clicking on the link and read the suggested sections in order to answer the following questions:
Qns 1 The report provides examples of models of Vocational Rehabilitation that AHPs have developed or are working in partnership with. The examples are specific to Scotland and therefore provide examples of vocational rehabilitation models used by NHS board areas within Scotland. Read the full list of Vocational rehabilitation models used in Scotland on pages 23-24. Have you come across any of these before on placement? Do you know of any other models apart from these ones mentioned in the document? Are you aware of what models are used in the rest of the UK?
Qns 2 The report identified the majority of work carried out by AHPs in mental health services occurs in secondary and specialists services . Through this identification they recommended that AHPs should consider trying to reach those patients outside this level 3-4 spectrum that require earlier intervention. with particular emphasises on the importance of enabling individuals to access services directly and easily before health issues become serious enough to require specialist, long-term care. Reflect on ways you might reach service users who require earlier intervention.
Qns 3
After reading the key principles and action plans found in the realising work potential document on pages 42-45, select two to four of these principles and reflect on how you would implement the proposed action plans into your clinical practice.
NICE clinical guideline 22 (2009) provides a guideline on mental wellbeing at work.
NICE recognized that work plays a vital part in promoting mental wellbeing but the work environment can also contain potential risks to an individual’s wellbeing.
This guideline was designed for those who have a direct or indirect role in promoting mental wellbeing at work. Recommendations 1 -4 are intended to provide guidance specifically for employers, trade unions and other employee representatives. Whereas recommendation 5 has been specifically formulated to provide guidance for primary care trusts, primary care services and occupational health services hence the information provided in this recommendation is most appropriate and applicable for physiotherapists. However, it is not to say that recommendations 1-4 cannot be used by physiotherapists as the physiotherapists can still advise employers, trade unions and other employee representatives they come into contact with to refer to the advice provided recommendations 1-4.
Recommendation 5 involves supporting micro, small and medium-sized businesses and NICE recommends that primary care trusts, primary care services and occupational health services should:
- collaborate with micro, small and medium-sized businesses and offer advice and a range of support and services including occupational health services.
- establish mechanisms for providing support and advice on developing and implementing organisation-wide approaches to promoting mental wellbeing. These could include tools and approaches for risk assessment, human resources management and management training and development.
This is just one of the recommendations extracted from the guideline, to engage in more in-depth reading of the other recommendations please access:link.
Challenges to Vocational Rehabilitation[edit | edit source]
Vocational rehabilitation enables patients with various health conditions to overcome barriers to accessing, sustaining or returning to employment or other meaningful occupation (Scottish Executive 2007).
Early intervention is key in vocational rehabilitation. The longer the patient is off work, the harder it becomes for them to return to work, making vocational rehabilitation more difficult (Waddell et al 2008).
Vocational rehabilitation has tended to be a specialist focus in physiotherapy, but not everyone will see a specialist in the early stages of disease/injury (University of Salford 2012).
Common barriers to vocational rehabilitation are:
- access to medical treatment due to NHS waiting lists
- economic factors - generous occupational sick pay or disability benefits
- lack of top-level organisational commitment
- cost of workplace modifications and availability of suitable alternative duties, particularly for smaller firms
- poor communication and common purpose among key stakeholders
- lack of co-ordinated approach among rehabilitation providers (Langman 2012)
There is a gap between research and practice in vocational rehabilitation. Evidence based practice is widely used in healthcare settings, however it is a fairly new concept in vocational rehabilitation. Many vocational rehabilitation practitioners report that they face barriers such as inadequate time and limited access to technology and research. A large caseload size was also reported to affect the implementation of evidence based practice in vocational rehabilitation (Lui et al 2014).
Vocational rehabilitation is a complex intervention and being able to implement it involves analysing the training and support used to transfer knowledge and put evidence into practice. Other barriers to implementing evidence based interventions in vocational rehabilitation are issues such as:
- management opposition
- lack of resources such as money and time
- lack of in-house skill
- lack of policy support and networks with other organisations to support a new initiative.
Other barriers lie with the healthcare professional themselves, including a lack of confidence, lack of knowledge, lack of desire for change and their own personal beliefs and the beliefs of others such as line managers (Vocational Rehabilitation Association 2014).
While healthcare has a key role in vocational rehabilitation, it is not a matter for health care alone. There is strong evidence to show that proactive company approaches are effective and cost effective. Vocational rehabilitation depends on work-focused healthcare and accommodating employers. Both are necessary to make a real and lasting difference (Waddell et al 2008). If employers are not accommodating to vocational rehabilitation it can cause a barrier to the healthcare professional providing effective vocational rehabilitation to the patient. It can be difficult to provide the best vocational rehabilitation if the employers are not working with the healthcare professionals to provide the patient with the optimum conditions to return to or stay at work, such as flexible working hours, phased return or modifying the patient's tasks until they can return to their full normal responsibilities and duties.
Unemployment progressively damages health and results in more sickness, disability, mental illness, obesity and decreased life expectancy. Due to significant personal, attitudinal and structural barriers, people with mental health conditions are less likely to be engaged in work roles than those with other health conditions and 85% are unemployed (NHS Scotland 2011).
Another barrier could be the government support to returning to or remaining in work. Currently, most people with mental health problems are put in government run back-to-work schemes (MIND 2105). MIND (2015) state that people with mental health problems should be offered a new vocational rehabilitation approach to returning to work that focuses on person-centred, specialist support that understands the patient and the challenges they face. They report that the current government schemes are actually making people more unwell and less likely to find work. They surveyed 439 people who were receiving support because of their mental health condition. 83% of the people surveyed reported that using back-to-work services through the Work Programme and/or Jobcentre Plus had made their mental health worse or much worse and lowered their self-esteem and confidence. 76% said that they felt less able to work as a result of being on these schemes. MIND (2015) are currently campaigning on this issue. Vocational rehabilitation working with healthcare professionals that have a comprehensive understanding of mental health and strategies to help people with mental health conditions to return to work would be more beneficial and avoid this barrier.
In order to successfully implement vocational rehabilitation, the physiotherapist needs to consider environmental and social factors and understand the patient's perspective on returning to work. These factors can be factors that are outside the individual’s control, individual factors and employer-related factors (Langman 2012).
Factors that are outside the individual’s control include societal beliefs and attitudes, labour market, housing, transport, family and level of support, legal process, government policies and benefits.
Individual factors include self-confidence, self-esteem, motivation, illness beliefs and attitudes, education, literacy, social skills, gender and co-morbidities.
Employer-related factors are things such as sector, size, absence-management policies, culture and physical environment (Langman 2012).
There is a lack of statutory basis for ensuring the delivery of vocational rehabilitation services in the UK, which has contributed to a situation where service provision is not always based on the individual’s needs but on random matters such as the employment status of the individual, the type of benefit they receive, the priorities and resources of the NHS trusts, the circumstances of the injury, employer insurance cover and resources and also the position of the insurer towards funding VR (Langman 2012).
Vocational rehabilitation service providers must understand the motivation of the patient while also maintaining their responsibilities towards the patient, employer, employer’s customers and their own professional standards.
The vocational rehabilitation service provider needs to recognise the patient’s perspective. Any fears they may have, such as future financial security or a fear of failure may, may be justified or subconsciously affecting their judgement (Langman 2012).
It is a good idea to keep a record of intervention and a barriers checklist is a good way of identifying issues and the steps taken to resolve them.
| Clinical | Yes/No | Comments | Response |
| Still receiving treatment | |||
| Operation impending | |||
| Negative impact of medication | |||
| Functional capactity not defined | |||
| Possible behavioural/interpersonal issues | |||
| Poor insight into limitations | |||
| Fatigue | |||
| Pain issues not resolved | |||
| Demographic/Social | Yes/No | Comment | Response |
| Age | |||
| Lack of family support | |||
| Marital issues | |||
| Lack of incentive to work | |||
| Lack of confidence | |||
| Lack of child-care arrangements | |||
| Presentation | |||
| Transport | |||
| Court conviction | |||
| Financial | Yes/No | Comments | Response |
| PI litigation | |||
| Level of benefits income | |||
| Wages being offered | |||
| Risk of return to work upsetting steady income | |||
| Potential retirement with financial gain | |||
| Cost of looking for work | |||
| Skill Related | Yes/No | Comments | Response |
| Overqualified | |||
| Under-qualified | |||
| Lack of IT skills | |||
| Language barrier | |||
| Lack of other skills | |||
| Lack of specific training | |||
| Limited organisational skills | |||
| Limited communication skills | |||
| Patchy work history | |||
| Capacity to learn and retain new skills | |||
| Job Search Related | Yes/No | Comments | Response |
| Limited job search experience | |||
| Lack of CV | |||
| Interview skills | |||
| Lack of references | |||
| Lack of jobs in the field | |||
| No job goal | |||
| Other | Yes/No | Comments | Response |
| Does not function well independently | |||
| Requires aids/adaptations | |||
| Believes they are unemployable | |||
| Does not wish to retrain | |||
| Transport problems | |||
| Possible alcohol/drug dependency | |||
| Cultural issues |
Some frequent issues heard by vocational rehabilitation counsellors are:
1. Why should I work in a job that is going nowhere and doing nothing except frustrate me and cause stress?
2. Why should I take a low paid job when I can get as much money in benefits?
People with mental health conditions are especially sensitive to the negative effects of unemployment and the loss of structure, identity and purpose it provides.
Work is important in maintaining and promoting mental health. It also reduces the need to use health services as it provides a social identity and status, social contacts and supports, a way of occupying and structuring time and a sense of achievement (Langman 2012).
Learning Activity
Case Study
Matilda is a 40-year-old care home assistant in a residential home for the elderly. She has been suffering from low back pain for over 6 months and has been prescribed anti-inflammatory medication and analgesia by her GP. She has not had any other intervention for her low back pain. Matilda is overweight and has diabetes. She reports that her low back pain refers to her buttocks and is made worse by bending forward. Her job is heavy - many of the residents required help with bodily functions and activities of daily living. Because of her low back pain, Matilda is feeling increasingly stressed as she is struggling to do her job and feels that her manager and co-workers are annoyed at her. Matilda feels that this is unsafe for her to do with her low back pain and asked her GP to sign her off work. She has been off work for 3 weeks and is receiving statutory sick pay. You are seeing Matilda as part of a vocational rehabilitation team to help her return to work.
Questions:
1)Using your previous learning from university or experience on placement/at work, what would you look for if you were assessing Matilda for red flags?
2)What barriers do you think Matilda could be facing to return to work?
3)Using your knowledge of pain and stress, and any experience you may have, analyse on how you would approach Matilda and help her remain at or return to work.
4)Think about the barriers facing physiotherapists in vocational rehabilitation and construct ways to overcome these barriers.
Barriers to employment[edit | edit source]
With most conditions there is a relationship between the severity of the injury or impairment and related barriers to employment.
For people with physical injuries, impairments or disabilities environmental barriers to employment can be an issue, such as access to public or private transport and buildings.
People with progressive conditions can face increasing problems in participating in the physical aspects of their work.
Social factors affect those with mental health problems and physical disabilities (Langman 2012)
The emphasis on the medical condition of claimants is a regularly occurring issue in policy approaches towards VR. Typical barriers to returning to work are:
- nature of injury or health condition and its impact on usual work
- lack of support from managers and colleagues
- psychological barriers such as fear of re-injury through work activities, loss of confidence and lack of motivation
- work pressures such as a fear of not being able to undertake ‘light duties’
- lack of suitable adjustments, both physical and to duties/hours of work
- lack of appropriate advice/treatment/rehabilitation programme
- management belief that the worker should be 100% fit before returning to work.
- financial and legal concerns
- fear of returning to the place where an accident occurred/caused stress
- fear of ability to cope with the pre-injury/accident/illness job (Langman 2012).
Vocational rehabilitation users without employment may face the additional issues of restricted labour market opportunities, redundant skills, a lack of a financial incentive, age and disability discrimination, lack of references and transport (Langman 2012).
Barriers to Returning to Work in Stress[edit | edit source]
Almost 50% of long-term absences from work are the result of mental health issues (NHS 2015).
There are many potential barriers for people suffering with stress face when remaining at or returning to work. These barriers include a fear that colleagues may find out about the diagnosis and have possible negative reactions, a loss of connection with co-workers, a perceived or actual lack of support from employers and managers, uncertainty about the level or type of support available, the stigma associated with mental health conditions and concerns that work-related contributors to stress have not been addressed (Heads Up 2015). Common concerns include facing discrimination or bullying and returning to work too soon and feeling unwell again (NHS 2015). Some people fear returning to work because that is the place where their mental health conditions started, for various reasons such as unsupportive or bullying management or team members. Heads Up (2015) suggested some practical strategies to address these barriers, such as educating and providing mental health awareness training for managers and staff.
While work can cause stress for some people in some situations, research shows that work is beneficial to health and well-being, not being in work is detrimental to health and well-being and re-employment after a time period of being unemployed leads to an improvement in health and well-being. Being employed can give the patient a greater sense of identity, an opportunity to meet new people and build new relationships, improve their financial situation and security and help them feel like they are playing an active part in society (NHS 2015).
Barriers to Physiotherapy in Stress[edit | edit source]
There can be communication barriers when working with people suffering from stress. The patient’s communication style may change when they are suffering from stress. They may struggle to find the ‘right’ word or they may swear more than usual. They may also become impatient and intolerant which can cause communication difficulties (Trinity College Dublin 2013).
Stress can cause sleeping problems, difficulty concentrating, low self-esteem, headaches, muscle tension or pain (NHS Choices 2014), all of which can be a barrier to physiotherapy and affect the effectiveness of physiotherapy treatment for different conditions.
Working with employers – what’s hard?[edit | edit source]
A Physiotherapist working in the field of vocational rehabilitation expressed her opinion to us that the main difference between rehabilitation and vocational rehabilitation is than in vocational rehabilitation the physiotherapist has two patients, instead of one. One patient is the employee and the other is the employer. This could potentially cause an issue with confidentiality.
The CSP (2013) Code of Conduct and the HCPC Standards of Proficiency (2013) state that Physiotherapists must maintain patient confidentiality. This means that to advise the employer about the employee’s ability to work, the physiotherapist must have the employees consent to do so. While the physiotherapist cannot divulge information about the employee’s condition, they can let the employer know what the employee is able to do with regards to their job role. The difficulty in this situation would be if the employee did not give consent for the physiotherapist to communicate with the employer. This would make providing vocational rehabilitation difficult as the physiotherapist would be unable to involve the employer in the rehabilitation process.
Role of Physiotherapist in VR[edit | edit source]
As outlined in the previous section VR is a service which can involve people who have gone through many varying situations and can require individualised rehabilitation. Gobelet (2007) demonstrates that vocational rehabilitation uses a pluridiciplinary (multidisciplinary approach) where a typical MTD will consist of physiotherapists, occupational therapists, psychologists, psychiatrists, work counsellors. Many other professions may be involved but that is dependent on the individual needs of the patient. This section will now look more specifically into the role that the physiotherapist plays in the rehabilitation of patients who require VR. We must be careful to outline that there is caution when stating ‘treating though VR’, as VR is more thought of as a connection linked to curing the initial issue, which has led to a person requiring occupation related assistance (Langman 2012).
Physiotherapists play an important role in the rehabilitation of these patients. As reported by the Chartered Society of Physiotherapy (CSP 2015) their aims are get patients back to their best possible level of function and wellbeing including matching, and increasing their normal activities of daily living (ALD’s) which may include activities in the home, for leisure or work. Conditions Treated
One of the most common conditions which a VR physiotherapist comes across are musculoskeletal (MSK), with 22% of these patients presenting (Langman 2012). These physical injuries can come in many forms, from lower back pain (LBP), broken bones and soft tissue injuries. (For an in-depth insight into information surrounding LBP please use the following link http://www.physio-pedia.com/Chronic_Low_Back_Pain). For MSK conditions it is recommended that physiotherapist’s should have an active role in workplace interventions, these interventions should promote health and wellbeing within the workplace in order to encourage normal function. (chronic pain ch 9 (on drive)
Patients suffering from stroke account for just 0.7% of cases seen for VR rehabilitation (Langman 2012), however there are currently 27,500 people each year in England who are of working age, who suffer from strokes. This complex and individualised neurological condition results in many difficult factors which affect a patient’s ability to return to work (RTW). Primarily, mobility issues, cognitive impairment and reduced hand function. (Sinclair et al. 2014) Currently the provision for VR services within this population is low with lack of suitable and appropriately timed care pathways, training to practitioners and integrated health-employer partnerships. Early intervention has been noted as vital and should be coupled with continual support throughout the whole rehabilitation process (Sinclair et al. 2014).
Research has also been undertaken in relation to the effect of VR in terms of dealing with patients after an acquired brain injury. A study last year highlighted how only 40% of people are able to return to paid work within 2 years. It also emphasised the importance of a specific protocol called Early Vocational Rehabilitation, (EVR) which is designed to guide an effective multidisciplinary approach of VR. The EVR protocol comprises of the following stages:
1) orientation of the rehabilitation team towards the patient’s work
2) investigating the gap between the patient’s abilities and work
3) work training
4) finalizing EVR. (Velzen van et al 2015)
^ in Diagram form?!
The final condition which we will look into, has been regarded as having the highest prevalence within VR - mental health. At 35%, which includes patients with stress, depression and anxiety, it is a large proportion of the population. This cannot be said for more serious mental health illnesses such as schizophrenia or cognitive impairments, which have less population size (Dean et al. 2015; Langman 2012).
As with all rehabilitation approaches, practitioners must ensure that the patient's needs are of utmost importance and in order to do this, that physiotherapists are increasingly aiding in the recovery of patients who suffer from psychological conditions. (www.sept.nhs.uk). A well known model (Fig___) called the International Classification of Functioning, Disability and Health (ICF) (WHO 2001) is a biopsychosocial framework which outlines links between how a health problem can impact the different elements of people's lives. Physiotherapists must be aware of this and incorporate it, to provide a holistic approach to VR planning. In order to effectively do this, they should provide advice and treatment based not only just on physiological problems but also psychological symptoms. This is implemented through different guidelines due to the high frequency and significance of mental factors affecting patients. The NHS Knowledge and Skills Framework (KSF) (NHS 2004) acknowledge this importance through Outlines HWB6 and HWB7: “psychological factors throughout assessment, treatment planning and implementation”. This is also stated by the Healthcare and Professions council (HCPC) (Council HaCP 2013) standard 13.9; “influence individuals' responses to their health status and physiotherapy interventions”. Physiotherapists must take the patients' mental aspects of dealing with a condition into consideration and understand the implications of potential coexisting symptoms or the risk of the patient developing new psychological symptoms.
A physiotherapist role in the recovery and rehabilitation of patients suffering from a mental illness merge the treatment of psychological and physical conditions into one. As WHO ( The World Health organization) defines health as absence of disease and infirmity treatment approach.
Role of Physiotherapist in Stress in VR[edit | edit source]
After substantial research we have found the main reason why patients who are stressed tend to be seen by a physiotherapist are due to an initial physiological diagnosis. Commonly it is through treatment of this which will only then determine if the stress can be reduced. As previously described we know that Musculoskeletal problems are the second highest (22%) reason why patients require VR, this coming only behind patients who have been out of work due to stress related conditions (35%). Research also shows that __% of people out of work due to MSK condition have a ___ chance of developing a mental illness. From these statistics we can see just how important physiotherapists work through VR can be, in reducing work related absence.
MAKE DIAGRAM SHOWING CYCLE LINK BETWEEN MSK CONDITION STRESS TIME OFF WORK AND THEN PT IN IF CONDITION IS TREATED = REDUCED STRESS AND REDUCED TIME OFF WORK.
We now understand that physiotherapists within VR can treat patients who are out of work due to a multitude of ailments whether that be physical, mental or psychosocial. However further understanding behind stress in the working population is needed before the topics of physiotherapy treatment and intervention in the management of stress can be discussed.
What is stress in the work place?[edit | edit source]
MedNet.com (2015) defines stress as a physical, mental or external factor that causes physical or physiological strain on the individual. Another definition, looking more specifically at work stress, states that it is a hostile reaction individuals have to too much pressure or strain on them in the workplace. As noted in section ____ stress is becoming a worldwide issue it is important to acknowledging the effects of stress on individuals in and out of the workplace. It is suggested that a considerable percentage of people out of work will develop a mental disorder due to the stress of unemployment, likewise, patients can equally develop a mental disorder and be subject to mental distress within the workplace. (Audhoe. 2009)
So as a physiotherapist whose treatment largely involves physiological techniques, is there anything that can be done?
Benefits of exercise for the treatment of stress within the workplace[edit | edit source]
There is significant evidence to show the benefits of exercise in general and there has been recent increases in the application of prescribed exercise. A systematic review (Lawlor 2001) highlights the benefits of exercise on improving the symptoms of those suffering from depression such as self ______ Society.org highlights that on a physiological level exercise increases the amount of endorphins within the body. These hormones are well associated with happiness and contribute to the feeling of wellbeing and comfort. A rise in the level of endorphins within the body creates a feeling of joy, improves a normal appetite and boosts the immune system. This response to endorphins helps reduce the negative effect of stress on the body. With the increase of prescribed exercise there is also an increased awareness of stress affecting employees in the work place (B, Long 2007). therefore there is an emphasis on creating effective work based exercise programmes aimed at helping people suffering from stress manage their symptoms more effectively. Physiotherapist Treatment With stress management there are key stages that need to be implemented to ensure effective treatment. The initial stage should be highly focused on the education of the individual (Meichenbaum 1985) it is suggested that a heavily structured programme is created and agreed on between employer and employee. There is limited evidence to suggest a precise physiotherapy management for patients suffering from stress. (Waddel, 2008) this can be contributed to the increase in stress cases, yet the still unclarified definition of stress and its manifestations. However there is still great evidence to support the need for an MDT approach when implementing vocational rehabilitation, especially within the work place and out in the community. (C. Gobelet et al 2009). Stress and anxiety were found to be the most frequent, with other diverse symptoms such as anger, depression and low mood effects on patients. (Alexanders et al. 2015). It is important that clinicians recognise warning signs of these conditions as it has been noted that patients who have a psychological complication are more at risk of developing further non problems such as increased muscular tension, development of trigger points and reduced function. After research, within clinical practice there have been many different interventions used by physiotherapists to overcome these mental barriers. Some of these include; relaxation, imagery, cognitive behavioural therapy (CBT) (Brunner et al. 2013), neuro programming (NLP) (Karunaratne 2010) and 'mindfulness based stress reduction' (Dufour et al. 2014). However, the 4 which have been more widely used in clinical practice are: goal setting, positive self talk, effective communication, as well as including variation to rehabilitation exercises.
The rehabilitation goal of all VR patients is hugely driven by the necessity for them to;
a. Remain in work
b. Return to work (RTW)
c. Access employment for the first time
The theory behind implementing patient and physiotherapist led goals during a rehabilitation session, is that it gives both physiotherapist and patient a common target that both feel they can work towards in order for improvement to be seen. Reviews which looked at patients thoughts and interpretation of the effectiveness of goal setting explained that they felt it improved their self confidence, self esteem and self efficacy (Farouk 2010). These positive experiences felt by patients are significant as it has been concluded that patient participation is of extreme importance for when the suitable time is made for goals to be put in place. Apart from increasing the interest and participation of the patient's, goal setting is also provides the benefit of empowering the patient to take their own responsibility for their recovery as well as aiming to make the rehabilitation process more meaningful and patient centred (Alexander et al. 2015). However, even though reports from patients have a shown largely positive insight into goal setting, when researching physiotherapists views on the subject, a different view point is made aware by Schoeb, (2009). It has been found that although goal setting is used widely throughout physiotherapy practices and for many varied patients, there is reason to believe that approaches used for goal setting are rarely standardised. Due to this, it can therefore mean that the effectiveness of approaches used for goal setting can also be inconsistent. Because of this, there is an increased need for training of professionals within this area this requirement has been recognised and agreed by some physiotherapists as being an intervention in which they would like to learn further skills ability to to implement realistic goal setting (________ 2008).
Through these appropriate goals VR will aim to gain patient ability within whichever sector of work is desired, from:
a. Full time employment
b. Part time employment
c. Self employment
d. Voluntary work
When looking towards vocational rehabilitation for the management of patients suffering
with stress it is important as physiotherapists recognise the importance of an effective relationship between patient and practitioner.
There is strong evidence to suggest that communication between professions is essential in
creating an effective Vocational Rehabilitation programme as there is not one single
profession that can deliver the service effectively. There is strong evidence to suggest that
communication during this process needs to be improved (Beaumont 2003a; Beaumont
2003b; MacEachen et al. 2006; Shaw et al. 2002).
From a qualitative review of therapists certain characteristics and qualities were
deemed the most effective in creating a positive alliance between patient and
therapist throughout the process of vocational rehabilitation. It was shown that the
main characteristics to creating a positive patient therapist relationship were as
follows; being trustworthy, experienced in their field; flexible, respectful, confident,
warm and open. It is suggested that these qualities will enable a patient to have a
more supportive beneficial relationship with the clinician which should will allow for
greater prospects for change (Ackerman 2003). Therefore while practicing, it is
essential to be aware of these traits as applying this knowledge may benefit the
relationship that you are able to build with your patient and may have a positive
experience on their treatment.
Settings (?)[edit | edit source]
The stage at which physiotherapists enter into VR can be seen in Fig. _(FB)__. It must be noted that the point of entry does not and should not end here, ideally continuing to progress until an ultimate goal has been reached.
INSERT DIAGRAM (FB)
The CSP (2016) suggests that for physiotherapy intervention for work based sickness to be effective it has to be easily accessible and started promptly after the initial onset of illness. By playing a role in VR at such an early stage, it is important that those patients in need are seen early by a physiotherapist. To help with this, VR physiotherapists can be in a range of settings allowing for larger access to many various people. • further info required As healthcare professionals physiotherapists also experience stress. From a study looking at 3 general hospitals it identity’s the main causes of occupational stress. This study uses The Occupational Stressors Inventory questionnaire as a way to evaluate the participants perceived stress levels. This is a 23 point, self-rated questionnaire. It was used on 55 physiotherapists in Lisborn to establish their main occupational stresses. From the 55 participants over half deemed themselves to be moderately stressed within the workplace. From the study, it was established that the main causes of stress were lack of order in the hierarchy command chain, disorganisation in work distribution, overload and low salary.
For continued up to date information on the principle of vocational rehabilitation, we encourage our readers to subscribe for the ‘Journal of Vocational Rehabilitation’.
Task What methods of communication are you aware/experience and what ways could you implement good communication within your practice. Take time to compare and contrast your ideas and justify your top 3 choices.
• ? Cancer information
• OM
• health risks at work??!
• ways to prevent work related injuries?!
• initiative to encourage exercise in workplace - monro signs, cycle to work schemes etc
• courses available for employers http://www.healthyworkinglives.com/events/national---mentally-healthy-workplace-training-blended-700
• enhance setting research
• effects for pts with mental health illness already?!
Stress, cancer and vocational rehab/time off work Stress can be a contributing factor to many health problems, however the evidence for stress being a cause of cancer is weak. Furthermore, people who suffer from stress many develop certain habits such as smoking, drinking excessive amounts of alcohol or overeating, which in turn, can increase the risk of developing cancer. (National Cancer Institute 2015).
People who have cancer may find the physical, emotional, and social effects of the disease to be stressful. Although there is no evidence that successful management of psychological stress improves cancer survival, there are benefits to using effective coping strategies when dealing with stress. Methods such as relaxation and stress management techniques can reduce levels of depression and anxiety in relation to cancer and its associated treatments. (National Cancer Institute 2015). There have been various studies carried out to investigate the effect of stress on the growth and spread on cancerous tumors, concluding that stress can have an effect. (Brief examples on National Cancer Institute site but can look to find articles if required?) Emotional and support can help cancer patients to cope with psychological stress positive impacts on reducing depression, anxiety and disease/ treatment related symptoms. These can take place in the form of: Cancer related post traumatic stress can also occur at any time during or after treatment. This is similar to post traumatic stress disorder but not usually as severe. Returning to work often plays an important role in cancer survivors. However, occupational stress is often a barrier to returning to work in cancer survivors so it is important that they are given sufficient opportunity to address this prior to returning to work. A study by Bottcher et al (2012) looked at the level of occupational stress amongst cancer patients and its associations with their well being, their subjective need for occupational rehabilitation and elevations in their risk of early retirement. At the beginning of rehab, patients were asked to complete a variety of occupation and health related questionnaires. Of the 477 patients participating, 19% were occupationally stressed and 26% reported subjective need for occupational rehab. Cancer patients reported decline in active coping strategies and mental stability at work, aswell as diminished quality of life. There is a strong link between occupational stress and early retirement. Screening patients for occupational stress is suggested as this may help clinicians to identify those patients at risk of experiencing problematic work re maintaining confidence when faced with work related tasks and so the development of a perception of self efficacy may be an effective treatment goal. • now explain how a physio plays a role in helping cancer pts by supplying them with suitable occupational health, coping strategies and mental stability at work
_____________________END OR INFORMATION TO BE READ IN DRAFT DAY 18th JAN_____________________________
- <g class="gr_ gr_234 gr-alert gr_spell ContextualSpelling ins-del multiReplace" id="234" data-gr-id="234">Consolodate</g> all evidence
- OUTCOME MEASURES HEADING
http://www.mdpi.com/1660-4601/12/2/1928/htm
http://www.mdpi.com/1660-4601/12/2/1928/htm==
(Alexanders et al. 2015) 2002 – 2013 studies
Physiotherapists must take a holistic approach to health and well-being recognising the importance of how diverse symptoms such as anger, depression and low-self-esteem have effects of patients and so their potential treatment outcomes.
Documents to help PT with this, include:
NHS KSF Outlines in HWB6 and HWB7; require the consideration of both physiological and psychological factors throughout assessment, treatment planning and implementation.
HCPC; standard 13.9;
University physiotherapy degree programmes consider many topic areas which fall under the word 'psychology'; communication skills, personality theories, effective team working and the impact of terminal illness on mental health.
Within clinical practice there are many different interventions used by physiotherapists. Some of these highlighting in _________________ (refs 2 and 10 of Alexs) study include; relaxation, imagery, positive self talk and goal setting. Cognitive behavioural therapy (CBT), neuro-linguistic programming (NLP) and 'mindfulness based stress reduction' are also being used. (14, 15,18 resp)
(Specific disciplines of physiotherapy practice are also beginning to include such interventions ,mostly chronic pain (11), anterior cruciate ligament rehabilitation (10), neurology (12,13) and sport (2).
Systematic Review - Exploration of MSK PT perceptions regarding use of psychological interventions in clinical practice: Studies investigated “common psychological symptoms that PT encounter within clinical practice.”
RESULTS:
“Stress and anxiety were the most frequently encountered psychological symptoms amongst individuals undergoing rehabilitation”
Interventions; “In particular goal setting, positive <g class="gr_ gr_256 gr-alert gr_spell ContextualSpelling multiReplace" id="256" data-gr-id="256">self talk</g>, effective communication and variation in rehabilitation exercises all appear to be relatively widely used.”
PT would like to improve their ability to improve their ability to implement realistic goal setting (24, 25)
4/6 studies say they received insufficient psychological training during Bsc studies (22,23,26,27)
PT working in MSK environment commonly encounter psychological symptoms.
Pt suffering from psychological symptoms following injury are more likely to develop non-specific MSK complaints eg increased muscular tension, development of trigger points and reduced function.
Occurrence of psychological symptoms following injury are frequent and significant issues
A vaulable approach in tackling this issue is to integrae psychological interventions within physiotherapy practice. Psychological interventions are used widely by MSK PT, using; goal setting, positive self talk and effective communication, with goal setting being identified as the most common psychological intervention.
^This is particularly encouraging finding given that goal setting during rehabilitation appears to improve patients' self confidence, self esteem and self efficacy (32)
Goal setting highlighted as an intervention PT want to learn more about ;
(33 Schoeb) detailed insight into use of goal setting in clinical setting – GS is frequently employed by PT however the approaches used for goal setting are rarely standardised. Effectiveness of GS varies significantly between difference PT's.
Study with difference HCP indicated GS has many difficulties; poor patient involvement throughout the goal setting process. (34)
Goal setting has been proven to have minimal consideration being given to psychological implications.
^ significant as “ patient participation appears to be of paramount importance – due to many beneficial effects associated with patient participation”
- Increasing patient participation during rehabilitation
- empowering patients to take responsibility for their recovery - making rehabilitation process more meaningful to patients.
Key points from systematic review:
Disparity between PT's reported use of goal setting and the training [rovided in this area in Bsc degree - some degrees do not provide sufficient level of formal training in the use of psychological interventions. - Pts repor feeling inadequatly trained in psychological interventions and welcome further training.
PT's ability to effectively incorporate psychological interventions would maximise potential of individual patients eg ensuring when goals are set they are both patient led and not just therapist led - so there is a need to review curricula of PT degrees to ensure training of psychological interventions is standarised!!
Future research using observational methods to investigate PT's implementation of goal setting in clinical setting would provide further insight into this area and be of value in identifying PT's training needs.
PT perceptions and practical use of psychological interventions are limited Clearly warranted due to large occurrence and impact on treatment outcomes Required to compare sporting private vs hospital NHS
(Romano and Peters 2015) Mechanisms of change in motivational interviewing: Meta analysis
Key points:
Motivational Interviewing (MI) is a patient centred directive method of facilitating change that aims to enhance motivation through the exploration and resolution of ambivalence (Miller & Rollnick, 1991). MI was originally developed to treat substance use disorders, however, the application of MI has extended to a growing list of psychological and physical health issues. Meta-analytic research provides support for the efficacy of MI in the treatment of physical activity, dietary change, and diabetes (Martins & McNeil, 2009), and gambling and general health promoting behaviours (Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010). There is also a growing evidence base to suggest that MI is useful as an adjunctive treatment to enhance treatment outcomes for patients presenting with anxiety disorders (Aviram & Westra, 2011; Westra, Arkowitz, & Dozois, 2009; Westra & Dozois, 2006),
However, in the treatment of psychological disorders such as anxiety and eating disorders, MI is primarily used as an adjunctive treatmentwith an aim to enhance treatment gains as a result of another treatment. In these areas, employing MI is thought to facilitate patient motivation and engagement in other treatment (e.g., cognitive behavioural treatment; CBT), thereby potentially yielding more positive outcomes (Westra, Aviram, & Doell, 2011). H I G H L I G H T S
• Motivational interviewing (MI) is useful in the treatment of a variety of mental health problems. • Previous meta-analyses of MI mechanisms of change are limited to substance using populations. • This review examined change mechanisms in patients diagnosed with anxiety, mood, eating, psychotic, and comorbid conditions. • Research should further examine MI mechanisms of change in diverse populations.
This review is a first attempt to investigate and meta-analyse MI mechanisms of change research conducted with participants who suffer mood, anxiety, psychotic, eating disorders, and comorbid conditions.
Results indicated that while MI did not increase patient motivation more so than did comparison conditions, MI showed a favourable effect on patient engagement variables
Overall, there were few MI mechanisms of change available for review, though the results suggest that patient engagement with treatment may be a potential mechanism of change in populations diagnosed with anxiety, mood, and psychotic disorders.
Anxious participants who receivedMI prior to CBT showed less resistance during CBT than thosewho did not receive a pre-treatment. When compared to CBT, MI also achieved a positive effect on resistance
Also, anecdotal evidence from therapists suggested that participants who attendedMI groups were more willing to engage in discussions about change (Dean et al., 2008),which supports the role ofMI in facilitating the change process.Moreover, quantitative findings demonstrated that participants who completed MI were more willing to partake in CBT and were more open to therapist contact (Buckner & Schmidt, 2009).While these datawere not included in effect size calculation, the findings further support the positive effect ofMI on engaging patients in active treatment.
Hsieh et al 2012 – DASS scale (depression, Anxiety, Stress Scale)
Coping with Work-Related Stress through Guided Imagery and Music (GIM): Randomized Controlled Trial (Bolette Daniels Beck, PhD, Åse Marie Hansen, PhD and Christian Gold, PhD,2015)
Background: Long-term stress-related sick leave constitutes a serious health threat and an economic burden on both the single worker and the society. Effective interventions for the rehabilitation and facilitation of return to work are needed.
Objective: The aim of the study was to examine the effects of Guided Imagery and Music (GIM), a psychotherapy intervention including relaxation, music listening, and imagery, on biopsychosocial measures of work-related stress.
Results: Significant beneficial effects of GIM compared to wait-list after nine weeks with large effect sizes were found in well-being, mood disturbance, and physical distress, and in cortisol concentrations with a medium effect size. A comparison between early and late intervention as related to the onset of sick leave showed faster job return and significantly improved perceived stress, well-being, mood disturbance, depression, anxiety, and physical distress symptoms in favor of early intervention. In the whole sample, 83% of the participants had returned to work at nine weeks’ follow-up.
Conclusions: The results indicate that GIM is a promising treatment for work-related chronic stress, and further studies are recommended.
http://www.bbc.co.uk/news/uk-scotland-highlands-islands-34572044
^Bycycle inititive
Taehan Kanho Hakhoe Chi. 2007 Jun;37(4):529-39. [A meta-analysis of effects of job stress management interventions (SMIs)]. [Article in Korean] Kim JH1. Author information Abstract PURPOSE: This quantitative meta analysis sought to determine the effectiveness of SMIs. METHOD: Forty-six experimental studies with a randomized or nonequivalent control group pre-post test design were included in the analysis. The selected studies were classified according to the sample characteristics, the types and methods of the interventions, and the types of outcome variables. Six intervention types were distinguished: cognitive-behavioral intervention(CBT), relaxation techniques(RT), exercise(EX), multimodal programs 1 and 2(MT1, 2), and organization focused interventions(OTs). Effect sizes were calculated for the 4 outcome categories across intervention types: psycho-social outcome, behavioral-personal resources, physiologic, and organizational outcome. RESULTS: Individual worker-focused interventions(ITs) were more effective than OTs. A small but significant overall effect was found. A moderate effect was found for RT, and small effects were found for other ITs. The effect size for OTs was the smallest. The interventions involving CBT and RT appeared to be the preferred means of reducing worker's psycho-social and organizational outcomes. With regard to physiologic outcomes, RT appeared to be most effective. CBT appeared to be most effective in reducing psycho-social outcomes. The effects of OT were non-significant, except for the psycho-social outcomes. CONCLUSIONS: SMIs are effective. Interventions involving RT and CBT are more effective than other types.
Med Pr. 2010;61(2):191-204. [Stress prevention programs--strategies, techniques, effectiveness. Part II. Organizational activities to prevent stress at work]. [Article in Polish] Małgorzata W1, Merecz D, Drabek M. Author information Abstract This is the second part of the publication on approaches to occupational stress prevention and a state of the art in different European countries. In this part, stress prevention within an organization is described and discussed. Although there is no one way of tackling stress at work, some recommendations can be formulated to increase the effectiveness of such interventions. The effective stress reducing programs should be aimed both at changes in the organization itself and empowerment of employees' coping with stress resources. It is also important to take the advantage of wide spectrum of methods and techniques (e.g., work redesign, participation, team work, cognitive behavioral methods, relaxation, etc.) remembering that one size does not fit all. The intervention should be carefully planned and adopted to the various branches, an individual organization or department and should be preceded by the identification of stress risks and risk groups. To have the stress prevention program successfully introduced one should also consider factors which may influence (positively or negatively) the process of program implementation.
Conclusion[edit | edit source]
- - Linking diagram; consolodating eveything
Final Task[edit | edit source]
As you did in the first task, construct another mind map of what you have learnt through this wiki on vocational rehabilitation and on stress. Contrast and compare these two mind maps. Critically evaluate how you could use this new knowledge in your current practice.
Recent Related Research[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.