Systemic Lupus Erythematosus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div> <div class="editorbox"> | <div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox"> | ||
'''Original Editors '''- [[User:Alli Christian|Alli Christian]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[User:Alli Christian|Alli Christian]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | ||
</div> | </div> | ||
== Definition/Description<br> == | == Definition/Description<br> == | ||
Lupus erythematosus is an autoimmune disease that can manifest itself in several different ways including: discoid lupus erythematosus (DLE), systemic lupus erythematosus (SLE), drug-induced lupus, late-state lupus, and antiphopholipid antibody syndrome. With this condition, "the body creates antibodies | Lupus erythematosus is an autoimmune disease that can manifest itself in several different ways including: discoid lupus erythematosus (DLE), systemic lupus erythematosus (SLE), drug-induced lupus, late-state lupus, and antiphopholipid antibody syndrome. With this condition, "the body creates antibodies against its own cells." These antibodies can be formed against many different tissues and components of the body including RBCs, neutrophils, platelets, lymphocytes, etc. For this reason, SLE can affect almost any area of a person's body.<ref name="Goodman et al">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd edition. St. Louis, Missouri: Saunders Elsevier, 2009.</ref> Systemic lupus erythematosus is a chronic, rheumatic, inflammatory disease that can affect a person’s skin, joints, kidneys, lungs, heart, nervous system, blood, and mucous membranes. It does not affect all patients in the same way, so patients experience variable organ involvement after being diagnosed with SLE.<ref name="Goodman et al" /> <ref name="Goodman cc et al">Goodman CC and Synder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th edition. St. Louis, Missouri: Saunders Elsevier, 2007.</ref> | ||
== Prevalence == | == Prevalence == | ||
| Line 16: | Line 16: | ||
*Most people are diagnosed with the disease between the ages of 15 and 40<ref name="Goodman cc et al" /> | *Most people are diagnosed with the disease between the ages of 15 and 40<ref name="Goodman cc et al" /> | ||
*Rarely diagnosed in the elderly <ref name="Laranzo et al" /> | *Rarely diagnosed in the elderly <ref name="Laranzo et al" /> | ||
*Occurs in 10-20/100,000 children (depends on the | *Occurs in 10-20/100,000 children (depends on the population) | ||
*About 15% of people diagnosed with SLE are younger than 18 years old, and when a person is diagnosed at an early age, the disease progresses more quickly and severely than if diagnosed after the age of 18.<ref name="Tucker et al">Tucker LB. Making the diagnosis of systemic lupus erythematosus in children and adolescents. Lupus; 16: 546-549. 2007.</ref> | *About 15% of people diagnosed with SLE are younger than 18 years old, and when a person is diagnosed at an early age, the disease progresses more quickly and severely than if diagnosed after the age of 18.<ref name="Tucker et al">Tucker LB. Making the diagnosis of systemic lupus erythematosus in children and adolescents. Lupus; 16: 546-549. 2007.</ref> | ||
*More prevalent in those who have a family history of SLE than it is in the general population<ref name="Goodman et al" /><br> | *More prevalent in those who have a family history of SLE than it is in the general population<ref name="Goodman et al" /><br> | ||
| Line 29: | Line 29: | ||
*Arthralgia | *Arthralgia | ||
*Skin rashes | *Skin rashes | ||
*Pulmonary involvement (symptoms include: chest pain,difficulty breathing, cough) | *Pulmonary involvement (symptoms include: chest pain, difficulty breathing, and cough) | ||
*Anemia | *Anemia | ||
*Kidney involvement (lupus nephritis) | *Kidney involvement (lupus nephritis) | ||
| Line 59: | Line 59: | ||
== Medications == | == Medications == | ||
*'''<u>[http://www.drugs.com/search.php?searchterm=analgesics&is_main_search=1 Analgesics]</u>'''<u>[http://www.drugs.com/search.php?searchterm=analgesics&is_main_search=1 ]:</u> These medications are used to control the pain that a patient has to endure from the pain of arthralgia, arthritis, and ulcers that SLE can cause.<ref name="Laranzo et al" /> | *'''<u>[http://www.drugs.com/search.php?searchterm=analgesics&is_main_search=1 Analgesics]</u>'''<u>[http://www.drugs.com/search.php?searchterm=analgesics&is_main_search=1]:</u> These medications are used to control the pain that a patient has to endure from the pain of arthralgia, arthritis, and ulcers that SLE can cause.<ref name="Laranzo et al" /> | ||
*[http://www.drugs.com/search.php?searchterm=Non-steroidal%20antiinflammatory%20&is_main_search=1 '''<u>Non-Steroidal Anti-inflammatory Drugs (NSAIDS)</u>:'''] These medications help to decrease tissue inflammation, and therefore decrease the patient’s joint and muscle pain. | *[http://www.drugs.com/search.php?searchterm=Non-steroidal%20antiinflammatory%20&is_main_search=1 '''<u>Non-Steroidal Anti-inflammatory Drugs (NSAIDS)</u>:'''] These medications help to decrease tissue inflammation, and therefore decrease the patient’s joint and muscle pain. | ||
*'''<u>Anti-malarials</u>''': These medications are used to treat a patient's arthritic, musculocutaneous, and renal symptoms that are associated with SLE. <br> - [http://www.drugs.com/search.php?searchterm=Chloroquine%20&is_main_search=1 Chloroquine (Aralen)]<ref name="Goodman et al" /><ref name="Laranzo et al" /><br> - [http://www.drugs.com/search.php?searchterm=Hydroxychloroquine%20&is_main_search=1 Hydroxychloroquine (Plaquenil)]<ref name="Laranzo et al" /> | *'''<u>Anti-malarials</u>''': These medications are used to treat a patient's arthritic, musculocutaneous, and renal symptoms that are associated with SLE. <br> - [http://www.drugs.com/search.php?searchterm=Chloroquine%20&is_main_search=1 Chloroquine (Aralen)]<ref name="Goodman et al" /><ref name="Laranzo et al" /><br> - [http://www.drugs.com/search.php?searchterm=Hydroxychloroquine%20&is_main_search=1 Hydroxychloroquine (Plaquenil)]<ref name="Laranzo et al" /> | ||
*'''<u>[http://www.drugs.com/search.php?searchterm=corticosteroids&is_main_search=1 Corticosteroids]</u>'''<u>[http://www.drugs.com/search.php?searchterm=corticosteroids&is_main_search=1 ]:</u> These drugs are usually only prescribed to patients with severe SLE whose signs and symptoms are not improving with any other drug therapy. Corticosteroids can give the patient relief from constitutional symptoms, arthritis, and cutaneous problems caused from SLE. | *'''<u>[http://www.drugs.com/search.php?searchterm=corticosteroids&is_main_search=1 Corticosteroids]</u>'''<u>[http://www.drugs.com/search.php?searchterm=corticosteroids&is_main_search=1]:</u> These drugs are usually only prescribed to patients with severe SLE whose signs and symptoms are not improving with any other drug therapy. Corticosteroids can give the patient relief from constitutional symptoms, arthritis, and cutaneous problems caused from SLE. | ||
*'''<u>Immunosuppressant Agents</u>''': These drugs are used to decrease inflammation, treat lupus nephritis, and suppress the patient's immune system. <br> - [http://www.drugs.com/search.php?searchterm=Azathioprine%20&is_main_search=1 Azathioprine (Imuran)]<br> - [http://www.drugs.com/search.php?searchterm=Cyclophosphamide%20&is_main_search=1 Cyclophosphamide (Cytoxan)]<ref name="Goodman et al" /><ref name="Laranzo et al" /><br> | *'''<u>Immunosuppressant Agents</u>''': These drugs are used to decrease inflammation, treat lupus nephritis, and suppress the patient's immune system. <br> - [http://www.drugs.com/search.php?searchterm=Azathioprine%20&is_main_search=1 Azathioprine (Imuran)]<br> - [http://www.drugs.com/search.php?searchterm=Cyclophosphamide%20&is_main_search=1 Cyclophosphamide (Cytoxan)]<ref name="Goodman et al" /><ref name="Laranzo et al" /><br> | ||
| Line 74: | Line 74: | ||
*Hemolytic anemia, leukopenia, lymphopenia, thrombocytopenia | *Hemolytic anemia, leukopenia, lymphopenia, thrombocytopenia | ||
*Neurologic disorder: seizures or psychosis | *Neurologic disorder: seizures or psychosis | ||
* | *Non-erosive arthritis of two or more peripheral joints characterized by tenderness, swelling, or effusion | ||
*Oral or nasopharyngeal ulcerations [[Image:Discoid rash.png|right|200x250px|This is an illustration of a discoid rash that is characteristic of a patient with SLE. It is included in this project courtesy of www.googleimages.com]] | *Oral or nasopharyngeal ulcerations [[Image:Discoid rash.png|right|200x250px|This is an illustration of a discoid rash that is characteristic of a patient with SLE. It is included in this project courtesy of www.googleimages.com]] | ||
*Photosensitivity | *Photosensitivity | ||
| Line 101: | Line 101: | ||
*'''<u>Heredity</u>'''- There is a high prevalence of SLE in first-degree relatives. The immune abnormalities associated with SLE can be triggered by both internal and external factors. | *'''<u>Heredity</u>'''- There is a high prevalence of SLE in first-degree relatives. The immune abnormalities associated with SLE can be triggered by both internal and external factors. | ||
*<u>'''Stress'''</u>- can provoke changes in the neuroendocrine system that changes the function of immune system cells | *<u>'''Stress'''</u>- can provoke changes in the neuroendocrine system that changes the function of immune system cells | ||
*<u>'''Bacterial or viral infection'''</u>- The Epstein-Barr virus has been determined a risk factor for the development of SLE. | *<u>'''Bacterial or viral infection'''</u>- The Epstein-Barr virus has been determined a risk factor for the development of SLE. | ||
*'''<u>Sunlight or UV exposure</u>''' | *'''<u>Sunlight or UV exposure</u>''' | ||
*<u>'''Immunizations '''</u> | *<u>'''Immunizations '''</u> | ||
*'''<u>Pregnancy</u>'''- The evidence about whether or not pregnancy can cause | *'''<u>Pregnancy</u>'''- The evidence about whether or not pregnancy can cause exacerbations is very inconclusive because some studies have found that pregnancy does affect the course of SLE, while others have found that it has no affect on the disease. | ||
*<u>'''Abnormal levels of estrogen'''</u>- There is a higher incidence of SLE among women who take low-dose contraceptives. | *<u>'''Abnormal levels of estrogen'''</u>- There is a higher incidence of SLE among women who take low-dose contraceptives. | ||
*'''<u>Certain drugs</u>'''- Drugs such as hydralazin, anticonvulsants, | *'''<u>Certain drugs</u>'''- Drugs such as hydralazin, anticonvulsants, penicillin, sulfa drugs, and oral contraceptives can change the cellular responsiveness and immunogenicity of self-antigens and therefore make a person more susceptible to SLE.<ref name="Goodman et al" /> | ||
== Systemic Involvement == | == Systemic Involvement == | ||
| Line 119: | Line 119: | ||
*Arthritis- typically affects hand, wrists, and knees | *Arthritis- typically affects hand, wrists, and knees | ||
* | *Arthralgia | ||
*Tenosynovitis | *Tenosynovitis | ||
*Tendon ruptures | *Tendon ruptures | ||
| Line 181: | Line 181: | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
The medical management for SLE is primarily drug therapy and is based upon the patients symptoms and systemic involvement. In addition to drug therapy, prevention is also very important when dealing with SLE. For patients with photosensitivities, flare-ups can be reduced if patients are cautious about the amount of sunlight or UV light that they are exposed to. Patients with SLE are also encouraged to lead a healthy lifestyle that includes: smoking cessation, controlling alcohol consumption, weight management, and regular exercise.<ref name="Goodman et al" /><ref name="Bertsias et al" /> Exercise is beneficial for patients with SLE because it decreases their muscle weakness while simultaneously increases their muscle endurance. Patients with SLE are also encouraged to participate in support groups, ensure they are taking the correct dosages and amounts of medications, and ensuring they visit medical professionals regularly.<ref name="Goodman et al" /> | The medical management for SLE is primarily drug therapy and is based upon the patients symptoms and systemic involvement. In addition to drug therapy, prevention is also very important when dealing with SLE. For patients with photosensitivities, flare-ups can be reduced if patients are cautious about the amount of sunlight or UV light that they are exposed to. Patients with SLE are also encouraged to lead a healthy lifestyle that includes: smoking cessation, controlling alcohol consumption, weight management, and regular exercise.<ref name="Goodman et al" /><ref name="Bertsias et al" /> Exercise is beneficial for patients with SLE because it decreases their muscle weakness while simultaneously increases their muscle endurance. Patients with SLE are also encouraged to participate in support groups, ensure they are taking the correct dosages and amounts of medications, and ensuring they visit medical professionals regularly.<ref name="Goodman et al" /> | ||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Physical therapists can play an important role for patients with SLE during and between exacerbations. The | Physical therapists can play an important role for patients with SLE during and between exacerbations. The patient's need for physical therapy will vary greatly depending on the systems involved. | ||
*<u>'''Education:'''</u>''' '''It is essential for patients with skin lesions to have appropriate education on the best way to care for their skin and to ensure they do not experience additional skin breakdown. | *<u>'''Education:'''</u>''' '''It is essential for patients with skin lesions to have appropriate education on the best way to care for their skin and to ensure they do not experience additional skin breakdown. | ||
*<u>'''Aerobic Exercise:'''</u> One of the most common impairments that patients with SLE experience is generalized fatigue that can limit their activities throughout the day.<ref name="Goodman et al" /> In a study by Tench et al., it was determined that graded aerobic exercise programs are more successful than relaxation techniques in decreasing the fatigue levels of patients with SLE. Aerobic activity caused many of them to feel "much better" or "very much better" at the conclusion of the study. The aerobic exercise program consisted of 30-50 minutes of aerobic activity (walking/swimming/cycling) with a heart rate corresponding to 60% of the patient's peak oxygen consumption.<ref name="Tench et al ">Tench CM, McCarthy J, McCurdie I, White PD, D'Cruz DP. Fatigue in systemic lupus erythematosus: a randomized control trial of exercise. Rheumatology; 42: 1050-1054. 2003.</ref> Another study, completed by Ramsey- Goldman et al., concluded that both aerobic exercise and range of motion/muscle strengthening exercises can increase the energy level, cardiovascular fitness, functional status, and muscle strength in patients with SLE. In this study, the patients completed aerobic exercise for 20-30 minutes at 70-80% of their | *<u>'''Aerobic Exercise:'''</u> One of the most common impairments that patients with SLE experience is generalized fatigue that can limit their activities throughout the day.<ref name="Goodman et al" /> In a study by Tench et al., it was determined that graded aerobic exercise programs are more successful than relaxation techniques in decreasing the fatigue levels of patients with SLE. Aerobic activity caused many of them to feel "much better" or "very much better" at the conclusion of the study. The aerobic exercise program consisted of 30-50 minutes of aerobic activity (walking/swimming/cycling) with a heart rate corresponding to 60% of the patient's peak oxygen consumption.<ref name="Tench et al">Tench CM, McCarthy J, McCurdie I, White PD, D'Cruz DP. Fatigue in systemic lupus erythematosus: a randomized control trial of exercise. Rheumatology; 42: 1050-1054. 2003.</ref> Another study, completed by Ramsey- Goldman et al., concluded that both aerobic exercise and range of motion/muscle strengthening exercises can increase the energy level, cardiovascular fitness, functional status, and muscle strength in patients with SLE. In this study, the patients completed aerobic exercise for 20-30 minutes at 70-80% of their maximum heart rate 3 times per week. The patients who completed range of motion and muscle strengthening activities met 3 times a week for 50 minutes sessions.<ref name="Ramsey-Goldman et al">Ramsey-Goldman GR, Schilling EM, Dunlop D, Langman C, Greenland P, Thomas RJ, Chang RW. A pilot study on the effects of exercise in patients with systemic lupus erythematosus. Arthritis Care and Research; 13(5): 262-269. 2000.</ref> | ||
*<u>'''Energy Conservation:'''</u> Physical therapists can educate patients on appropriate energy conservation techniques and the best ways to protect joints that are susceptible to damage. | *<u>'''Energy Conservation:'''</u> Physical therapists can educate patients on appropriate energy conservation techniques and the best ways to protect joints that are susceptible to damage. | ||
*Additionally, physical therapists should be aware of signs and symptoms that suggest a progression of SLE including those associated with avascular necrosis, kidney involvement, and neurological involvement.<ref name="Goodman et al" /> | *Additionally, physical therapists should be aware of signs and symptoms that suggest a progression of SLE including those associated with avascular necrosis, kidney involvement, and neurological involvement.<ref name="Goodman et al" /> | ||
| Line 198: | Line 198: | ||
Sometimes used in addition to medical treatment, alternative treatments are used to treat symptoms caused SLE. These alternative treatments include: | Sometimes used in addition to medical treatment, alternative treatments are used to treat symptoms caused SLE. These alternative treatments include: | ||
*Homeopathy [[Image:Acupuncture-to-body.jpg|right|250x200px]] | *Homeopathy [[Image:Acupuncture-to-body.jpg|right|250x200px]] | ||
*Chiropractic | *Chiropractic | ||
*Traditional Chinese medicines (acupuncture and Tai Chi) | *Traditional Chinese medicines (acupuncture and Tai Chi) | ||
| Line 220: | Line 220: | ||
== Case Reports == | == Case Reports == | ||
''A Case Report of a Very Late-Onset Systemic Lupus Erythematous'' [http://www.clinicalgeriatrics.com/articles/A-Case-Report-a-Very-Late-Onset-Systemic-Lupus-Erythematous http://www.clinicalgeriatrics.com] | ''A Case Report of a Very Late-Onset Systemic Lupus Erythematous'' [http://www.clinicalgeriatrics.com/articles/A-Case-Report-a-Very-Late-Onset-Systemic-Lupus-Erythematous http://www.clinicalgeriatrics.com] | ||
''Development and management of systemic lupus erythematosus in an HIV-infected man with Hepatitis C and B | ''Development and management of systemic lupus erythematosus in an HIV-infected man with Hepatitis C and B co-infection followed by interferon therapy: a case report'' [http://www.jmedicalcasereports.com/content/pdf/1752-1947-0003-0000007289.pdf http://www.jmedicalcasereports.com] | ||
''Case Report: Multiple Sclerosis and SLE Revisited'' [http://www.medicaljournal-ias.org/12_3/Bhigjee.pdf http://www.medicaljournal-ias.org/12_3/Bhigjee.pdf] | ''Case Report: Multiple Sclerosis and SLE Revisited'' [http://www.medicaljournal-ias.org/12_3/Bhigjee.pdf http://www.medicaljournal-ias.org/12_3/Bhigjee.pdf] | ||
== Resources <br> == | == Resources <br> == | ||
| Line 232: | Line 232: | ||
''Medline Plus: Lupus'' [http://www.nlm.nih.gov/medlineplus/lupus.html http://www.nlm.nih.gov/medlineplus/lupus.html] | ''Medline Plus: Lupus'' [http://www.nlm.nih.gov/medlineplus/lupus.html http://www.nlm.nih.gov/medlineplus/lupus.html] | ||
''WebMD: Lupus'' [http://lupus.webmd.com/ http://lupus.webmd.com/] | ''WebMD: Lupus'' [http://lupus.webmd.com/ http://lupus.webmd.com/] | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
| Line 238: | Line 238: | ||
see tutorial on [[Adding PubMed Feed|Adding PubMed Feed]] | see tutorial on [[Adding PubMed Feed|Adding PubMed Feed]] | ||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | <rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | ||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
Revision as of 15:23, 3 April 2010
Original Editors - Alli Christian from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description
[edit | edit source]
Lupus erythematosus is an autoimmune disease that can manifest itself in several different ways including: discoid lupus erythematosus (DLE), systemic lupus erythematosus (SLE), drug-induced lupus, late-state lupus, and antiphopholipid antibody syndrome. With this condition, "the body creates antibodies against its own cells." These antibodies can be formed against many different tissues and components of the body including RBCs, neutrophils, platelets, lymphocytes, etc. For this reason, SLE can affect almost any area of a person's body.[1] Systemic lupus erythematosus is a chronic, rheumatic, inflammatory disease that can affect a person’s skin, joints, kidneys, lungs, heart, nervous system, blood, and mucous membranes. It does not affect all patients in the same way, so patients experience variable organ involvement after being diagnosed with SLE.[1] [2]
Prevalence[edit | edit source]
- Occurs in 15-24/100,000 people throughout the world[3]
- Most likely to occur in women of child-bearing age
- More common in those of African American, Hispanic, Asian, and Native American decent than in Caucasians[1]
- 10 to 15 times more likely in women compared to men
- Most people are diagnosed with the disease between the ages of 15 and 40[2]
- Rarely diagnosed in the elderly [3]
- Occurs in 10-20/100,000 children (depends on the population)
- About 15% of people diagnosed with SLE are younger than 18 years old, and when a person is diagnosed at an early age, the disease progresses more quickly and severely than if diagnosed after the age of 18.[4]
- More prevalent in those who have a family history of SLE than it is in the general population[1]
Characteristics/Clinical Presentation [edit | edit source]
SLE can affect many organs of the body, but it rarely affects them all. The following list includes common signs and symptoms of SLE in order of the most to least prevalent. All of the below symptoms might not be present at the initial diagnosis of SLE, but as the disease progresses more of a person’s organ systems become involved.
- “Constitutional symptoms (fever, malaise, fatigue, weight loss): most commonly fatigue and a low-grade fever
- Achy joints (arthralgia)
- Arthritis (inflamed joints)
- Arthralgia
- Skin rashes
- Pulmonary involvement (symptoms include: chest pain, difficulty breathing, and cough)
- Anemia
- Kidney involvement (lupus nephritis)
- Sensitivity to the sun or light (photosensitivity)
- Hair loss
- Raynaud’s phenomenon
- CNS involvement (seizures, headaches, peripheral neuropathy, cranial neuropathy, cerebral vascular accidents, organic brain syndrome, psychosis)
- Mouth, nose, or vaginal ulcers”
- Arthralgia and arthritis are the two symptoms most common symptoms of SLE[2]
- The most common signs and symptoms of SLE in children and adolescents are: "fever, fatigue, weight loss, arthritis, rash, and renal disease."[4]
Associated Co-morbidities[edit | edit source]
- About 30% of people who have been diagnosed with SLE also have been diagnosed with fibromyalgia.[2]
- Atherosclerosis[5] [6]
- Lupus Nephritis- leads to End Stage Renal Disease (ESRD)
- Anemia[7]
- Some types of cancers (especially non-Hodgkin's lymphoma and lung cancer) [6][8]
- Infections
- Hypertension
- Dyslipidemia
- Diabetes Mellitus
- Osteoporosis
- Avascular Necrosis [6]
Medications[edit | edit source]
- Analgesics[1]: These medications are used to control the pain that a patient has to endure from the pain of arthralgia, arthritis, and ulcers that SLE can cause.[3]
- Non-Steroidal Anti-inflammatory Drugs (NSAIDS): These medications help to decrease tissue inflammation, and therefore decrease the patient’s joint and muscle pain.
- Anti-malarials: These medications are used to treat a patient's arthritic, musculocutaneous, and renal symptoms that are associated with SLE.
- Chloroquine (Aralen)[1][3]
- Hydroxychloroquine (Plaquenil)[3] - Corticosteroids[2]: These drugs are usually only prescribed to patients with severe SLE whose signs and symptoms are not improving with any other drug therapy. Corticosteroids can give the patient relief from constitutional symptoms, arthritis, and cutaneous problems caused from SLE.
- Immunosuppressant Agents: These drugs are used to decrease inflammation, treat lupus nephritis, and suppress the patient's immune system.
- Azathioprine (Imuran)
- Cyclophosphamide (Cytoxan)[1][3]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
According to the American Rheumatism Association, a patient must exhibit at least 4 of the following criteria concurrently or successively to be diagnosed with systemic lupus erythematosus.
- "Abnormal titer of antinuclear antibodies (ANAs)
- Butterfly (malar) rash
- Discoid rash
- Hemolytic anemia, leukopenia, lymphopenia, thrombocytopenia
- Neurologic disorder: seizures or psychosis
- Non-erosive arthritis of two or more peripheral joints characterized by tenderness, swelling, or effusion
- Oral or nasopharyngeal ulcerations
- Photosensitivity
- Pleuritis or pericarditis
- Positive lupus erythematosus cell preparations, anti DNA, or anti-splice sosomal test or chronic false-positive serologic test for syphilis
- Renal disorder: profuse proteinuria (>0.5 grams/day) or excessive cellular casts in urine."[1]
The lab tests completed may include:
- Complete Blood Count: This blood test reveals a patient's total number of red blood cells, white blood cells, platelets, and hemoglobin. Low white blood cell or platelet counts can be indicative of SLE, whereas low red blood cell counts can be indicate of anemia which commonly occurs in conjunction with SLE.
- Erythrocyte Sedimentation Rate: An elevated erythrocyte sedimentation rate can reveal a systemic problem. This test is not specific to SLE, but it can reveal that the patient could potentially have this disease if this test is positive.
- Kidney and Liver Tests: These tests are completed to determine if a patient's kidneys and liver are functioning properly because SLE can affect these systemic organs.
- Urinalysis: This test is performed to determine if there are proteins or red blood cells present in a patient's urine. If so, this could indicate that the kidneys are damaged, potentially from SLE.
- ANA test: A positive test reveals that a patient could potentially have SLE, but other infections and diseases can cause this test to be positive as well. If positive, further testing is necessary to determine if the positive results occurred due to SLE.
- Chest X-ray: This test is performed to determine if there is inflammation present in the patient's lungs or excessive fluid surrounding his/her heart.
- Syphilis Test: A false-positive syphilis test can reveal that a patient has anti-phospholipids present, and this false-positive test result is indicative that the patient could have SLE.[8]
Causes[edit | edit source]
There is no known cause of SLE, but research states that the interaction between a person's genetic make-up, immune system, hormonal balance, and environment could potentially cause SLE. At this time, autoimmunity is thought to be the primary causative factor of SLE.
There are certain factors that can predispose a patient to SLE including:
- Heredity- There is a high prevalence of SLE in first-degree relatives. The immune abnormalities associated with SLE can be triggered by both internal and external factors.
- Stress- can provoke changes in the neuroendocrine system that changes the function of immune system cells
- Bacterial or viral infection- The Epstein-Barr virus has been determined a risk factor for the development of SLE.
- Sunlight or UV exposure
- Immunizations
- Pregnancy- The evidence about whether or not pregnancy can cause exacerbations is very inconclusive because some studies have found that pregnancy does affect the course of SLE, while others have found that it has no affect on the disease.
- Abnormal levels of estrogen- There is a higher incidence of SLE among women who take low-dose contraceptives.
- Certain drugs- Drugs such as hydralazin, anticonvulsants, penicillin, sulfa drugs, and oral contraceptives can change the cellular responsiveness and immunogenicity of self-antigens and therefore make a person more susceptible to SLE.[1]
Systemic Involvement[edit | edit source]
There are many visceral systems can be affected from SLE, but the extent to the bodies' involvement differs from person to person. Some people diagnosed with SLE have only few visceral systems involved, while others have numerous systems that have been affected by the disease.
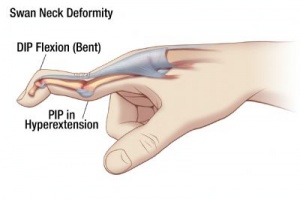
Musculoskeletal System:
- Arthritis- typically affects hand, wrists, and knees
- Arthralgia
- Tenosynovitis
- Tendon ruptures
- Swan-neck deformity
- Ulnar drift
Cardiopulmonary System:
- Pleuritis
- Pericarditis
- Dyspnea
- Myocarditis
- Endocarditis
- Tachycarditis
- Pneumonitis
Central Nervous System:
- Emotional instability
- Psychosis
- Seizures
- Cerebrovascular Accidents
- Cranial neuropathy
- Peripheral neuropathy
- Organic brain syndrome
Renal System:
- Usually SLE affects the glomerulus
- Hematuria
- Proteinuria
- Kidney failure[1]
Cutaneous System:
- Calcinosis
- Cutaneous vasculitis
- Hair loss
- Raynaud's phenomenon
- Mucosal ulcers
- Petechiae
Blood Disorders:
- Anemia
- Thrombocytopenia
- Leukopenia
- Neutropenia
- Thrombosis
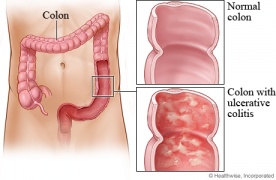
Gastrointestinal System:
- Ulcerative colitis
- Chrone's disease
- Peritonitis
- Ascites
- Pancreatitis
- Peptic ulcers
- Autoimmune Hepatitis [9]
Medical Management (current best evidence)[edit | edit source]
The medical management for SLE is primarily drug therapy and is based upon the patients symptoms and systemic involvement. In addition to drug therapy, prevention is also very important when dealing with SLE. For patients with photosensitivities, flare-ups can be reduced if patients are cautious about the amount of sunlight or UV light that they are exposed to. Patients with SLE are also encouraged to lead a healthy lifestyle that includes: smoking cessation, controlling alcohol consumption, weight management, and regular exercise.[1][6] Exercise is beneficial for patients with SLE because it decreases their muscle weakness while simultaneously increases their muscle endurance. Patients with SLE are also encouraged to participate in support groups, ensure they are taking the correct dosages and amounts of medications, and ensuring they visit medical professionals regularly.[1]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapists can play an important role for patients with SLE during and between exacerbations. The patient's need for physical therapy will vary greatly depending on the systems involved.
- Education: It is essential for patients with skin lesions to have appropriate education on the best way to care for their skin and to ensure they do not experience additional skin breakdown.
- Aerobic Exercise: One of the most common impairments that patients with SLE experience is generalized fatigue that can limit their activities throughout the day.[1] In a study by Tench et al., it was determined that graded aerobic exercise programs are more successful than relaxation techniques in decreasing the fatigue levels of patients with SLE. Aerobic activity caused many of them to feel "much better" or "very much better" at the conclusion of the study. The aerobic exercise program consisted of 30-50 minutes of aerobic activity (walking/swimming/cycling) with a heart rate corresponding to 60% of the patient's peak oxygen consumption.[10] Another study, completed by Ramsey- Goldman et al., concluded that both aerobic exercise and range of motion/muscle strengthening exercises can increase the energy level, cardiovascular fitness, functional status, and muscle strength in patients with SLE. In this study, the patients completed aerobic exercise for 20-30 minutes at 70-80% of their maximum heart rate 3 times per week. The patients who completed range of motion and muscle strengthening activities met 3 times a week for 50 minutes sessions.[11]
- Energy Conservation: Physical therapists can educate patients on appropriate energy conservation techniques and the best ways to protect joints that are susceptible to damage.
- Additionally, physical therapists should be aware of signs and symptoms that suggest a progression of SLE including those associated with avascular necrosis, kidney involvement, and neurological involvement.[1]
Alternative/Holistic Management (current best evidence) [edit | edit source]
Sometimes used in addition to medical treatment, alternative treatments are used to treat symptoms caused SLE. These alternative treatments include:
- Homeopathy
- Chiropractic
- Traditional Chinese medicines (acupuncture and Tai Chi)
- Ayurveda
- Naturopathy
- Massage therapy
- Meditation
- Biofeedback- In conjunction with medication, biofeedback has been shown to decrease a patient's pain and stress levels
- Herbs and Supplements
- Acupuncture- Some research reveals that acupuncture can decrease a patient's arthritis pain[9]
Differential Diagnosis[edit | edit source]
- Viral Infections
- Bacterial Infections
- Malignancies
- Rheumatoid Arthritis
- Vasculitis [4]
- Multiple Sclerosis [12]
Case Reports[edit | edit source]
A Case Report of a Very Late-Onset Systemic Lupus Erythematous http://www.clinicalgeriatrics.com
Development and management of systemic lupus erythematosus in an HIV-infected man with Hepatitis C and B co-infection followed by interferon therapy: a case report http://www.jmedicalcasereports.com
Case Report: Multiple Sclerosis and SLE Revisited http://www.medicaljournal-ias.org/12_3/Bhigjee.pdf
Resources
[edit | edit source]
Lupus Foundation of America www.lupus.org
Medline Plus: Lupus http://www.nlm.nih.gov/medlineplus/lupus.html
WebMD: Lupus http://lupus.webmd.com/
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd edition. St. Louis, Missouri: Saunders Elsevier, 2009.
- ↑ 2.0 2.1 2.2 2.3 Goodman CC and Synder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th edition. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Laranzo D. Elderly-onset systemic lupus erythematosus. Drugs and Aging; 24 (9):701-715. 2007.
- ↑ 4.0 4.1 4.2 Tucker LB. Making the diagnosis of systemic lupus erythematosus in children and adolescents. Lupus; 16: 546-549. 2007.
- ↑ Becker-Merok A, Nossent JC. Prevalence, predictors, and outcomes of vascular damamge in systemic lupus erythematosus. Lupus; 18: 508-515. 2009.
- ↑ 6.0 6.1 6.2 6.3 Bertsias G, Gordon C, Boumpas DT. Clinical trials in systemic lupus erythematosus (SLE): lessons from the past as we proceed to the future- the EULAR recommendations for the management of SLE and the use of end-points in clinical trials. Lupus; 17: 437-442. 2008.
- ↑ Wingard R. Increased risk of anemia in dialysis patients with comorbid diseases. Nephrology Nursing Journal; 31 (2): 211-214. 2004.
- ↑ 8.0 8.1 Medical Foundation for Medical Education and Research. Mayo Clinic: Lupus Page. www.mayoclinic.com. Updated October 20, 2009. Accessed February 17, 2010.
- ↑ 9.0 9.1 Lupus Foundation of America. How lupus affects the body page. Website updated: 2010. Website accessed: February 17, 2010.
- ↑ Tench CM, McCarthy J, McCurdie I, White PD, D'Cruz DP. Fatigue in systemic lupus erythematosus: a randomized control trial of exercise. Rheumatology; 42: 1050-1054. 2003.
- ↑ Ramsey-Goldman GR, Schilling EM, Dunlop D, Langman C, Greenland P, Thomas RJ, Chang RW. A pilot study on the effects of exercise in patients with systemic lupus erythematosus. Arthritis Care and Research; 13(5): 262-269. 2000.
- ↑ Bhiglee AI, Bill PL. Case Report: Multiple sclerosis and SLE revisited. Medical Journal of Islamic Academy of Sciences; 12 (3): 79-84. 1999.