Subjective Assessment of the Lumbar Spine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
== '''Introduction ''' == | == '''Introduction ''' == | ||
Low back pain (LBP) is a common, disabling condition with both musculoskeletal and non musculoskeletal contributions. It has been reported that greater than 80% of individuals will experience LBP within their lifetime and 20-30% of individuals are affected with these symptoms at any point in time<ref name=" | Low back pain (LBP) is a common, disabling condition with both musculoskeletal and non musculoskeletal contributions. It has been reported that greater than 80% of individuals will experience LBP within their lifetime and 20-30% of individuals are affected with these symptoms at any point in time<ref name="13">Freburger JK, Holmes GM, et al. The rising prevalence of chronic LBP. Arch Intern Med. 2009. 169(3):251-8.</ref>. Katz et al. reported the cumulative cost to manage this condition is greater than 100 billion dollars per year<ref name="23">Katz, J. et al. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006. 88(2):21-4.</ref>. Given the high economic costs associated with LBP it is imperative for the clinician to obtain the necessary information needed to determine the appropriate plan of care, either outside referral or Physical Therapy treatment, for their patient. Matching appropriate interventions based on a patient’s symptoms has been shown to decrease healthcare costs in patients with LBP<ref name="6">Brennan, G. et al. Identifying Subgroups of Patients With Acute/Sub acute “Nonspecific” Low Back Pain: Results of a Randomized Clinical Trial. Spine. 2006.</ref><ref name="16">Fritz, J. et al. Subgrouping Patients With Low Back Pain: Evolution of a Classification Approach to Physical Therapy. JOSPT. 2007. 37(6):290-302.</ref>. | ||
The patient interview is the first opportunity for the clinician to gather information regarding the patient’s condition. Information gathered during the subjective history can increase the clinician’s confidence in either ruling in or ruling out a suspected condition through the utilization of likelihood ratios (LR) to determine the probability of a condition’s presence or absence. After determining the condition responsible for a patient’s LBP symptoms, the subjective examination may help determine which referral or intervention is warranted. <br> | The patient interview is the first opportunity for the clinician to gather information regarding the patient’s condition. Information gathered during the subjective history can increase the clinician’s confidence in either ruling in or ruling out a suspected condition through the utilization of likelihood ratios (LR) to determine the probability of a condition’s presence or absence. After determining the condition responsible for a patient’s LBP symptoms, the subjective examination may help determine which referral or intervention is warranted. <br> | ||
| Line 14: | Line 14: | ||
== '''Subjective Examination''' == | == '''Subjective Examination''' == | ||
A thorough and detailed subjective history and review of systems allows the clinician to gather information regarding the location, quality, severity, irritability, and behavior of a patient’s symptoms. This information is then assimilated to identify patients appropriate for Physical Therapy and those who require a referral to an outside healthcare provider. The subjective examination facilitates this decision by providing a strong diagnostic resource given the patient’s presenting symptoms. Hampton, et al. reported the subjective history alone assisted in the medical diagnosis of 83% of patients seen in a primary care practice<ref name=" | A thorough and detailed subjective history and review of systems allows the clinician to gather information regarding the location, quality, severity, irritability, and behavior of a patient’s symptoms. This information is then assimilated to identify patients appropriate for Physical Therapy and those who require a referral to an outside healthcare provider. The subjective examination facilitates this decision by providing a strong diagnostic resource given the patient’s presenting symptoms. Hampton, et al. reported the subjective history alone assisted in the medical diagnosis of 83% of patients seen in a primary care practice<ref name="18">Hampton, J. et al. Relative Contributions of History-taking, Physical Examination, and Laboratory Investigation to Diagnosis and Management of Medical Outpatients. BMJ. 1975. 2:486-489.</ref>. Specifically, 4 subjective examination questions have demonstrated a sensitivity of 1.0 in screening for cancer in patients with LBP<ref name="11">Deyo, R. et al. Cancer as a cause of low back pain. J Gen Int Med. 1988. 3:230-239.</ref>. Despite its importance authors have reported the average time given to a patient to explain their symptoms without interruption is 18 seconds and once interrupted patients often do not return to their previous complaints<ref name="4">Beckman HB, Frankel RM. The use of videotape in internal medicine training. J Gen Intern Med. 1994 Sep;9(9):517-21.</ref>. In contrast, an uninterrupted patient only needs 150 seconds to fully express their concerns<ref name="4" />. | ||
Based on the information gathered from the subjective examination, the clinician will determine which tests to perform designed to confirm or refute their hypothesis on the source of a patient’s symptoms. A selection of the most appropriate questions, with the highest diagnostic utility, will increase the clinician’s confidence in ruling in or out sinister disorders. The following paragraphs will describe questions demonstrating the strongest shifts in probability of a condition being present (+ LR) or absent (-LR). These shifts in probability provide an excellent resource to the clinician treating patients with LBP. <br> | Based on the information gathered from the subjective examination, the clinician will determine which tests to perform designed to confirm or refute their hypothesis on the source of a patient’s symptoms. A selection of the most appropriate questions, with the highest diagnostic utility, will increase the clinician’s confidence in ruling in or out sinister disorders. The following paragraphs will describe questions demonstrating the strongest shifts in probability of a condition being present (+ LR) or absent (-LR). These shifts in probability provide an excellent resource to the clinician treating patients with LBP. <br> | ||
| Line 20: | Line 20: | ||
== '''Risk Factors ''' == | == '''Risk Factors ''' == | ||
The symptoms reported by patients collected through the intake paperwork, review of systems, and subjective examination can assist in clinical hypothesis generation and identification of risk factors shown to influence the prognosis of a patient with LBP. A recent review of the evidence and epidemiological data reports risk factors for LBP include advancing age with first onset between 30-40, sedentary lifestyle, history of back surgery, occupational demands, smoking, depression, corticosteroid use, and obesity<ref name=" | The symptoms reported by patients collected through the intake paperwork, review of systems, and subjective examination can assist in clinical hypothesis generation and identification of risk factors shown to influence the prognosis of a patient with LBP. A recent review of the evidence and epidemiological data reports risk factors for LBP include advancing age with first onset between 30-40, sedentary lifestyle, history of back surgery, occupational demands, smoking, depression, corticosteroid use, and obesity<ref name="14">Fritz, J. et al. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002 Oct;82(10):973-83.</ref><ref name="21">Hill, J. et al. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther. 2011. 91(5):712-21</ref><ref name="37">Shiri, R. et al. The association between obesity and low back pain: a meta analysis. Am J. Epidemiology. 2010. 171(2):135-154.</ref><ref name="38">Shiri, R. et al. The association between smoking and low back pain: a metal analysis. Am J Med. 2010. 123(1):87. e7-35.</ref>. Many of these variables have been correlated with an increased risk of developing LBP in population based studies. Further, studies have identified features that are associated with chronicity of symptoms, such as lower extremity radiating pain, low expectations for recovery, elevated initial pain score, coping style, fear, and psychosocial stress<ref name="26">Koes, B. et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010. 19(12):2075-94</ref><ref name="38" />. | ||
== '''Yellow Flags''' == | == '''Yellow Flags''' == | ||
Due to the multiple factors associated with pain and their relationship with behavior and personal beliefs, it is necessary to review additional details related to this interaction. Kendall defined yellow flags as factors which increase the risk of developing, or perpetuating long term disability and work loss associated with low back pain<ref name=" | Due to the multiple factors associated with pain and their relationship with behavior and personal beliefs, it is necessary to review additional details related to this interaction. Kendall defined yellow flags as factors which increase the risk of developing, or perpetuating long term disability and work loss associated with low back pain<ref name="21" /> including depression, pain catastrophizing, and elevated fear avoidance beliefs. Arroll et al. reported two questions, “During the past month have you been feeling down, depressed or hopeless?” and “During the past month have you been bothered by having little interest or pleasure in doing things?”, although lacking diagnostic properties (Specificity (Sp) .57-.67), improve our ability to screen (Sensitivity (Sn) .96-.97) for the presence of depression in patients with LBP<ref name="1">Arroll, B. et al. Effect of the addition of a "help" question to two screening questions on specificity for diagnosis of depression in general practice: diagnostic validity study. BMJ. 2005. 15. 331(7521):884.</ref>. In addition, asking patients when they would like assistance with these questions can help identify those patients benefiting from help today ((+) Likelihood ratio (LR) 17.5) or help in the future ((+) LR 7.9) for their depression. | ||
Elevated fear avoidance scores associated with the fear avoidance beliefs questionnaire (FABQ) have been associated with an exaggerated perception of pain and an elevated risk for chronic LBP symptoms<ref | Elevated fear avoidance scores associated with the fear avoidance beliefs questionnaire (FABQ) have been associated with an exaggerated perception of pain and an elevated risk for chronic LBP symptoms<ref name="14" />. Specifically, a FABQ Work score >34 and work score <29 produces a (+) LR 3.33 and (-) LR 0.08, respectively, for the development of chronic LBP symptoms. Calley et al. reported the utilization of a two question screen for fear avoidance behaviors including “Are you afraid physical activity will cause an increase in your LBP?” and “Are you afraid that moving your back will be harmful to you?” can be effective for identifying patients requiring further education on their LBP symptoms<ref name="8">Calley, D. et al. Identifying Patient Fear-Avoidance Beliefs by Physical Therapists Managing Patients With Low Back Pain. JOSPT. 2010. 40(12):774-783.</ref>. An education session devoted to improving a patient’s understanding of pain neurophysiology including nociception and central sensitization, as well as, understanding their thoughts and beliefs regarding their symptoms can improve outcomes in these patients<ref name="31">Main, C. et al. Psychologically Informed Practice for Management of Low Back Pain: Future Directions in Practice and Research. PT. 2011. 91:820-824.</ref><ref name="32">Moreley, S. Efficacy and effectiveness of cognitive behaviour therapy for chronic pain: Progress and some challenges. Pain. 2011. 152:S99–S106.</ref><ref name="33">Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. European Journal of Pain. 2004. 8:39-45.</ref><ref name="34">Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clinical Journal of Pain. 2004. 20:324-30</ref><ref name="40">Smeets, R. et al. Reduction of Pain Catastrophizing Mediates the Outcome of Both Physical and Cognitive-Behavioral Treatment in Chronic Low Back Pain. The J Pain. 2006. 7(4):261-271</ref>. Clinician’s should aim to reduce a patient’s focus on the patho-anatomical sources of their LBP (ex. herniated disc), educate the patient on the resiliency of the spine and limitations of imaging in LBP, and improve a patient’s self efficacy for management of their symptoms. | ||
<br> | <br> | ||
| Line 32: | Line 32: | ||
== '''Red Flags''' == | == '''Red Flags''' == | ||
Although uncommon, non musculoskeletal conditions may present as LBP in approximately 5% of patients presenting to primary care offices (see table)<ref>Deyo, R. et al. What Can the History and Physical Examination Tell Us About Low Back Pain? JAMA. 1992. 268(6):760-766.</ref><ref>Jarvik, J. et al. Diagnostic Evaluation of Low Back Pain with Emphasis on Imaging. Ann Intern Med. 2002;137:586-597.</ref>. Within this 5%, 1% are attributed to non mechanical disorders including cancer, infection, and inflammatory arthropathies; 1-2% are attributed to the viscera (abdominal aortic aneurysm (AAA), pelvic, renal, GI); and 2-3% are attributed to other diseases (Paget’s disease, parathyroid disease). | Although uncommon, non musculoskeletal conditions may present as LBP in approximately 5% of patients presenting to primary care offices (see table)<ref name="12">Deyo, R. et al. What Can the History and Physical Examination Tell Us About Low Back Pain? JAMA. 1992. 268(6):760-766.</ref><ref name="22">Jarvik, J. et al. Diagnostic Evaluation of Low Back Pain with Emphasis on Imaging. Ann Intern Med. 2002;137:586-597.</ref>. Within this 5%, 1% are attributed to non mechanical disorders including cancer, infection, and inflammatory arthropathies; 1-2% are attributed to the viscera (abdominal aortic aneurysm (AAA), pelvic, renal, GI); and 2-3% are attributed to other diseases (Paget’s disease, parathyroid disease). | ||
*Estimated 5% of LBP is caused by serious disease | *Estimated 5% of LBP is caused by serious disease | ||
| Line 41: | Line 41: | ||
== '''Cauda Equina Syndrome''' == | == '''Cauda Equina Syndrome''' == | ||
Cauda Equina Syndrome (CES) commonly involves a large midline lumbar disc herniation at L4/5, L5/S1, or less commonly L3/4 which impairs lumbosacral nerve function<ref>Small, S. et al. Orthopedic pitfalls: cauda equina syndrome. American Journal of Emergency Medicine (2005) 23, 159–163</ref>. This disorder is most frequently seen in individuals aged 40-60 with a prevalence estimated at .04% of the population<ref | Cauda Equina Syndrome (CES) commonly involves a large midline lumbar disc herniation at L4/5, L5/S1, or less commonly L3/4 which impairs lumbosacral nerve function<ref name="39">Small, S. et al. Orthopedic pitfalls: cauda equina syndrome. American Journal of Emergency Medicine (2005) 23, 159–163</ref>. This disorder is most frequently seen in individuals aged 40-60 with a prevalence estimated at .04% of the population<ref name="39" />. Up to 70% of patients with this disorder will complain of a chronic history of LBP and may report symptoms including incontinence, loss of sphincter tone, saddle anesthesia, gait disturbances, unilateral or bilateral sciatica, and urinary retention depending on the severity and duration of symptoms. Early identification of CES is important considering surgical decompression is most successful in patients < 72 hours since onset<ref name="39" />. Each of these reported symptoms provide the clinician with additional information necessary to rule in or out this condition. Specifically, saddle anesthesia (Sn .75) and unilateral or bilateral sciatica (Sn. 80) may assist in the screening of this patient<ref name="27">Kostuik, J. et al. Cauda equina syndrome and lumbar disc herniation. Bone Joint Surg Am. 1986 Mar;68(3):386-91.</ref>. More importantly, the presence (Sp .95, +LR 9.9) or absence (Sn. 90, –LR .11) of urinary retention offers the greatest diagnostic utility for CES <ref name="12" /><ref name="27" />.<br> | ||
== '''Cancer''' == | == '''Cancer''' == | ||
The prevalence of cancer within the LBP population is estimated at 0.7%<ref | The prevalence of cancer within the LBP population is estimated at 0.7%<ref name="12" /><ref name="22" /> and although this condition is rare clinicians can increase their confidence in screening for this pathology by following the evidence supported in the literature. Henschke, N. et al.<ref name="20">Henschke, N. et al. Screening for malignancy in low back pain patients: a systematic review. Eur Spine J. 2007. 16:1673–1679.</ref> conducted a systematic review on 6 studies of 5,097 patients and found a prevalence ranging from .1 to 3.5%. A previous history of cancer (+LR 23) and clinician judgment consistent with cancer (+ 12.1) offered the best shift in post test probability of cancer being present. Conversely, a patient younger than 50 years of age demonstrated a (-) LR of .34 for the presence of cancer. See Table. Further, Deyo, R. et al.<ref name="11" /> demonstrated a four item cluster of age >50 years old, unexplained weight changes, a previous history of cancer, and no improvement with conservative care offered the best screening utility for cancer in patients with LBP (Sn 1.0, -LR .06 (0.0-.91)). In short, if a patient answers no to these historical items we can have increased confidence in our ability to rule out cancer as the source of a patient’s LBP symptoms. <br> | ||
'''TABLE - Henschke, N. et al. Screening for malignancy in low back pain patients: <br>a systematic review. Eur Spine J. 2007. 16:1673–1679.''' | '''TABLE - Henschke, N. et al. Screening for malignancy in low back pain patients: <br>a systematic review. Eur Spine J. 2007. 16:1673–1679.''' | ||
| Line 78: | Line 78: | ||
== '''[[Image:AS Lumbar Spine.jpg|frame|left|Radiograph findings of AS]]Ankylosing Spondylitis<br>''' == | == '''[[Image:AS Lumbar Spine.jpg|frame|left|Radiograph findings of AS]]Ankylosing Spondylitis<br>''' == | ||
Ankylosing Spondylitis (AS) is an inflammatory arthropathy most commonly occurring in males in their 20s and 30s with an estimated prevalence of 3%<ref | Ankylosing Spondylitis (AS) is an inflammatory arthropathy most commonly occurring in males in their 20s and 30s with an estimated prevalence of 3%<ref name="12" /><ref name="22" />. Radiographic evidence of ankylosis may not be present until several years following initial onset of back pain or stiffness<ref name="25" />. Given these findings a thorough history and subjective examination may help in early detection of AS. A past medical history significant for irritable bowel syndrome, crohn’s disease, psoriatic arthritis, and reactive arthritis are often found in patients with AS<ref name="9">Coronado R. et al. Spondyloarthritis in a patient with unilateral buttock pain and history of Crohn disease. PT. 2010. 90:784-792.</ref>. Inflammatory back pain (IBP) is a common sign associated with AS. Diagnostic variables of IBP include age < 40 years, > 3 month onset of symptoms, insidious onset, morning stiffness lasting at least 30 min, and improvement with exercise. These variables demonstrated a sensitivity of .95 and specificity of .85 if 4 of the 5 criteria were met<ref name="25" />. | ||
Specifically, patients with AS may complain of pain and stiffness longer than 3 months, morning stiffness lasting at least 30 minutes, no improvement of back pain with rest, awakening in the second half of the night because of back pain, and alternating buttock pain. If 3 of these 4 criteria are met then there is a (+) LR of 12.4 of AS being present<ref>Rudwaleit M, Metter A, Listing J, et al. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum 2006;54:569–78.</ref>. See Table 1. In addition, Gran, J. et al.17 reported 5 questions with diagnostic value: age < 40 years old, morning stiffness, improvement of symptoms with exercise, a gradual onset, and duration of symptoms > 3 months, offer small shifts in the probability of this condition being present. See Table 2. <br> | Specifically, patients with AS may complain of pain and stiffness longer than 3 months, morning stiffness lasting at least 30 minutes, no improvement of back pain with rest, awakening in the second half of the night because of back pain, and alternating buttock pain. If 3 of these 4 criteria are met then there is a (+) LR of 12.4 of AS being present<ref name="36">Rudwaleit M, Metter A, Listing J, et al. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum 2006;54:569–78.</ref>. See Table 1. In addition, Gran, J. et al.17 reported 5 questions with diagnostic value: age < 40 years old, morning stiffness, improvement of symptoms with exercise, a gradual onset, and duration of symptoms > 3 months, offer small shifts in the probability of this condition being present. See Table 2. <br> | ||
<br> | <br> | ||
| Line 154: | Line 154: | ||
== '''Lumbar Stenosis''' == | == '''Lumbar Stenosis''' == | ||
Lumbar spine stenosis (LSS) is estimated to represent 3% of patients with LBP and is most commonly found in older adults<ref | Lumbar spine stenosis (LSS) is estimated to represent 3% of patients with LBP and is most commonly found in older adults<ref name="12" /><ref name="22" />. Compression of neurologic structures within the spine can occur from soft tissue (disc, ligament) or bone structures. Up to 20% of asymptomatic individuals over 60 years old may demonstrate pathology on imaging. Symptoms of back pain and leg pain associated with lumbar stenosis must be differentiated from vascular claudication within this population. A patient reporting a minimal duration of rest required for symptoms to ease following activity may indicate a vascular versus neurological claudication. In a previous study, Katz, J. et al.<ref name="24">Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-41.</ref> reported on the diagnostic utility of historical items within the subjective examination (see table) with age >65 years old and severe leg pain offering the best screening utility for lumbar stenosis while the best diagnostic properties were found with relief of symptoms with sitting. | ||
'''TABLE - Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-41. <br>''' | '''TABLE - Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-41. <br>''' | ||
| Line 213: | Line 213: | ||
== '''[[Image:Lumbar disc herniation.png|left|Sagital view of L5/S1 HNP on MRI]]Lumbar Disc Herniations<br>''' == | == '''[[Image:Lumbar disc herniation.png|left|Sagital view of L5/S1 HNP on MRI]]Lumbar Disc Herniations<br>''' == | ||
A herniated lumbar disc is estimated to have a prevalence of 4% in the LBP population occurring most frequently in patients aged 30-55 years old<ref | A herniated lumbar disc is estimated to have a prevalence of 4% in the LBP population occurring most frequently in patients aged 30-55 years old<ref name="12" /><ref name="22" />. 95% of these herniations occur at the L4/5 and L5/S1 levels involving the L5 and S1 nerve roots, respectively. Commonly patients will report an acute onset of pain radiating below the knee. Vroomen, P. et al.<ref name="42">Vroomen, P. et al. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry 2002;72:630–634</ref> and Lauder, T. et al.<ref name="28">Lauder, T. et al. Effect of history and exam in predicting electrodiagnostic outcome among patients with suspected lumbosacral radiculopathy. Am J Phys Med. 2000. 79:60-68.</ref> reported on the diagnostic utility of historical examination items in patients with suspected lumbosacral nerve root symptoms. See Tables 1 and 2. The absence of sciatica, lower extremity pain not greater than back pain, and an absence of dermatomal pain offered the greatest value for screening for this pathology. <br> | ||
<br>'''TABLE 1 - Vroomen, P. et al. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry 2002;72:630–634''' | <br>'''TABLE 1 - Vroomen, P. et al. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry 2002;72:630–634''' | ||
| Line 263: | Line 263: | ||
== '''[[Image:L4 compression fracture.jpg|left|174x232px|L4 compression fracture on radiograph]]Vertebral Frature <br>''' == | == '''[[Image:L4 compression fracture.jpg|left|174x232px|L4 compression fracture on radiograph]]Vertebral Frature <br>''' == | ||
Spinal fractures are most common in older, white females occurring with a prevalence of 4% with less than 1% occurring secondary to trauma<ref | Spinal fractures are most common in older, white females occurring with a prevalence of 4% with less than 1% occurring secondary to trauma<ref name="12" /><ref name="22" />. This prevalence may be underestimated secondary to the asymptomatic nature of many osteoporotic fractures. | ||
The clinician’s ability to improve the probability of this pathology being present is supported by the literature from Henschke, N. et al. who reported moderate to high shifts in probability if a patient’s pain is associated with major trauma or pain and tenderness within the spine. See table. Further evidence<ref | The clinician’s ability to improve the probability of this pathology being present is supported by the literature from Henschke, N. et al. who reported moderate to high shifts in probability if a patient’s pain is associated with major trauma or pain and tenderness within the spine. See table. Further evidence<ref name="12" /><ref name="22" /> suggests a positive history of corticosteroid use may suggest the presence of vertebral fracture (Sp .95, (+) LR 12.0). | ||
<br> | <br> | ||
| Line 318: | Line 318: | ||
== '''Spinal Infection<br>''' == | == '''Spinal Infection<br>''' == | ||
Infections in the spine including osteomyelitis, septic discitis, abscess, and shingles most commonly present secondary to a previous infection elsewhere in the body. Infections known to cause spinal infection include IV drug use, skin infection, urinary tract infection, and skin infection occurring with an estimated prevalence of .01%<ref | Infections in the spine including osteomyelitis, septic discitis, abscess, and shingles most commonly present secondary to a previous infection elsewhere in the body. Infections known to cause spinal infection include IV drug use, skin infection, urinary tract infection, and skin infection occurring with an estimated prevalence of .01%<ref name="12" /><ref name="22" />. Symptoms of fever (>100 degrees), chills, malaise, and fatigue may be present concurrent with a patient’s LBP. These infections in the spine are also commonly found in patients with a current or past medical history of immunosuppresion. Waldvogel, F. et al.<ref name="43">Waldvogel FA. et al. Osteomyelitis: the past decade. N Engl J Med. 1980. 303:360-70</ref><br>reported on the diagnostic utility of the subjective examination in this patient population, of note is the lack of screening utility of the presence of fever in this population. See Table. One exception is for infective spondylitis with a positive response for fever offering a sensitivity of .98 and specificity of .50. | ||
'''TABLE - Waldvogel FA. et al. Osteomyelitis: the past decade. N Engl J Med. 1980. 303:360-70''' | '''TABLE - Waldvogel FA. et al. Osteomyelitis: the past decade. N Engl J Med. 1980. 303:360-70''' | ||
| Line 351: | Line 351: | ||
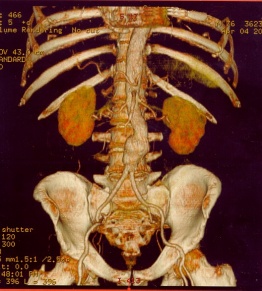
== [[Image:AneurysmAorta.jpg|left|262x291px|CT AAA]]<br>'''Abdominal Aortic Aneurysm'''<br> == | == [[Image:AneurysmAorta.jpg|left|262x291px|CT AAA]]<br>'''Abdominal Aortic Aneurysm'''<br> == | ||
Abdominal aortic aneurysms (AAA) are included within the visceral prevalence estimates for LBP. This disorder is responsible for 9000/deaths per year with men having 5-6 times the risk of females<ref>Lederle FA, et al. Selective screening for abdominal aortic aneurysms with physical examination and ultrasound. Arch Intern Med. 1988;148:1753-1756.</ref><ref>Lederle, F. et al. The aneurysm detection and management study screening program: validation cohort and final results. Aneurysm Detection and Management Veterans Affairs Cooperative Study Investigators. Arch Intern Med. 2000 May 22;160(10):1425-30.</ref>. Interestingly, 75% of patients are asymptomatic at the time of diagnosis <ref | Abdominal aortic aneurysms (AAA) are included within the visceral prevalence estimates for LBP. This disorder is responsible for 9000/deaths per year with men having 5-6 times the risk of females<ref name="29">Lederle FA, et al. Selective screening for abdominal aortic aneurysms with physical examination and ultrasound. Arch Intern Med. 1988;148:1753-1756.</ref><ref name="30">Lederle, F. et al. The aneurysm detection and management study screening program: validation cohort and final results. Aneurysm Detection and Management Veterans Affairs Cooperative Study Investigators. Arch Intern Med. 2000 May 22;160(10):1425-30.</ref>. Interestingly, 75% of patients are asymptomatic at the time of diagnosis <ref name="29" /><ref name="30" />. The generation of LBP in this pathology is thought to occur from the blood vessels or the pressure of the AAA on the vertebral bodies in the lumbar spine. This pain is typically present in the midline of the spine, hip, buttock, or abdomen described as throbbing or pulsing. Patients may have concurrent symptoms including early satiety, nausea, and weight changes. Lederle et al. reported risk factors include smoking (Odds Ratio (OR) 3-5), family history of AAA or vascular disease (OR 1.28-1.84), and an OR of 1.71 for each 7 year increase in age over 65 years old<ref name="29" /><ref name="30" />. | ||
'''<span id="1321968856066S" style="display: none"> </span>''' | '''<span id="1321968856066S" style="display: none"> </span>''' | ||
== '''Low Back Pain Classification System''' == | == '''Low Back Pain Classification System''' == | ||
After screening for risk factors, as well as, yellow and red flags the clinician may utilize the subjective history to assist in the classification of a patient with LBP to an indicated treatment group. The utilization of this classification system has demonstrated improvements in pain, disability, and a reduction in cost at 4 weeks and one year compared to Agency for Healthcare Policy and Research guidelines in patients with acute LBP<ref>Fritz, J. Delitto, A. et al. Comparison of Classification-Based Physical Therapy With Therapy Based on Clinical Practice Guidelines for Patients with Acute Low Back Pain. A Randomized Clinical Trial. Spine. 2003;1363-1372.</ref>. Further patients correctly treated within their appropriate sub group demonstrated reduced disability up to one year compared to those patients given treatments not consistent with their sub group classification<ref | After screening for risk factors, as well as, yellow and red flags the clinician may utilize the subjective history to assist in the classification of a patient with LBP to an indicated treatment group. The utilization of this classification system has demonstrated improvements in pain, disability, and a reduction in cost at 4 weeks and one year compared to Agency for Healthcare Policy and Research guidelines in patients with acute LBP<ref name="15">Fritz, J. Delitto, A. et al. Comparison of Classification-Based Physical Therapy With Therapy Based on Clinical Practice Guidelines for Patients with Acute Low Back Pain. A Randomized Clinical Trial. Spine. 2003;1363-1372.</ref>. Further patients correctly treated within their appropriate sub group demonstrated reduced disability up to one year compared to those patients given treatments not consistent with their sub group classification<ref name="6" />. The table below reports historical and subjective history items which can improve clinician’s ability to match patients to appropriate sub groups of treatment. | ||
{| style="width: 564px; height: 128px" cellspacing="1" cellpadding="1" width="564" border="1" | {| style="width: 564px; height: 128px" cellspacing="1" cellpadding="1" width="564" border="1" | ||
Revision as of 16:09, 22 November 2011
Original Editors - Brian Duffy, Carleen Jogodka, Jeff Ryg, James White
Lead Editor - Jeff Ryg
Evidence for the subjective exam. What evidence do we have the strength of the history in our examination? What information can we glean from it? How important is it in providing effective treatment?
Introduction [edit | edit source]
Low back pain (LBP) is a common, disabling condition with both musculoskeletal and non musculoskeletal contributions. It has been reported that greater than 80% of individuals will experience LBP within their lifetime and 20-30% of individuals are affected with these symptoms at any point in timeCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Katz et al. reported the cumulative cost to manage this condition is greater than 100 billion dollars per yearCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Given the high economic costs associated with LBP it is imperative for the clinician to obtain the necessary information needed to determine the appropriate plan of care, either outside referral or Physical Therapy treatment, for their patient. Matching appropriate interventions based on a patient’s symptoms has been shown to decrease healthcare costs in patients with LBPCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
The patient interview is the first opportunity for the clinician to gather information regarding the patient’s condition. Information gathered during the subjective history can increase the clinician’s confidence in either ruling in or ruling out a suspected condition through the utilization of likelihood ratios (LR) to determine the probability of a condition’s presence or absence. After determining the condition responsible for a patient’s LBP symptoms, the subjective examination may help determine which referral or intervention is warranted.
Subjective Examination[edit | edit source]
A thorough and detailed subjective history and review of systems allows the clinician to gather information regarding the location, quality, severity, irritability, and behavior of a patient’s symptoms. This information is then assimilated to identify patients appropriate for Physical Therapy and those who require a referral to an outside healthcare provider. The subjective examination facilitates this decision by providing a strong diagnostic resource given the patient’s presenting symptoms. Hampton, et al. reported the subjective history alone assisted in the medical diagnosis of 83% of patients seen in a primary care practiceCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Specifically, 4 subjective examination questions have demonstrated a sensitivity of 1.0 in screening for cancer in patients with LBPCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Despite its importance authors have reported the average time given to a patient to explain their symptoms without interruption is 18 seconds and once interrupted patients often do not return to their previous complaintsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. In contrast, an uninterrupted patient only needs 150 seconds to fully express their concernsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Based on the information gathered from the subjective examination, the clinician will determine which tests to perform designed to confirm or refute their hypothesis on the source of a patient’s symptoms. A selection of the most appropriate questions, with the highest diagnostic utility, will increase the clinician’s confidence in ruling in or out sinister disorders. The following paragraphs will describe questions demonstrating the strongest shifts in probability of a condition being present (+ LR) or absent (-LR). These shifts in probability provide an excellent resource to the clinician treating patients with LBP.
Risk Factors [edit | edit source]
The symptoms reported by patients collected through the intake paperwork, review of systems, and subjective examination can assist in clinical hypothesis generation and identification of risk factors shown to influence the prognosis of a patient with LBP. A recent review of the evidence and epidemiological data reports risk factors for LBP include advancing age with first onset between 30-40, sedentary lifestyle, history of back surgery, occupational demands, smoking, depression, corticosteroid use, and obesityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Many of these variables have been correlated with an increased risk of developing LBP in population based studies. Further, studies have identified features that are associated with chronicity of symptoms, such as lower extremity radiating pain, low expectations for recovery, elevated initial pain score, coping style, fear, and psychosocial stressCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Yellow Flags[edit | edit source]
Due to the multiple factors associated with pain and their relationship with behavior and personal beliefs, it is necessary to review additional details related to this interaction. Kendall defined yellow flags as factors which increase the risk of developing, or perpetuating long term disability and work loss associated with low back painCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title including depression, pain catastrophizing, and elevated fear avoidance beliefs. Arroll et al. reported two questions, “During the past month have you been feeling down, depressed or hopeless?” and “During the past month have you been bothered by having little interest or pleasure in doing things?”, although lacking diagnostic properties (Specificity (Sp) .57-.67), improve our ability to screen (Sensitivity (Sn) .96-.97) for the presence of depression in patients with LBPCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. In addition, asking patients when they would like assistance with these questions can help identify those patients benefiting from help today ((+) Likelihood ratio (LR) 17.5) or help in the future ((+) LR 7.9) for their depression.
Elevated fear avoidance scores associated with the fear avoidance beliefs questionnaire (FABQ) have been associated with an exaggerated perception of pain and an elevated risk for chronic LBP symptomsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Specifically, a FABQ Work score >34 and work score <29 produces a (+) LR 3.33 and (-) LR 0.08, respectively, for the development of chronic LBP symptoms. Calley et al. reported the utilization of a two question screen for fear avoidance behaviors including “Are you afraid physical activity will cause an increase in your LBP?” and “Are you afraid that moving your back will be harmful to you?” can be effective for identifying patients requiring further education on their LBP symptomsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. An education session devoted to improving a patient’s understanding of pain neurophysiology including nociception and central sensitization, as well as, understanding their thoughts and beliefs regarding their symptoms can improve outcomes in these patientsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Clinician’s should aim to reduce a patient’s focus on the patho-anatomical sources of their LBP (ex. herniated disc), educate the patient on the resiliency of the spine and limitations of imaging in LBP, and improve a patient’s self efficacy for management of their symptoms.
Red Flags[edit | edit source]
Although uncommon, non musculoskeletal conditions may present as LBP in approximately 5% of patients presenting to primary care offices (see table)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Within this 5%, 1% are attributed to non mechanical disorders including cancer, infection, and inflammatory arthropathies; 1-2% are attributed to the viscera (abdominal aortic aneurysm (AAA), pelvic, renal, GI); and 2-3% are attributed to other diseases (Paget’s disease, parathyroid disease).
- Estimated 5% of LBP is caused by serious disease
- 1% Non mechanical spine disorders (cancer, infection, seronegative spondyloarthritides)
- 1-2% Visceral disease (Pelvic, renal, aortic aneurysm, GI)
- 2-3% Other Disease (Paget's disease, parathyroid disease, hemoglobinopathies)
Cauda Equina Syndrome[edit | edit source]
Cauda Equina Syndrome (CES) commonly involves a large midline lumbar disc herniation at L4/5, L5/S1, or less commonly L3/4 which impairs lumbosacral nerve functionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. This disorder is most frequently seen in individuals aged 40-60 with a prevalence estimated at .04% of the populationCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Up to 70% of patients with this disorder will complain of a chronic history of LBP and may report symptoms including incontinence, loss of sphincter tone, saddle anesthesia, gait disturbances, unilateral or bilateral sciatica, and urinary retention depending on the severity and duration of symptoms. Early identification of CES is important considering surgical decompression is most successful in patients < 72 hours since onsetCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Each of these reported symptoms provide the clinician with additional information necessary to rule in or out this condition. Specifically, saddle anesthesia (Sn .75) and unilateral or bilateral sciatica (Sn. 80) may assist in the screening of this patientCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. More importantly, the presence (Sp .95, +LR 9.9) or absence (Sn. 90, –LR .11) of urinary retention offers the greatest diagnostic utility for CES Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Cancer[edit | edit source]
The prevalence of cancer within the LBP population is estimated at 0.7%Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title and although this condition is rare clinicians can increase their confidence in screening for this pathology by following the evidence supported in the literature. Henschke, N. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title conducted a systematic review on 6 studies of 5,097 patients and found a prevalence ranging from .1 to 3.5%. A previous history of cancer (+LR 23) and clinician judgment consistent with cancer (+ 12.1) offered the best shift in post test probability of cancer being present. Conversely, a patient younger than 50 years of age demonstrated a (-) LR of .34 for the presence of cancer. See Table. Further, Deyo, R. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title demonstrated a four item cluster of age >50 years old, unexplained weight changes, a previous history of cancer, and no improvement with conservative care offered the best screening utility for cancer in patients with LBP (Sn 1.0, -LR .06 (0.0-.91)). In short, if a patient answers no to these historical items we can have increased confidence in our ability to rule out cancer as the source of a patient’s LBP symptoms.
TABLE - Henschke, N. et al. Screening for malignancy in low back pain patients:
a systematic review. Eur Spine J. 2007. 16:1673–1679.
| Clinical Response | Post Test Probability given 1% pre test probability | Post test probability given 5% pre test probability |
| No relief with bed rest | 1.7 | 8.3 |
| Age > 50 years | 2.2 | 10.4 |
| Duration > 1 month | 2.5 | 12.1 |
| No improvement at 1 month | 2.9 | 13.7 |
| Previous history of cancer | 19.2 | 55.7 |
Ankylosing Spondylitis
[edit | edit source]
Ankylosing Spondylitis (AS) is an inflammatory arthropathy most commonly occurring in males in their 20s and 30s with an estimated prevalence of 3%Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Radiographic evidence of ankylosis may not be present until several years following initial onset of back pain or stiffnessCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Given these findings a thorough history and subjective examination may help in early detection of AS. A past medical history significant for irritable bowel syndrome, crohn’s disease, psoriatic arthritis, and reactive arthritis are often found in patients with ASCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Inflammatory back pain (IBP) is a common sign associated with AS. Diagnostic variables of IBP include age < 40 years, > 3 month onset of symptoms, insidious onset, morning stiffness lasting at least 30 min, and improvement with exercise. These variables demonstrated a sensitivity of .95 and specificity of .85 if 4 of the 5 criteria were metCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Specifically, patients with AS may complain of pain and stiffness longer than 3 months, morning stiffness lasting at least 30 minutes, no improvement of back pain with rest, awakening in the second half of the night because of back pain, and alternating buttock pain. If 3 of these 4 criteria are met then there is a (+) LR of 12.4 of AS being presentCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. See Table 1. In addition, Gran, J. et al.17 reported 5 questions with diagnostic value: age < 40 years old, morning stiffness, improvement of symptoms with exercise, a gradual onset, and duration of symptoms > 3 months, offer small shifts in the probability of this condition being present. See Table 2.
TABLE 1 – Rudaweit, M. et al. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum. 2006. 54;569-578.
| Sn | Sp | (+) LR | (-) LR | |
| 2/4 Positive | .70 | .81 | 3.7 | |
| 3/4 Positive | .33 | .98 | 12.4 |
TABLE 2 - Gran JY. et al. An epidemiological survey of the signs and symptoms of ankylosing spondylitis. Clin Rheum. 1985;4:161-9.
| Sn | Sp | (+) LR | (-)LR | |
| Positive 4/5 Questions | .23 | .82 | 1.3 | .94 |
| > 40 years old | 1.0 | .07 | 1.1 | 0.0 |
| No relief in supine | .80 | .07 | 1.6 | .41 |
| Morning stiffness | .64 | .59 | 1.6 | .41 |
| > 3 months of pain | .09 | .99 | 9.0 | .92 |
Lumbar Stenosis[edit | edit source]
Lumbar spine stenosis (LSS) is estimated to represent 3% of patients with LBP and is most commonly found in older adultsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Compression of neurologic structures within the spine can occur from soft tissue (disc, ligament) or bone structures. Up to 20% of asymptomatic individuals over 60 years old may demonstrate pathology on imaging. Symptoms of back pain and leg pain associated with lumbar stenosis must be differentiated from vascular claudication within this population. A patient reporting a minimal duration of rest required for symptoms to ease following activity may indicate a vascular versus neurological claudication. In a previous study, Katz, J. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title reported on the diagnostic utility of historical items within the subjective examination (see table) with age >65 years old and severe leg pain offering the best screening utility for lumbar stenosis while the best diagnostic properties were found with relief of symptoms with sitting.
TABLE - Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-41.
| Sn | Sp | (+) LR | (-) LR | |
| > 65 years old | .77 | .69 | 2.5 | .33 |
| Severe LE pain | .65 | .67 | 2.0 | .52 |
| No pain with sitting | .46 | .93 | 6.6 | .58 |
| Worse with walking | .71 | .30 | 1.0 | .97 |
| Pain better with sitting | .52 | .83 | 3.1 | .58 |
| Numbness | .63 | .59 | 1.5 | .63 |
| Weakness | .47 | .78 | 2.1 | .68 |
Lumbar Disc Herniations
[edit | edit source]
A herniated lumbar disc is estimated to have a prevalence of 4% in the LBP population occurring most frequently in patients aged 30-55 years oldCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. 95% of these herniations occur at the L4/5 and L5/S1 levels involving the L5 and S1 nerve roots, respectively. Commonly patients will report an acute onset of pain radiating below the knee. Vroomen, P. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title and Lauder, T. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title reported on the diagnostic utility of historical examination items in patients with suspected lumbosacral nerve root symptoms. See Tables 1 and 2. The absence of sciatica, lower extremity pain not greater than back pain, and an absence of dermatomal pain offered the greatest value for screening for this pathology.
TABLE 1 - Vroomen, P. et al. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry 2002;72:630–634
| Sn | Sp | (+) LR | (-) LR | |
| Sciatica | .95 | |||
| Leg pain > back pain | .82 | .54 | 1.74 | .33 |
| Dermatomal pain | .89 | .31 | 1.3 | .34 |
TABLE 2 - Lauder, T. et al. Effect of history and exam in predicting electrodiagnostic outcome among patients with suspected lumbosacral radiculopathy. Am J Phys Med. 2000. 79:60-68.
| (+) LR | (-) LR | |
| Weakness | 1.2 | .73 |
| Numbness | 1.0 | 9.4 |
Vertebral Frature
[edit | edit source]
Spinal fractures are most common in older, white females occurring with a prevalence of 4% with less than 1% occurring secondary to traumaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. This prevalence may be underestimated secondary to the asymptomatic nature of many osteoporotic fractures.
The clinician’s ability to improve the probability of this pathology being present is supported by the literature from Henschke, N. et al. who reported moderate to high shifts in probability if a patient’s pain is associated with major trauma or pain and tenderness within the spine. See table. Further evidenceCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title suggests a positive history of corticosteroid use may suggest the presence of vertebral fracture (Sp .95, (+) LR 12.0).
TABLE - Henschke, N. et al. A systematic review identifies five red flags to screen for vertebral fracture. J Clin Epidemiology. 2008. 61:110-118.
| Sn | Sp | (+) LR | (-) LR | |
| History of major trauma | .65 | .95 | 12.8 |
.37 |
| Pain and tenderness | .60 | .91 | 6.7 | .44 |
| Age < 50 years | .79 | .64 | 2.2 | .34 |
| Female | .47 | .80 | 2.3 | .67 |
| Corticosteroid use | .06 | .995 | 12.0 | .94 |
Spinal Infection
[edit | edit source]
Infections in the spine including osteomyelitis, septic discitis, abscess, and shingles most commonly present secondary to a previous infection elsewhere in the body. Infections known to cause spinal infection include IV drug use, skin infection, urinary tract infection, and skin infection occurring with an estimated prevalence of .01%Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Symptoms of fever (>100 degrees), chills, malaise, and fatigue may be present concurrent with a patient’s LBP. These infections in the spine are also commonly found in patients with a current or past medical history of immunosuppresion. Waldvogel, F. et al.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
reported on the diagnostic utility of the subjective examination in this patient population, of note is the lack of screening utility of the presence of fever in this population. See Table. One exception is for infective spondylitis with a positive response for fever offering a sensitivity of .98 and specificity of .50.
TABLE - Waldvogel FA. et al. Osteomyelitis: the past decade. N Engl J Med. 1980. 303:360-70
| Sn | Sp | (+) LR | (-) LR | |
| Concurrent infection or drug use | .40 | |||
| Spinal tenderness to percussion | .86 | .60 | 2.1 | .23 |
| Fever | .27-.83 |
Abdominal Aortic Aneurysm
[edit | edit source]
Abdominal aortic aneurysms (AAA) are included within the visceral prevalence estimates for LBP. This disorder is responsible for 9000/deaths per year with men having 5-6 times the risk of femalesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Interestingly, 75% of patients are asymptomatic at the time of diagnosis Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. The generation of LBP in this pathology is thought to occur from the blood vessels or the pressure of the AAA on the vertebral bodies in the lumbar spine. This pain is typically present in the midline of the spine, hip, buttock, or abdomen described as throbbing or pulsing. Patients may have concurrent symptoms including early satiety, nausea, and weight changes. Lederle et al. reported risk factors include smoking (Odds Ratio (OR) 3-5), family history of AAA or vascular disease (OR 1.28-1.84), and an OR of 1.71 for each 7 year increase in age over 65 years oldCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Low Back Pain Classification System[edit | edit source]
After screening for risk factors, as well as, yellow and red flags the clinician may utilize the subjective history to assist in the classification of a patient with LBP to an indicated treatment group. The utilization of this classification system has demonstrated improvements in pain, disability, and a reduction in cost at 4 weeks and one year compared to Agency for Healthcare Policy and Research guidelines in patients with acute LBPCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Further patients correctly treated within their appropriate sub group demonstrated reduced disability up to one year compared to those patients given treatments not consistent with their sub group classificationCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. The table below reports historical and subjective history items which can improve clinician’s ability to match patients to appropriate sub groups of treatment.
| LBP Classification Sub Group | Subjective Report |
| Manipulation | Acute onset, symptoms above knee, FABQ work subscale <16 |
| Direction Specific Exercise | Strong subjective preference for sitting, walking or standing, report of peripheralization with positioning |
| Stabilization Training | Younger age, previous history of LBP episodes |
| Traction | Symptoms of nerve root compression, lack of centralization with positioning |
Conclusion
[edit | edit source]
The subjective examination is one of most powerful tools a clinician can utilize in the examination and treatment of patients with LBP. The questions utilized during this process can improve the clinician’s confidence in identification of sinister pathology warranting outside referral, screening for yellow flags which may interfere with PT interventions, and assist in matching PT interventions with a patient’s symptoms.