Template:TXSTEBP
Original Editors
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit source]
Database Search: CINHAL, Cochrane Library, JOSPT, PEDro, PubMed
Keywords: lumbar, fracture, management, therapy, burst, osteoporosis, nonoperative, treatment, thoracolumbar
Search Timeline: April 13, 2011 - May 1, 2011
Definition/Description[edit source]
The complex shape of the vertebra, along with the interaction of Central Nervous system and interactions with relatively specialized structures like the intervertebral disks the associated vertebral ligaments has made the description and classification of spinal fractures an ongoing pursuit for the medical community. The current system had its roots in 1963 after Holdsworth proposed classifying spinal fractures by the MOI of compression, flexion, extension, and flexion-rotation. He divided the injuries involvement of the anterior weight bearing column and the posterior “tension bearing” column of facet joints and ligament complex[1].
In 1983 the Denis system revised this to add in a center column comprised of the posterior vertebral body, posterior vertebral disk and Posterior Longitudinal ligament[1].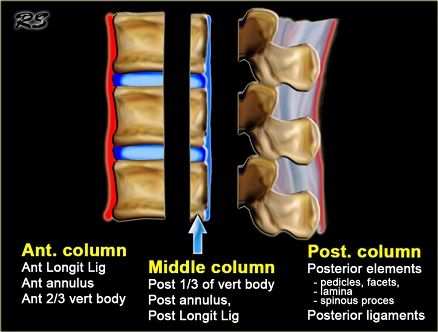
In his paper it was believed that trauma focused into the middle column was sufficient to cause instability in the spine. The instability was further categorized into three types: first degree instability, considered mechanical, second degree instability was considered neurological or combined mechanical/neurological that was considered third degree instability. The Denis system is still currently the favored method. The main frustration from the Denis method is that the inclusion of the middle column introduced a “virtual landmark” that isn’t really suitable for determining an injury type. A recently developed a system by Aebi incorporates the two column method, combined with the method of injury, and the instability which may result in neurological compromise. This method can result in 27 subgroups of spinal fractures4! Obviously the classification of fractures is complicated and ongoing.
The American Academy of Orthopedic Surgeons website5 lists fractures based on the pattern of injury and in a simpler format:
The flexion pattern contains compression fractures, and axial burst fractures5.
The extension pattern, which contains an extension/distraction (often called a chance fracture).
The rotation pattern contains transverse process and fracture-dislocation5.
While the listed examples above all imply trauma for a spinal fracture, osteoporosis and conditions such as osteogenesis imperfect are commonly implicated in vertebral fractures as well.
Epidemiology /Etiology[edit source]
The extension pattern of lumbar fractures:
•A chance fracture results from a distraction accident such as stopping quickly and the force from a seatbelt pulling your vertebrae apart.
The flexion pattern of lumbar fractures:
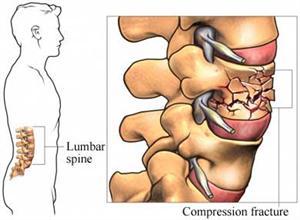
•Compression fractures are usually caused by an axial load that causes the anterior vertebrae to lose height5. Axial Burst fractures are caused by an axial load of a sudden acceleration or deceleration transmitted thru the spine that causes the vertebrae to lose height on all sides.
•Burst fractures may result in some retropulsion of the vertebra into the vertebral canal3. Compression and burst fractures are most commonly seen in falls and traffic accidents6.
The rotation pattern of lumbar fractures:
•Transverse Process (TP) fractures are uncommon and result from extreme sideways bending. These do not usually affect stability.
•The fracture-dislocation is a fracture in which bone and its accompanying soft tissue will move off an adjacent vertebra. This type is an unstable fracture and may cause severe Spinal cord compression.
Characteristics/Clinical Presentation[edit source]
add text here
Differential Diagnosis[edit source]
add text here
Examination[edit source]
add text here
Medical Management (current best evidence)[edit source]
add text here
Physical Therapy Management (current best evidence)[edit source]
Key Research[edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit source]
add appropriate resources here
Clinical Bottom Line[edit source]
add text here
Recent Related Research (from Pubmed)[edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit source]
1. Holdsworth FW. Fractures, dislocations and fracture/dislocation of the spine. J Bone Joint Surg Br 1963;45:6-20.
2. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 1983;8:817-31.
3. Heary R, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian Journal of Orthopaedics [serial online]. October 2007;41(4):268-276. Available from: Academic Search Complete, Ipswich, MA. Accessed April 14, 2011.
4. Aebi M. Classification of thoracolumbar fractures and dislocations. European Spine Journal. October 2009;19: (suppl I):S2-S7. Accessed April 25, 2011.
5. American Academy of Orthopedic Surgeons web site. Available at: http://orthoinfo.aaos.org/topic.cfm?topic=a00368
Assessed 4/28/2011.
6. Heary R, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian Journal of Orthopaedics [serial online]. October 2007;41(4):268-276. Available from: Academic Search Complete, Ipswich, MA. Accessed April 14, 2011