Serotonin Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 73: | Line 73: | ||
<br> | <br> | ||
Physician's will use either Hunter's Toxicity Criteria or Sternbach's Criteria to diagnose Serotonin Syndrome.<ref name="Wilson et al">Wilson L, Rooney T, Baugh RF, Millington B. Recognition and management of perioperative serotonin syndrome. AJO 2012; 33:319-321. http://ck8zf4yc8t.search.serialssolutions.com.libproxy.bellarmine.edu/?genre=article&amp;isbn=&amp;issn=1532818X&amp;title=American+Journal+Of+Otolaryngology&amp;volume=33&amp;issue=3&amp;date=20120501&amp;atitle=Recognition+and+management+of+perioperative+serotonin+syndrome.&amp;aulast=Wilson+L&amp;spage=319&amp;sid=EBSCO:MEDLINE&amp;pid= (accessed 8 March 2013).</ref><br> | Physician's will use either Hunter's Toxicity Criteria or Sternbach's Criteria to diagnose Serotonin Syndrome.<ref name="Wilson et al">Wilson L, Rooney T, Baugh RF, Millington B. Recognition and management of perioperative serotonin syndrome. AJO 2012; 33:319-321. http://ck8zf4yc8t.search.serialssolutions.com.libproxy.bellarmine.edu/?genre=article&amp;amp;isbn=&amp;amp;issn=1532818X&amp;amp;title=American+Journal+Of+Otolaryngology&amp;amp;volume=33&amp;amp;issue=3&amp;amp;date=20120501&amp;amp;atitle=Recognition+and+management+of+perioperative+serotonin+syndrome.&amp;amp;aulast=Wilson+L&amp;amp;spage=319&amp;amp;sid=EBSCO:MEDLINE&amp;amp;pid= (accessed 8 March 2013).</ref><br> | ||
{| width="800" border="1" cellpadding="1" cellspacing="1" | {| width="800" border="1" cellpadding="1" cellspacing="1" | ||
| Line 263: | Line 263: | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox"><rss> | <div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1J3Q0COHK8s_j5FFdD48tQDF6yLMwxs1iq6Ycsuon67WUNWoKk|charset=UTF-8|short|max=10</rss><br></div> | ||
<br> | <br> | ||
Revision as of 15:06, 10 March 2013
Original Editors -HannahAnderson & Millie Ware from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[1][2][3][edit | edit source]
Serotonin syndrome occurs when you take medications that cause high levels of the chemical serotonin to accumulate in your body. Serotonin syndrome can occur when you increase the dose of such a drug or add a new drug to your regimen. Certain illicit drugs and dietary supplements are also associated with serotonin syndrome.
Serotonin is a chemical your body produces that's needed for your nerve cells and brain to function. But too much serotonin causes symptoms that can range from mild — shivering and diarrhea — to severe — muscle rigidity, fever and seizures. Severe serotonin syndrome can be fatal if not treated.
Serotonin syndrome most often occurs when two drugs that affect the body's level of serotonin are taken together at the same time. The drugs cause too much serotonin to be released or to remain in the brain area.
Vomiting, sleep, temperature regulation, appetite, mood, regulation of blood pressure, and the perception of pain are functions that involve brain serotonergic neurons. Serotonin may also be associated or involved in conditions such as migraine headaches and anxiety. While correct serotonin concentrations can greatly improve quality of life, too much serotonin can have deleterious effects manifested as Serotonin Syndrome.
Prevalence[edit | edit source]
- Serotonin Syndrome is on the rise, however information on it is limited.
- According to an article in the New England Journal of Medicine, in 2002 there were over 7,000 cases of Serotonin Syndrome and of those 93 cases were fatal.[4]
- Approximately 10% of the adult population in the U.S. reports having Depression.[5]
- In 2011, the U.S. Center of Disease Control finished a study about the number of Americans taking Anti-depressants. The CDC found that one in every ten people over the age of 12 years old is taking an antidepressant.[6]
- According to the Migraine Research Foundation, every one of four homes in the U.S. has someone who experiences migraines.[7]
- The American Migraine Foundation states that 36 million Americans suffer from migraines.[8]
Characteristics/Clinical Presentation[2][edit | edit source]
Serotonin syndrome symptoms typically occur within several hours of taking a new drug or increasing the dose of a drug you're already taking. Signs and symptoms include:
- Agitation or restlessness
- Confusion
- Rapid heart rate and high blood pressure
- Dilated pupils
- Loss of muscle coordination or twitching muscles
- Heavy sweating
- Diarrhea
- Headache
- Shivering
- Goose bumps
Severe serotonin syndrome can be life-threatening. Signs and symptoms include:
- High fever
- Seizures
- Irregular heartbeat
- Unconsciousness
Associated Co-morbidities[9][edit | edit source]
- Depression
- Migraine Headaches
- Cluster Headaches
Medications[1][edit | edit source]
- Benzodiazepines such as diazepam (Valium) or lorazepam (Ativan): to decrease agitation, seizure-like movements, and muscle stiffness
- Cyproheptadine (Periactin): a drug that blocks serotonin production
Diagnostic Tests/Lab Tests/Lab Values[2][1][edit | edit source]
Typically to diagnose Serotonin Syndrome, physicians will do various diagnostic tests to rule out other diseases and causes of the patient’s signs and symptoms. Tests may include:
- Blood cultures
- Complete blood count
- Drug screen
- Electrolyte levels
- Electrocardiogram
- Kidney and liver function tests
- Thyroid function tests
- Check body functions that may be affected by Serotonin Syndrome
Physician's will use either Hunter's Toxicity Criteria or Sternbach's Criteria to diagnose Serotonin Syndrome.[11]
| Classification | Hunter Toxicity Criteria | Sternbach Criteria |
| 1. Must have taken a serotenergic agent and have ONE of the following: | 1. Recent addition or increase in a known serotinergic agent | |
| A. Spontaneous clonus | 2. Absence of other possible etiologies | |
| B. Inducible clonus plus agitation or diaphoresis | 3. No recent addition or increase of a neuroleptic agent | |
| C. Ocular clonus plus agitation or diaphoresis | 4. At least 3 of the following symptoms: mental status changes, agitation, myoclonus, hyperreflexia, diaphoresis, shivering, tremor, diarrhea, incoordination, fever | |
| D. Tremor and hyperreflexia | ||
| E. Hypertonia | ||
| F. Temperature above 38° plus ocular or inducible clonus | ||
| Sensitivity | 84% |
75% |
| Specificity | 97% | 96% |
Etiology/Causes[2][edit | edit source]
Serotonin syndrome most often occurs when two drugs that affect the body's level of serotonin are taken together at the same time. The drugs cause too much serotonin to be released or to remain in the brain area.
Although it's possible that taking just one drug that increases serotonin levels can cause serotonin syndrome in susceptible individuals, it occurs most often when you combine certain medications. For example, serotonin syndrome may occur if you take an antidepressant with a migraine medication. A common cause of serotonin syndrome is intentional overdose of antidepressant medications.
A number of over-the-counter and prescription drugs may be associated with serotonin syndrome, especially antidepressants. Illicit drugs and dietary supplements also may be associated with the condition. These drugs and supplements include:
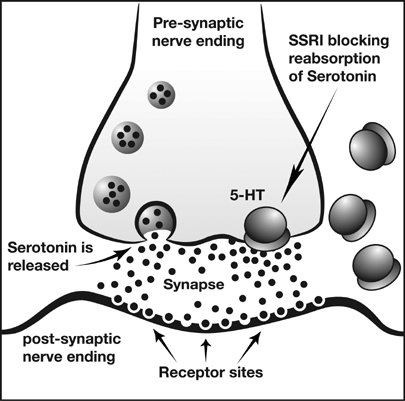
- Selective serotonin reuptake inhibitors (SSRIs), antidepressants such as citalopram (Celexa), fluoxetine (Prozac, Sarafem), fluvoxamine, paroxetine (Paxil) and sertraline (Zoloft)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs), antidepressants such as trazodone and venlafaxine (Effexor)
- Bupropion (Wellbutrin, Zyban), an antidepressant and tobacco-addiction medication
- Tricyclic antidepressants, such as amitriptyline and nortriptyline (Pamelor)
- Monoamine oxidase inhibitors (MAOIs), antidepressants such as isocarboxazid (Marplan) and phenelzine (Nardil)
- Anti-migraine medications such as triptans (Axert, Amerge, Imitrex), carbamazepine (Tegretol) and valproic acid (Depakene)
- Pain medications such as cyclobenzaprine (Flexeril), fentanyl (Duragesic), meperidine (Demerol) and tramadol (Ultram)
- Lithium (Lithobid), a mood stabilizer
- Illicit drugs, including LSD, Ecstasy, cocaine and amphetamines
- Herbal supplements, including St. John's wort and ginseng
- Over-the-counter cough and cold medications containing dextromethorphan (Delsym, Robitussin DM, others)
- Anti-nausea medications such as granisetron (Kytril), metoclopramide (Reglan) and ondansetron (Zofran)
- Linezolid (Zyvox), an antibiotic
- Ritonavir (Norvir), an anti-retroviral medication used to treat HIV/AIDS
Serotonin syndrome is more likely to occur when you first start or increase the medicine.
SSRI and Serotonin[12]
Systemic Involvement[13][1][edit | edit source]
Musculoskeletal System
o Clonus
o Muscle rigidity
o Hyperreflexia
Central Nervous System
o Altered mental status, delirium, agitation
o Akathisia (RLS)
Autonomic Nervous System
o Changes in blood pressure
o Tachycardia
o Increase in body Temperature
o Gastrointestinal System: diarrhea, nausea, vomiting
Medical Management (current best evidence)[1][2][edit | edit source]
Treatment:
Patients with serotonin syndrome should stay in the hospital for at least 24 hours for close observation.
Treatment may include:
- Benzodiazepines such as diazepam (Valium) or lorazepam (Ativan) to decrease agitation, seizure-like movements, and muscle stiffness
- Cyproheptadine (Periactin), a drug that blocks serotonin production
- Fluids by IV
- Withdrawal of medicines that caused the syndrome
- In life-threatening cases, medicines that keep your muscles still (paralyze them) and a temporary breathing tube and breathing machine will be needed to prevent further muscle damage.
Treatment of serotonin syndrome depends on the severity of your symptoms.
- If your symptoms are minor, a visit to the doctor and stopping the medication causing the problem may be enough.
- If you have symptoms that concern your doctor, you may need to go to the hospital. Your doctor may have you stay in the hospital for several hours to make sure you're OK.
- If you have severe serotonin syndrome, you'll need intensive treatment in a hospital.
Depending on your symptoms, you may receive the following treatments:
- Muscle relaxants. Benzodiazepines, such as diazepam (Valium) or lorazepam (Ativan), can help control agitation, seizures and muscle stiffness.
- Serotonin-production blocking agents. If other treatments aren't working, medications such as cyproheptadine can help by blocking serotonin production.
- Oxygen and intravenous (IV) fluids. Breathing oxygen through a mask helps maintain normal oxygen levels in your blood, and IV fluids are used to treat dehydration and fever.
- Drugs that control heart rate and blood pressure. These may include esmolol (Brevibloc) or nitroprusside (Nitropress), to reduce a high heart rate or high blood pressure. If your blood pressure is too low, your doctor may give you phenylephrine (Neo-Synephrine) or epinephrine.
- A breathing tube and machine and medication to paralyze your muscles. These may be necessary if you have a high fever.
Milder forms of serotonin syndrome usually go away within 24 hours of stopping medications that increase serotonin, and by taking medications to block the effects of serotonin already in your system if they're needed. However, symptoms of serotonin syndrome caused by some antidepressants could take several weeks to go away completely. These medications remain in your system longer than do other medications that can cause serotonin syndrome.
Physical Therapy Management (current best evidence)[14][edit | edit source]
Physical therapy can include:
- Inclusion of passive range of motion activities: Progression to active-assist, active, and with resistance range of motion activities
- Walking program: Treadmill training, over-ground training
- Strengthening: core and extremities
Alternative/Holistic Management (current best evidence)[edit | edit source]
Depression[15]
- Diet: Follow a diet primarily based on whole foods (ex. fruits, vegetables, whole grains, lean meats, and fish), avoid foods high in sugar (ex. soda, processed foods, sugary snacks)
- Exercise: According to research, exercise can cause an increase in serotonin levels similar to those caused by medication. In addition, exercise can be beneficial to mood and energy level.
- Talk Therapy: Cognitive-behavioral therapy and interpersonal therapy are strategies for patients to help manage their Depression.
Migraines/Headaches[16]
- Biofeedback: Can decrease the number and length of headaches
- Stress Management: getting enough sleep, relaxation/breathing techniques
- Acupuncture: May cause a release in endorphins in the body that help with decreasing pain
- Massage: To reduce stress
- Herbs: Feverfew
- Essential Oils: Aromatherapy
- Diet: Supplement diet with Omega-3 fatty acids, avoid foods high in fat
Differential Diagnosis[13][2][edit | edit source]
Serotonin Syndrome is unlikely to be the cause of the symptoms the patient is experiencing if they have not taken a Selective Serotonin Reuptake Inihibitor (SSRI), Serotonin-norepinephrine Reuptake Inihibitor (SNRI), or a Triptan within the last month.
Possible Diagnoses:
- Anticholinergic Overdose: This can be caused by use of insecticides. Symptoms include dry/hot skin, absent bowel sounds, and normal reflexes.
- Malignant Hyperthermia: This is related to the patient being under anesthesia and occurs acutely. Hyporeflexia is a common symptom.
- Neuroleptic Malignant Syndrome: NMS is a reaction to a dopamine antagonist drug. This is most commonly confused with Serotonin Syndrome because similar symptoms (ex. Hyperthermia, changes in mental status). However, symptoms of this syndrome that are different from Serotonin Syndrome are bradykinesia and muscle rigidity. Also, there is a gradual onset over a many days, whereas symptoms of Serotonin Syndrome quickly progress.
- Amphetamine, cocaine, or an MAOI drug overdose
- Some thyroid conditions
- Alcohol or heroin withdrawal
Case Reports/ Case Studies[edit | edit source]
Sener S, Yamanel L, Comert B. A fatal case of severe serotonin syndrome accompanied by moclobemide and paroxetine overdose. IJCCM 2005; 9:173-175. http://web.ebscohost.com.libproxy.bellarmine.edu/ehost/pdfviewer/pdfviewer?sid=ed470dbb-f94b-4f9f-a041-c3d02070ee0d%40sessionmgr112&vid=25&hid=117 (accessed 8 March 2013).
Wilson L, Rooney T, Baugh RF, Millington B. Recognition and management of perioperative serotonin syndrome. AJO 2012; 33:319-321. http://ck8zf4yc8t.search.serialssolutions.com.libproxy.bellarmine.edu/?genre=article&isbn=&issn=1532818X&title=American+Journal+Of+Otolaryngology&volume=33&issue=3&date=20120501&atitle=Recognition+and+management+of+perioperative+serotonin+syndrome.&aulast=Wilson+L&spage=319&sid=EBSCO:MEDLINE&pid= (accessed 8 March 2013).
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Mayo Clinic - Serotonin Syndrome:
www.mayoclinic.com/health/serotonin-syndrome/DS00860
Hope for Depression Research Foundation:
American Migraine Foundation:
www.americanmigrainefoundation.org/
Recent Related Research (from Pubmed) [edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NGmwZeh8JwVIzrKgHG1LrDm0izTr7ViJiDkSYAY2BW5hiXsx0|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 PubMed Health. Serotonin Syndrome. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004531/ (accessed 6 March 2013).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Mayo Clinic. Serotonin Syndrome. http://www.mayoclinic.com/health/serotonin-syndrome/DS00860 (accessed 6 March 2013). Cite error: Invalid
<ref>tag; name "Mayo Clinic" defined multiple times with different content Cite error: Invalid<ref>tag; name "Mayo Clinic" defined multiple times with different content Cite error: Invalid<ref>tag; name "Mayo Clinic" defined multiple times with different content Cite error: Invalid<ref>tag; name "Mayo Clinic" defined multiple times with different content Cite error: Invalid<ref>tag; name "Mayo Clinic" defined multiple times with different content - ↑ Utox Update. Serotonin Syndrome. http://uuhsc.utah.edu/poison/healthpros/utox/vol4_no4.pdf (accessed 6 March 2013).
- ↑ Boyer EW, Shannon M. Current concepts the serotonin syndrome. NEJM 2005; 352: 1112-1121. http://toxicology.ucsd.edu/art%203%20serotonin%20syndrome.pdf (accessed 8 March 2013).
- ↑ Centers for Disease Control and Prevention. CDC Features: An Estimated 1 in 10 U.S. Adults Report Depression. http://www.cdc.gov/features/dsdepression/ (accessed 8 March 2013).
- ↑ Centers for Disease Control and Prevention. NCHS Data Brief - Number 76, October 2011. http://www.cdc.gov/nchs/data/databriefs/db76.htm (accessed 8 March 2013).
- ↑ Migraine Research Foundation. About Migraine. http://www.migraineresearchfoundation.org/about-migraine.html (accessed 8 March 2011).
- ↑ American Migraine Foundation. About Migraine. http://www.americanmigrainefoundation.org/about-migraine/ (accessed 8 March 2011).
- ↑ National Headache Foundation. Press Kits – Facts About Triptans. http://www.headaches.org/press/NHF_Press_Kits/Press_Kits_-_Facts_About_Triptans (accessed 8 March 2013).
- ↑ ITV News. Depression News. http://www.itv.com/news/topic/depression/ (accessd 8 March 2013).
- ↑ Wilson L, Rooney T, Baugh RF, Millington B. Recognition and management of perioperative serotonin syndrome. AJO 2012; 33:319-321. http://ck8zf4yc8t.search.serialssolutions.com.libproxy.bellarmine.edu/?genre=article&amp;isbn=&amp;issn=1532818X&amp;title=American+Journal+Of+Otolaryngology&amp;volume=33&amp;issue=3&amp;date=20120501&amp;atitle=Recognition+and+management+of+perioperative+serotonin+syndrome.&amp;aulast=Wilson+L&amp;spage=319&amp;sid=EBSCO:MEDLINE&amp;pid= (accessed 8 March 2013).
- ↑ Neurotic Physiology. Back to Basics 3: Depression post 5, The Serotonin Theory of Depression. http://scientopia.org/blogs/scicurious/2010/08/25/back-to-basics-3-depression-post-5-the-serotonin-theory-of-depression/ (accessed 8 March 2013).
- ↑ 13.0 13.1 Robinson DS. Serotonin Syndrome. PPJ 2006; 13:36-38. http://www.primarypsychiatry.com/aspx/articledetail.aspx?articleid=554 (accessed 8 March 2013).
- ↑ Physical Therapy. Misdiagnosis of serotonin syndrome as fibromyalgia and the role of physical therapists. PTJ 2008; 88:757-765. http://ptjournal.apta.org/content/88/6/757.full#ref-1 (accessed 8 March 2013).
- ↑ WebMD. A Holistic Approach to Treating Depression. http://www.webmd.com/depression/features/holistic-medicine (accessed 8 March 2013).
- ↑ WebMD. Alternative Treatments for Migraines and Headaches. http://www.webmd.com/balance/nontraditional-headache-treatments (accessed 8 March 2013).