Suprascapular Nerve Palsy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 23: | Line 23: | ||
In rare cases, systemic conditions like systemic lupus erthymatosus (SLE) and rheumatoid arthritis (RA) can result in suprascapular nerve palsy.<ref>Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. Int Orthop. 2002;26(6):339-43.</ref> | In rare cases, systemic conditions like systemic lupus erthymatosus (SLE) and rheumatoid arthritis (RA) can result in suprascapular nerve palsy.<ref>Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. Int Orthop. 2002;26(6):339-43.</ref> | ||
== | == Clinical presentation == | ||
Usually, patients will present with dull aching pain over the superior or posterolateral aspect of the shoulder. Pain might radiate down the upper limb or to the neck. Cross-body adduction and internal rotation may increase pain. Pain will not be present if nerve injury is distal to spinoglenoid notch. Almost 40% of cases present with associated trauma to the shoulder. This is common in athletes involved in repeated overhead activities. Patients with history of trauma can also report a sense of instability in the shoulder. | |||
The most common clinical sign of suprascapular nerve palsy is atrophy of the supraspinatus and/or infraspinatus muscles. If the injury is proximal to the spinoglenoid notch, both muscles will be atrophied and if the injury is distal to the spinoglenoid notch, the supraspinatus is spared and only the infraspinatus will present with atrophy. | |||
== Management == | == Management == | ||
Revision as of 06:25, 18 November 2021
Original Editor - Arnold Fredrick D'Souza
Top Contributors - Arnold Fredrick D'Souza, Kim Jackson, Joseph Zahn and Naomi O'Reilly
Introduction[edit | edit source]
The suprascapular nerve is a mixed nerve of the upper limb. Suprascapular nerve injury is experiencing an increase in clinical significance due to its role in shoulder pain and upper limb weakness.[1]
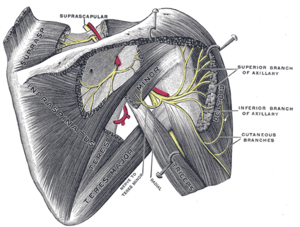
Anatomy[edit | edit source]
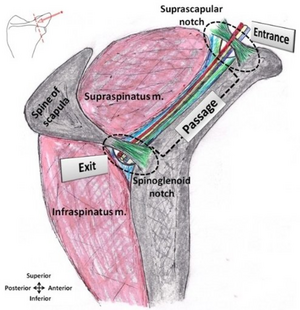
The suprascapular nerve branches out from the upper trunk of the brachial plexus. Its nerve roots are C5 and C6. Sporadically, it may have roots from C4 as well. From the posterior triangle of the neck, the nerve goes over the upper part of the scapula, then downward and laterally, parallel to the omohyoid muscle belly. It then passes below the suprascapular ligament, through the suprascapular notch and into the supraspinous fossa where it innervates supraspinatus and continues. Through here it curves around the spinous process of the scapula, through the spinoglenoid notch and then into the infraspinous fossa where it innervates infraspinatus.[1]The suprascapular nerve also provides sensory innervation to the glenohumeral and acromioclavicular joint.[2]
Etiology[edit | edit source]
Compression neuropathy resulting from nerve entrapment is the most common cause of suprascapular nerve palsy. The common sites of nerve entrapment are the suprascapular notch and the spinoglenoid notch.[3]
Trauma to the shoulder resulting from fractures of scapula, clavicle and proximal humerus can significantly damage the suprascapular nerve.[4][5]
Post-surgical complications after open or athroscopic shoulder surgery can lead to suprascapular nerve damage.[6]
Scapula dyskinesia can lead to suprascapular nerve palsy.[7]
Tumors, cysts and other space-occupying lesions around the shoulder can compress the suprascapular nerve.[8]
In rare cases, systemic conditions like systemic lupus erthymatosus (SLE) and rheumatoid arthritis (RA) can result in suprascapular nerve palsy.[9]
Clinical presentation[edit | edit source]
Usually, patients will present with dull aching pain over the superior or posterolateral aspect of the shoulder. Pain might radiate down the upper limb or to the neck. Cross-body adduction and internal rotation may increase pain. Pain will not be present if nerve injury is distal to spinoglenoid notch. Almost 40% of cases present with associated trauma to the shoulder. This is common in athletes involved in repeated overhead activities. Patients with history of trauma can also report a sense of instability in the shoulder.
The most common clinical sign of suprascapular nerve palsy is atrophy of the supraspinatus and/or infraspinatus muscles. If the injury is proximal to the spinoglenoid notch, both muscles will be atrophied and if the injury is distal to the spinoglenoid notch, the supraspinatus is spared and only the infraspinatus will present with atrophy.
Management[edit | edit source]
Surgical[edit | edit source]
Physiotherapy[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Kostretzis L, Theodoroudis I, Boutsiadis A, Papadakis N, Papadopoulos P. Suprascapular Nerve Pathology: A Review of the Literature. Open Orthop J. 2017 Feb 28;11:140-53.
- ↑ Avery BW, Pilon FM, Barclay JK. Anterior coracoscapular ligament and suprascapular nerve entrapment. Clin Anat. 2002 Nov;15(6):383-6.
- ↑ Gosk J, Urban M, Rutowski R. Entrapment of the suprascapular nerve: anatomy, etiology, diagnosis, treatment. Ortop Traumatol Rehabil. 2007 Jan-Feb;9(1):68-74.
- ↑ Zoltan JD. Injury to the suprascapular nerve associated with anterior dislocation of the shoulder: case report and review of the literature. J Trauma. 1979 Mar;19(3):203-6.
- ↑ Solheim LF, Roaas A. Compression of the suprascapular nerve after fracture of the scapular notch. Acta Orthop Scand. 1978 Aug;49(4):338-40.
- ↑ Mallon WJ, Bronec PR, Spinner RJ, Levin LS. Suprascapular neuropathy after distal clavicle excision. Clin Orthop Relat Res. 1996 Aug;(329):207-11
- ↑ Reece CL, Varacallo M, Susmarski A. Suprascapular Nerve Injury. [Updated 2021 Jul 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559151/
- ↑ Sjödén GO, Movin T, Güntner P, Ingelman-Sundberg H. Spinoglenoid bone cyst causing suprascapular nerve compression. J Shoulder Elbow Surg. 1996 Mar-Apr;5(2 Pt 1):147-9.
- ↑ Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. Int Orthop. 2002;26(6):339-43.