The effect of Pilates on pelvic floor muscle strength in women with urinary incontinence
Introduction[edit | edit source]
The prevalence of Urinary Incontinence (UI) is approximately 48.3 and 46.4%, and only 26% of women, presenting with UI symptoms, consulted a doctor. Stress UI seems to be more common under younger women and urgency UI dominate more common among women older than 80 years. Women with a body mass index (BMI) ≥35 had the highest prevalence of UI[1][2].
Conditions such as; urinary incontinence, pelvic organ prolapse, pain and sexual disorders; are associated with weakness of pelvic floor muscles (PFM)[3].
Clinically Relevant Anatomy[edit | edit source]
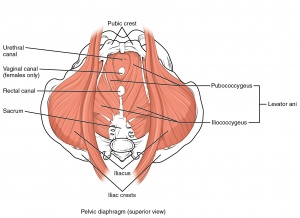
The bladder, uterus, rectum and the urethral- and anal sphincters are surrounded by a dome-shaped striated muscular sheet called the Pelvic Floor Muscles (PFM). This dome-shaped structure plays an important role in storing and elimination of urine and stool[4].
The PFM mainly consists of the levator ani and coccygeus muscles[4].
The levator, coccygeus and urogenital diaphragm are innervated by S2, S3, and S4 nerve fibres; while the external anal sphincter is innervated by the pudendal nerve [5].
Mechanism of pelvic floor Injury[edit | edit source]
Literature indicates a strong association between vaginal childbirth and pelvic floor disorders however, further research is necessary to determine which aspects of childbirth contribute most[6].
Pregnancy and childbirth may lead to pelvic floor injury due to compression, stretching or tearing of nerve, muscle, and connective tissue.
The following pelvic floor-complications may occur due to pregnancy and childbirth;
- neural injury (due to compression during labour and vaginal delivery),
- levator ani and coccygeus muscles injury,
- fascial injury, and
- impaired connective tissue remodelling (increased synthesis of collagen and elastin causes an alteration in soft tissue biomechanics during pregnancy)[7].
For further information regarding clinical presentation and diagnostic procedure, please read 'Incontinence'
Pilates-centred Pelvic Floor Muscle Training (PFMT)[edit | edit source]
It's important to understand that PFM function in synergy with abdominal muscles, chest wall and diaphragm, and not in isolation. Throughout each day, the intra-abdominal pressure and trunk muscle activity alternate regularly. The PFM have to respond rapidly to these changes to prevent incontinence or prolapse of pelvic organs.
The pilates concept is based on 'centre'(core) and 'control'. The pilates method focusses on the following muscles when referring to the 'core';
- PFM (inferiorly),
- diaphragm (superiorly),
- transverse abdominis (TrA) and oblique muscles (anteriorly)
- multifidus (posteriorly)[8]
Therefore, when rehabilitating the PFM, it is important to do so in conjunction with the other muscular groups named above.
Pilates exercise program vs. conventional PFM exercise program[edit | edit source]
A Pilates exercise - and conventional PFM exercise program seems to be equally effective, in improving the recovery time of UI, as well as improve quality of life (QoL). However, higher rates of fully-recovered individuals, diagnosed with UI, are found among individuals following Pilates exercise programmes[8].
Why might the Pilates method be better?
- A lower financial impact on the healthcare system
- Less discomfort (no internal devices)
- An alternative for individuals disliking conventional PFM exercises[8]
Current best available evidence states that individuals, diagnosed with UI, can benefit by doing as little as one session per week, for 8 to 52 weeks[8].
Clinicians often apply activity restrictions among women suffering from pelvic floor disorders. This is due to the association of increased intra-abdominal pressure (IAP) with pelvic floor loading. Fortunately, a study completed by Coleman et al. (2015), determined no statistically significant difference between the IAP in sit-to-stand and fundamental Pilates exercises and therefore recommends Pilates exercises to women desiring a low intra-abdominal pressure exercise routine[9].
Modified Pilates (MP) as an adjunct to conventional physiotherapy care seems to be even more beneficial in improving self-esteem, decreasing social embarrassment and lowering impact on normal daily activities[10].
Examples of Pilates exercises[edit | edit source]
1. Activation (supine/ crook-ly)[edit | edit source]
2. Pelvic Clock (supine/ crook-ly)[edit | edit source]
moving pelvis like a clock to facilitate spinal flexion, extension, lateral flexion and rotation
3. Bridging (supine/ crook-ly)[edit | edit source]
posterior pelvic tilt pelvis, then elevate the pelvis
4. Adductor Squeeze (supine/ crook-ly)[edit | edit source]
contract muscles by squeezing a ball between knees
5. Bent Knee fall out (supine/ crook-ly)[edit | edit source]
unilateral abduction with pelvic stabilization
6. Supine Arm series (supine/ crook-ly)[edit | edit source]
arm work in flexion, abduction and rotation with trunk stabilization
7. 4 point kneeling position[edit | edit source]
elevate one limb with trunk stabilization or maintaining a neutral spine
8. Roll down series (seated)[edit | edit source]
segmented spinal flexion and back up maintaining PFM activation
9. Standing Leg Pump[edit | edit source]
1 leg dissociation (hip and knee flexion) with trunk and pelvic stabilization
10. Assisted Squat[edit | edit source]
squat with trunk stabilization and co-contraction of core [8]
Related articles[edit | edit source]
add text here relating to the differential diagnosis of this condition
References[edit | edit source]
- ↑ Schreiber Pedersen L, Lose G, Høybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta obstetricia et gynecologica Scandinavica. 2017 Aug;96(8):939-48.
- ↑ Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. International urogynecology journal. 2012 Aug 1;23(8):1087-93.
- ↑ Martinez CS, Ferreira FV, Castro AA, Gomide LB. Women with greater pelvic floor muscle strength have better sexual function. Acta obstetricia et gynecologica Scandinavica. 2014 May;93(5):497-502.
- ↑ 4.0 4.1 Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterology & Motility. 2006 Jul;18(7):507-19.
- ↑ Percy JP, Swash M, Neill ME, Parks AG. Electrophysiological study of motor nerve supply of pelvic floor. The Lancet. 1981 Jan 3;317(8210):16-7.
- ↑ Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A. Pelvic floor disorders 5-10 years after vaginal or cesarean childbirth. Obstetrics and gynecology. 2011 Oct;118(4):777.
- ↑ Handa VL. Urinary incontinence and pelvic organ prolapse associated with pregnancy and childbirth. UpToDate2014. 2015.
- ↑ 8.0 8.1 8.2 8.3 8.4 Pedriali FR, Gomes CS, Soares L, Urbano MR, Moreira EC, Averbeck MA, de Almeida SH. Is pilates as effective as conventional pelvic floor muscle exercises in the conservative treatment of post‐prostatectomy urinary incontinence? A randomised controlled trial. Neurourology and urodynamics. 2016 Jun;35(5):615-21.
- ↑ Coleman TJ, Nygaard IE, Holder DN, Egger MJ, Hitchcock R. Intra-abdominal pressure during Pilates: unlikely to cause pelvic floor harm. International urogynecology journal. 2015 Aug 1;26(8):1123-30.
- ↑ Lausen A, Marsland L, Head S, Jackson J, Lausen B. Modified Pilates as an adjunct to standard physiotherapy care for urinary incontinence: a mixed methods pilot for a randomised controlled trial. BMC women's health. 2018 Dec;18(1):16.