Spondylolysis in Young Athletes: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
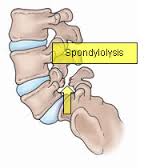
<span style="line-height: 1.5em;">[[Image:Spondylolysis.jpg|center|Figure showing a pars interarticularis defect present in Spondylolysis]]</span> | <span style="line-height: 1.5em;">[[Image:Spondylolysis.jpg|center|Figure showing a pars interarticularis defect present in Spondylolysis]]</span> | ||
<br> | == <span style="line-height: 1.5em;" />Spondylolisthesis == | ||
Spondylolisthesis is the forward shift of one vertebra on another. The slip usually occurs anteriorly at the levels of L5/S1 and causes the vertebra to move out of alignment with the other spinal vertebrae. This often occurs as a result of a bilateral spondylolysis (Luqmani et al., 2008), with it being reported that 50-81% of these cases developing a spondylolisthesis. However this may also occur as a result of birth defect, trauma or degeneration (Syrmou et al., 2010; Krabak, 2014). | |||
<br>The degree of slip can be graded using the Meyerding scale. A first degree injury involves slippage of 0-25% of the diameter. A second degree slip is 25-50% and a third degree is 50-75%. This can progress to a fourth degree slippage which would be a 75-100% diameter displacement or the vertebrae can displace by more than 100% producing a grade 5 slip (Krabak, 2014).<br> | |||
= Epidemiology/Etiology | = Epidemiology/Etiology = | ||
It is estimated that spondylolysis is present in 6 – 8% of the general population (Leone). The incidence has seen to be increased (47%) within the young athletic population (micheli). There is a particular increased risk in sports which subject athletes to repetitive hyperextension and rotation across the lumbar spine (iwanoto). Gymnasts, in particular, have been found to be 4 times more likely than their non athletic peers to develop a spondylolysis (Jackson). Research has also found there to be an increased risk for cricket bowlers, particularly fast bowlers (hardcastle). | It is estimated that spondylolysis is present in 6 – 8% of the general population (Leone). The incidence has seen to be increased (47%) within the young athletic population (micheli). There is a particular increased risk in sports which subject athletes to repetitive hyperextension and rotation across the lumbar spine (iwanoto). Gymnasts, in particular, have been found to be 4 times more likely than their non athletic peers to develop a spondylolysis (Jackson). Research has also found there to be an increased risk for cricket bowlers, particularly fast bowlers (hardcastle). | ||
| Line 23: | Line 27: | ||
= Clinical Presentation<br> = | = Clinical Presentation<br> = | ||
Majority of the cases are asymptomatic | Majority of the cases are asymptomatic | ||
( | <br>Subjective Assessment:<br>• Can be acute or gradual onset of pain<br>• May report recent history of trauma to that area<br>• Athletes between 15 and 16 most commonly diagnosed<br>• Increased risk for young athletes (6% of population below 18 diagnosed, 8-14% elite adolescent athletes diagnosed (Standaert & Herring, 2007))<br>• May be worse after intensive repetitive athletic activity (hyperextension or rotation) eg. Cricket, gymnastics, weightlifting, track and field athletes, tennis and rowing (Standaert & Herring, 2007) | ||
<br>Symptomatic athletic patients may present with:<br>• Focal low back pain<br>• Dull ache but can become sharp on movement<br>• Pain may be distributed more laterally if injury is unilateral<br>• Pain can radiate into buttock or proximal lower limb<br>• Intense pain<br>• Limits ADLs<br>• Insidious onset after traumatic event<br>• Progressively worsens<br>• Typically worsen after a stressful event<br>• Hamstring tightness<br>• Symptoms often worse with exercise<br>• Rest eases symptoms | |||
<br> | (Syrmou et al., 2010; Leone et al., 2011; Litao et al., 2013; Sundell et al., 2008)<br> | ||
= Differential Diagnosis = | = Differential Diagnosis = | ||
| Line 99: | Line 99: | ||
[[Image:Progression of exercises.jpg|center|400x600px|Progressive exercises for spondylolysis]] | [[Image:Progression of exercises.jpg|center|400x600px|Progressive exercises for spondylolysis]] | ||
The use of specific core strengthening exercises with spondylolysis patients has been shown to significantly reduce pain and enhance functional ability when compared to other conservative treatments (O’Sullivan, 1997).<br> | The use of specific core strengthening exercises with spondylolysis patients has been shown to significantly reduce pain and enhance functional ability when compared to other conservative treatments (O’Sullivan, 1997).<br> | ||
== Surgical == | == Surgical == | ||
| Line 139: | Line 139: | ||
{| width="1000" border="1" cellpadding="1" cellspacing="1" | {| width="1000" border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
! scope="col" | Title | ! scope="col" | Title | ||
! scope="col" | Authors | ! scope="col" | Authors | ||
! scope="col" | Source and Year | ! scope="col" | Source and Year | ||
! scope="col" | Aim | ! scope="col" | Aim | ||
! scope="col" | Type of study and subjects | ! scope="col" | Type of study and subjects | ||
! scope="col" | Key Findings | ! scope="col" | Key Findings | ||
! scope="col" | Limitations | ! scope="col" | Limitations | ||
|- | |- | ||
| Direct repair of spondylolytic defects in young competitive athletes <br> | | Direct repair of spondylolytic defects in young competitive athletes <br> | ||
| <span style="font-size: 13.63636302948px;">Reitman and Esses</span> | | <span style="font-size: 13.63636302948px;">Reitman and Esses</span> | ||
| <span style="font-size: 13.63636302948px;">Spine Journal – 2002</span> | | <span style="font-size: 13.63636302948px;">Spine Journal – 2002</span> | ||
| <span style="font-size: 13.63636302948px;"> To review outcome, specifically return to sport, in a group of competitive athletes after direct pars repair for symptomatic spondylolysis</span> | | <span style="font-size: 13.63636302948px;"> To review outcome, specifically return to sport, in a group of competitive athletes after direct pars repair for symptomatic spondylolysis</span> | ||
| <span style="font-size: 13.63636302948px;"> Retrospective case series of a single surgeon// Series of four athletes who underwent direct pars repair over an 18-month period</span><span style="font-size: 13.63636302948px;">l</span><span style="font-size: 13.63636302948px;">ack of detail regarding the control group and the exercise and interventions that they received. Also looked at spondylolthesis patients as well when this page is just looking at spondylolysis. </span> | | <span style="font-size: 13.63636302948px;"> Retrospective case series of a single surgeon// Series of four athletes who underwent direct pars repair over an 18-month period</span><span style="font-size: 13.63636302948px;">l</span><span style="font-size: 13.63636302948px;">ack of detail regarding the control group and the exercise and interventions that they received. Also looked at spondylolthesis patients as well when this page is just looking at spondylolysis. </span> | ||
| <span style="font-size: 13.63636302948px;">All participants were able to return to their presymptomatic level of activity with no restriction. One had periodic low back pain that required nonsteroidal anti-inflammatory medicine as needed. The others were entirely asymptomatic.</span> | | <span style="font-size: 13.63636302948px;">All participants were able to return to their presymptomatic level of activity with no restriction. One had periodic low back pain that required nonsteroidal anti-inflammatory medicine as needed. The others were entirely asymptomatic.</span> | ||
| <span style="font-size: 13.63636302948px;">Small sample size (only 4 participants) with the same surgeon.</span> | | <span style="font-size: 13.63636302948px;">Small sample size (only 4 participants) with the same surgeon.</span> | ||
|- | |- | ||
| Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis.//<br>/ .// // .// .// L<br> | | Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis.//<br>/ .// // .// .// L<br> | ||
| <span style="font-size: 13.63636302948px;">O’Sullivan, Phyty, Tworney and Alision </span> | | <span style="font-size: 13.63636302948px;">O’Sullivan, Phyty, Tworney and Alision </span> | ||
| <span style="font-size: 13.63636302948px;">Spine Journal – 1997/</span> | | <span style="font-size: 13.63636302948px;">Spine Journal – 1997/</span> | ||
| <span style="font-size: 13.63636302948px;">To determine the efficacy of a specific exercise intervention in the treatment of patients with chronic low back pain and a radiologic diagnosis of spondylolysis or spondylolisthesis</span> | | <span style="font-size: 13.63636302948px;">To determine the efficacy of a specific exercise intervention in the treatment of patients with chronic low back pain and a radiologic diagnosis of spondylolysis or spondylolisthesis</span> | ||
| <span style="font-size: 13.63636302948px;">A randomized, controlled trial, test--retest design</span><span style="font-size: 13.63636302948px;">Forty-four patients with this condition. Either randomly assigned to one of 2 groups. The first group underwent a 10-week specific exercise treatment program involving the specific training of the deep abdominal muscles, with co-activation of the lumbar multifidus proximal to the pars defects. The activation of these muscles was incorporated into previously aggravating static postures and functional tasks. The control group underwent treatment as directed by their treating practitione</span> | | <span style="font-size: 13.63636302948px;">A randomized, controlled trial, test--retest design</span><span style="font-size: 13.63636302948px;">Forty-four patients with this condition. Either randomly assigned to one of 2 groups. The first group underwent a 10-week specific exercise treatment program involving the specific training of the deep abdominal muscles, with co-activation of the lumbar multifidus proximal to the pars defects. The activation of these muscles was incorporated into previously aggravating static postures and functional tasks. The control group underwent treatment as directed by their treating practitione</span> | ||
| <span style="font-size: 13.63636302948px;">The specific exercise group showed a statistically significant reduction in pain intensity and functional disability levels, which was maintained at a 30-month follow-up. The control group showed no significant change in these parameters after intervention or at follow-up </span> | | <span style="font-size: 13.63636302948px;">The specific exercise group showed a statistically significant reduction in pain intensity and functional disability levels, which was maintained at a 30-month follow-up. The control group showed no significant change in these parameters after intervention or at follow-up </span> | ||
|- | |- | ||
| Line 187: | Line 187: | ||
|} | |} | ||
<br> | |||
{| width="1000" border="1" cellpadding="1" cellspacing="1" | {| width="1000" border="1" cellpadding="1" cellspacing="1" | ||
Revision as of 16:54, 15 January 2015
Introduction[edit | edit source]
Further adding to the knowledge of the Spondylolsis physiopedia page, this Wiki page aims to provide readers with a background understanding of spondylolysis, why the young athletic population are more at risk and give an insight into the different management options which are available. We will discuss in detail the different treatment options using pre-existing evidence, with a main focus on the efficacy of each treatment option in returning the athlete to sport.
What is Spondylolysis?[edit | edit source]
Spondylolysis is defined as a bony defect within the pars interarticularis of the vertebral arch (Syrmou, 2010. It presents as a weakness or fracture at this point (syrmou, 2010). The vast majority of spondylolitic defects are seen at level L5 (85-95%) (Standaert, 2003), with level L4 being the second most likely to be affected. The higher levels of the lumbar spine are rarely affected (Standaert, 2003).
Spondylolisthesis[edit | edit source]
Spondylolisthesis is the forward shift of one vertebra on another. The slip usually occurs anteriorly at the levels of L5/S1 and causes the vertebra to move out of alignment with the other spinal vertebrae. This often occurs as a result of a bilateral spondylolysis (Luqmani et al., 2008), with it being reported that 50-81% of these cases developing a spondylolisthesis. However this may also occur as a result of birth defect, trauma or degeneration (Syrmou et al., 2010; Krabak, 2014).
The degree of slip can be graded using the Meyerding scale. A first degree injury involves slippage of 0-25% of the diameter. A second degree slip is 25-50% and a third degree is 50-75%. This can progress to a fourth degree slippage which would be a 75-100% diameter displacement or the vertebrae can displace by more than 100% producing a grade 5 slip (Krabak, 2014).
Epidemiology/Etiology[edit | edit source]
It is estimated that spondylolysis is present in 6 – 8% of the general population (Leone). The incidence has seen to be increased (47%) within the young athletic population (micheli). There is a particular increased risk in sports which subject athletes to repetitive hyperextension and rotation across the lumbar spine (iwanoto). Gymnasts, in particular, have been found to be 4 times more likely than their non athletic peers to develop a spondylolysis (Jackson). Research has also found there to be an increased risk for cricket bowlers, particularly fast bowlers (hardcastle).
The exact cause of spondylolysis currently remains unclear, with many factors thought to contribute to its development (McCleary, 2007). It has been described as hereditary, or acquired as a result of repetitive stress to the lumbar spine (Haun, 2005). In the young athlete the spine is still growing, giving rise to numerous ossification centres which leave points of weakness in the spine (McCleary, 2007). This leaves young athletes, in particular those exposed to repetitive hyperextension and rotation of the lumbar spine (Iwanoto), susceptible to injury and the development of spondylolysis.
Clinical Presentation
[edit | edit source]
Majority of the cases are asymptomatic
Subjective Assessment:
• Can be acute or gradual onset of pain
• May report recent history of trauma to that area
• Athletes between 15 and 16 most commonly diagnosed
• Increased risk for young athletes (6% of population below 18 diagnosed, 8-14% elite adolescent athletes diagnosed (Standaert & Herring, 2007))
• May be worse after intensive repetitive athletic activity (hyperextension or rotation) eg. Cricket, gymnastics, weightlifting, track and field athletes, tennis and rowing (Standaert & Herring, 2007)
Symptomatic athletic patients may present with:
• Focal low back pain
• Dull ache but can become sharp on movement
• Pain may be distributed more laterally if injury is unilateral
• Pain can radiate into buttock or proximal lower limb
• Intense pain
• Limits ADLs
• Insidious onset after traumatic event
• Progressively worsens
• Typically worsen after a stressful event
• Hamstring tightness
• Symptoms often worse with exercise
• Rest eases symptoms
(Syrmou et al., 2010; Leone et al., 2011; Litao et al., 2013; Sundell et al., 2008)
Differential Diagnosis[edit | edit source]
Diagnosis[edit | edit source]
Spondylolysis in Sport[edit | edit source]
It was reported that 47% of low back pain in young athletes is diagnosed as spondylolysis (Micheli & Wood, 1995; McCleary & Congeni, 2007). High incidence rates of spondylolysis have been reported in a number of sports including cricket, gymnastics, tennis and weightlifting. Therefore this section will briefly touch upon some of these sports and why these young athletes are more predisposed to this condition.
Cricket[edit | edit source]
A 2002 study (Gregory, Batt, Wallace) observed bowlers over 6 months; they found that 10% of spin bowlers and 12% of fast bowlers developed LBP over the season. The action of bowling in cricket involves rotation and side flexion of the spine at high speeds. During the delivery phase the bowler is performing these movements to the best of their ability in order to gain as much speed, spin and strength to the ball. As the front leg comes forward to deliver the ball, forces travelling through the leg and up into the lumbar spine can be 3-9 times that of our bodyweight. Adding to this that the bowler will have to bowl 6 balls every over for as many as 9-10 overs. It is not hard to see why this repetitive and powerful motion may lead to a spondylolysis.
Studies believe that young cricketers are more at risk due to longer and more intense training sessions, poor preparation and technique, longer spells of bowling and subsequently overuse
It is common for these athletes to report non-specific low back pain, which often feels like a dull ache but can become a sharper pain during their sporting activity.
Treatment for this population can be difficult as it often involves rest in the early stages, this can be as long as 8 months in some cases. However it is then important to address factors such as muscle imbalance, core stability, flexibility and pelvic control. Although they will be unable to bowl during this period of time they can continue to maintain cardiovascular fitness – such as swimming and cycling – as long as they are symptom free. Most importantly treatment must be sport specific especially in the later stages of rehab.
Example: When focusing on core stability the player is standing on leg balancing on a soft cushion or trampette while performing the bowling action. This is later progressed by attaching the ball to a theraband, which is tied to a fixed point behind the player.
(Some of the information above was taken from a 2006 article in the Sport Ex magazine).
Gymnastics[edit | edit source]
It was reported in a paper published in 2000 (Guillodo, Botton, Saraux et al) that the incidence rate in gymnasts was between 15-20%, this is much higher than the general population. Once again it is not hard to understand why this would be due to the high physical demands of the sport, the hours of daily training and repetitive forces (Kruse & Brooke, 2009).
One case study that focused on female gymnasts in 1979 (Jackson, Wiltse, Circincione) looked at 100 gymnasts and found that 11 had spondylolysis and 6 of these had progressed to a spondylolysthesis. The girls described the pain as chronic, dull aching and found it was particularly aggravated when hyperextended.
Weightlifting[edit | edit source]
This is another high intensity sport, which involves increased forces. The incidence rate has been reported to be between 30.7-44% (Kotani, Ichikawa, Wakabayashi et al, 1970; Stone, Fry, Ritchie et al 1994). Studies believe there is a clear relationship between this condition and the stress of lifting.
Stone et al (1994) described the actions involved in weightlifting and discussed the excessive impact forces seen during the catching phase of the bar. They also noted that these stress and shear forces are greatly increased through the joints when the athlete completes the jump onto one leg.
Treatment
[edit | edit source]
Enabling patients to return to sport is at the forefront of any treatment plan for an athlete following injury (Brukner, 2005). Each athlete must be considered individually in terms of his/her symptoms, functional limitations, their sport and level of participation, as well as any other characteristics which may influence their treatment (Standaert and Herring, 2007).
The optimal treatment for athletes with spondylolysis is still widely debated within the literature, with there being a current lack of controlled studies to have investigated the management (Syrmou, 2010). However it is generally accepted that the young athlete with spondylolysis should initially be managed conservatively (McNeely, 2003). Surgical management is generally only considered when all conservative methods have failed, with only an estimated 9-15% of all symptomatic cases undergoing surgery (Syrmou, 2010).
Conservative[edit | edit source]
Conservative treatment is generally the initial management plan for young athletes with spondylolysis. The most common form conservative management applied is physiotherapy and can consist of:
• Periods of rest/ activity modification
• Lumbosacral brace
• Core stability strengthening - Bails add about hamstrings
• Electrical modalities
Physiotherapy with these patients aims to restore range of motion, stabilise and strengthen the spine, and to reduce pain (Hall & Brody, 1999).
The use and effectiveness of lumbosacral braces is still debated within the literature. Use of a brace is supposed to allow the healing of the bony defect in the pars interarticularis, reducing the athlete’s pain and allowing a return to sport. However, Watkins (2010) states that it is yet to be demonstrated statistically to enhance the healing of a spondylolitic defect. Previous studies though have found the use of bracing to be effective in allowing the return to sport for an athlete (Iwamoto, 2004; Sys, 2001). Both thes studies though, did include a period of exercise therapy following the use of the brace, prior to a return to sport.
Common physical therapy used in the rehabilitation of spondylolysis in young athletes is concentrated strengthening of the core stability muscles; transverse abdominus, multifidus and quadrates lumborum. With the main focus in the rehabilitation of athletes being a return to sport, it is important that core stability strengthening is progressed into functional, specific exercises for each athlete following an initial period of retraining/activating the core muscles.
The use of specific core strengthening exercises with spondylolysis patients has been shown to significantly reduce pain and enhance functional ability when compared to other conservative treatments (O’Sullivan, 1997).
Surgical[edit | edit source]
The use of surgery for spondylolysis within the young athletic population is seen as a last resort option, after all the methods of conservative treatment fail (Syrmou, 2010). There are vast arrays of surgical techniques which can be performed, but most commonly either a screw or wire fixation are the preferred methods (Drazin, 2011).
As like the conservative treatment methods, surgical treatment of spondylolysis with the young athletic population has been shown to be very effective in returning athletes to their sport (Reitman, 2002; Debnath, 2003). In fact one study (Reitman, 2002) demonstrated a 100% success rate for surgery with every athlete included in the study returning to their sport following surgery. However, in comparison to the conservative approach, surgical treatment did require athletes to have an extended period away from their sport. One study (Debnath, 2003) showed an average lay off time of 7 months following surgical treatment.
Due the nature of surgery, athletes still require a period of rehabilitation postoperatively (Drazin, 2011). This post operative treatment will include many of the exercises used in the conservative approach, targeting the strengthening of core stability muscles (Drazin, 2011).
Patient Experience [edit | edit source]
Case Study from Clinical Practice [edit | edit source]
This account was taken from a physiotherapist working in an outpatients setting. The case study describes a past patient that she assessed and treated.
A 15 year old keen cricketer and golfer presented with acute right-sided low back pain which had come on suddenly after playing cricket at the weekend; at the time he was unable to run and in fact felt considerable pain walking. During the week before this he had been on a golfing holiday playing a round a day and on some days 2 rounds. He had experienced a dull pain three weeks before and it was always related to cricket. In fact, this young boy recalled some twinges of pain in the previous school term while playing in the nets. He was a fast bowler.
This boy was in good health with no previous episodes of back pain. He had recently had a growth spurt.
On examination there was significant right-sided muscle spasm on lumber movements. There was pain during flexion and right side flexion with an excessive amount of movement available. Right hip flexion was painful and a right straight leg raise resulted in low back pain. On palpation there was pain and resistance at L4/5 and L5/S1.
During the initial treatment manual therapy was used to settle the acute pain and spasm. The patient reported that this eased the pain until he then went and picked up cricket balls from off the floor. He was referred on for further investigations at this point.
An x-ray, including oblique views, showed evidence of a spondylolysthesis of L5/S1. Therefore An MRI was arranged. This clearly showed a bilateral pars interarticularis defect. However there was no forward displacement of L5.
The patient was then instructed to completely rest for the next four months, he was referred back for physiotherapy at this point. Now, on examination, his movements were pain-free. On palpation there was some mild stiffness in the low lumbar spine but the hip and straight leg raise showed no symptoms. Treatment at this point included gentle stability and strengthening exercises.
For example he was encouraged to stretch his hamstrings, use breathing control and begin lower transverse abdominal exercises: spine curls in lying, bridging exercises and stability exercises whilst moving the legs.
These were later progressed onto the Swiss Ball combined with more functional exercises in standing aiming towards cricket related exercises. For example using the overhead movement of the arm taking care not to over extend the lumbar spine. Ensuring there wasn't a hinge point into lumber extension and that rotation was used. It was also worth checking he had enough available shoulder movement.
Patient Testimonial [edit | edit source]
Kamal is a 21 year old, cricket player, playing at a competitive University level. He was diagnosed with Spondylolysis 5 years ago. and was treated conservatively with physiotherapy. In his testimony, made by ourselves, Kamal talks about his experiences, treatment, and emotional well being, as young athele with spondylolsis.
Review of Key Papers [edit | edit source]
| Title | Authors | Source and Year | Aim | Type of study and subjects | Key Findings | Limitations |
|---|---|---|---|---|---|---|
| Direct repair of spondylolytic defects in young competitive athletes |
Reitman and Esses | Spine Journal – 2002 | To review outcome, specifically return to sport, in a group of competitive athletes after direct pars repair for symptomatic spondylolysis | Retrospective case series of a single surgeon// Series of four athletes who underwent direct pars repair over an 18-month periodlack of detail regarding the control group and the exercise and interventions that they received. Also looked at spondylolthesis patients as well when this page is just looking at spondylolysis. | All participants were able to return to their presymptomatic level of activity with no restriction. One had periodic low back pain that required nonsteroidal anti-inflammatory medicine as needed. The others were entirely asymptomatic. | Small sample size (only 4 participants) with the same surgeon. |
| Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis.// / .// // .// .// L |
O’Sullivan, Phyty, Tworney and Alision | Spine Journal – 1997/ | To determine the efficacy of a specific exercise intervention in the treatment of patients with chronic low back pain and a radiologic diagnosis of spondylolysis or spondylolisthesis | A randomized, controlled trial, test--retest designForty-four patients with this condition. Either randomly assigned to one of 2 groups. The first group underwent a 10-week specific exercise treatment program involving the specific training of the deep abdominal muscles, with co-activation of the lumbar multifidus proximal to the pars defects. The activation of these muscles was incorporated into previously aggravating static postures and functional tasks. The control group underwent treatment as directed by their treating practitione | The specific exercise group showed a statistically significant reduction in pain intensity and functional disability levels, which was maintained at a 30-month follow-up. The control group showed no significant change in these parameters after intervention or at follow-up | |
| Title | Authors | Source and Year | Aim | Type of Study and Subjects | Key Findings | Limitations |
|---|---|---|---|---|---|---|
| Back pain in young athletes | Micheli, LJ. & Wood R | Archives of Pediatrics and Adolescent Medicine. 1995 | To determine any differences between the causes of LBP in young athletes and adult population. | Retrospective randomized case comparison study. 100 athletes 12-18yrs. 100 adults 21-77. LBP | 47% of adolescents had spondylolysis. • 5% of adults |
Older Study. • A retrospective observational |
| Spondylolysis in the female gymnast |
Jackson, DW. Wiltse, LL. Cirincione, RJ | Clinical Orthopedics and Related Research, 1976. | A roentgenogenic analysis of the lumbar spine in 100 female gymnasts. | Cohort Study. 100 female gymnasts aged from 6-24 years. Regional, national and international levels |
11 of the 100 had spondylolysis. |
No clear aim of objective was given. • A very old study. • No clear study design was mentioned. |
| Contralateral Spondylolysis and Fracture of the Lumbar Pedicle in an Elite Female Gymnast: A Case Report |
Guillodo, Y. Botton, E. Saraux, A. Le Goff, P | Spine. 2000 | To present a fracture of the right lumbar pedicle in a female gymnast | A case Report. Female gymnast (born in 1983) who trains 15 hours a week. From 1994 to 1997 she underwent clinical examination and lumbar radiographs. | Reports a 15-20% incidence of spondylolysis in gymnasts. • There are inconsistencies between radiographs and observations. • Spontaneous consolidation of this fracture occurred despite continuing with gymnastics. |
No reference used for the incidence rate. • Older Study. • A case report: therefore still has a very subjective point of view from the subject. • Not generalisable. |
| Studies of Spondylolysis found among weightlifters. |
Kotani, PT. Ichikawa, N. Wakabayashi, W | British Journal of Sports Medicine. 1971. | To determine if there is a relationship between spondylolysis and the motion of lifting a weight | Case report. 26 male weightlifters aged 18 to 24 years. | 8 cases of spondylolysis were found = 30.7%. • Found more commonly in those who had been taking part for 4yrs + |
Small sample size. • Done before 1972 and therefore still using ‘standing-press’ – involves greater hyperextension |
| Comparing Injuries in spin bowlers with fast bowlers in young cricketers. | Gregory, P. Batt, M. Wallace, W | Clinical Journal of Sports Medicine. 2002. | To compare the incidence and anatomical distribution of injuries in fast and spin bowlers. | prospective cohort study. 112 young male bowlers; aged 9 to 21.
42 spin bowlers and 70 fast. Telephone questionnaire every 6 weeks for 6 months. |
Incidence of injury in fast = 0.165/1000 balls bowled.
• 17.6% were LBP injuries. |
Injuries were self-reported and not examined. |