Secondary Progressive Multiple Sclerosis (SPMS) - A Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
== '''Abstract''' == | == '''Abstract''' == | ||
''' | '''Purpose:''' The purpose of this fictional case study is to present and examine the presentation of a patient with Secondary Progressive Multiple Sclerosis (SPMS) and present the research on the effects of treatment by an interdisciplinary health care team with the focus on physiotherapy management. This case spans from initial assessment to follow up and discharge. | ||
''' | '''Case Presentation:''' This fictional case study focuses on Geraldine Smith, a 35-year-old woman whose diagnosis recently changed from SPMS active without progression to SPMS active with progression. This progression brought an increase in symptoms mainly effecting her mobility, work, activities of daily living and participation in fun events with her family. | ||
'''Intervention:''' Mrs. Smith is prescribed an intervention program focusing on balance, strengthening, stretching and gait to help improve or limit her symptoms. Geraldine is currently seeking other treatment from her neurologist, occupational therapist and psychiatrist, while also looking into massage therapy and pelvic floor physiotherapy. | |||
'''Outcomes:''' Geraldine’s follow-up showed notable improvements in her fatigue level, balance and gait. Changing her gait aid improved her confidence, balance and gait overall. Her additional treatments from the rest of her interdisciplinary health care team have also contributed to her improved quality of life and functional ability. Geraldine’s success with her home exercise program and her improvements indicate that she is on track to meet her goals and can be discharged at this time. | |||
== '''Introduction''' == | == '''Introduction''' == | ||
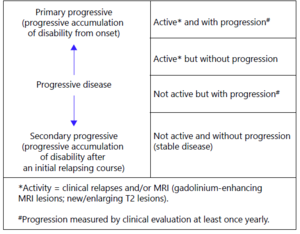
Multiple Sclerosis (MS) is an autoimmune inflammatory disease that causes the demyelination of neurons in the Central Nervous System (CNS). It tends to develop in young adults, resulting in considerable deficits in sensory, motor, autonomic, and neurocognitive function (Sospedra). MS can be classified as either Relapsing-Remitting MS (RRMS), or Progressive MS. The latter could be categorized as Primary or Secondary, and further broken down into active or not active, with or without progression, as listed in the diagram below. Progressive MS affects 10-20% of patients, and several mechanisms have been proposed to explain its occurrence. One explanation is that inflammation causes degeneration of the brain, while other theories state that the inflammation and neurodegeneration occur independently (Lassman). However, the two are not mutually exclusive. In fact, 50% of those diagnosed with RRMS will transition to Progressive MS within 10 years, and 90% will transition within 25 years (CITE PLS). Progression is measured through clinical evaluation of the patient’s status and outcome measures, at least once a year. This can be done using the Nine Hole Peg Test (NHPT), Timed 25-Foot Walk (T25FW), and Paced Auditory Serial Addition (PASAT) which give a picture of physical and cognitive function. | Multiple Sclerosis (MS) is an autoimmune inflammatory disease that causes the demyelination of neurons in the Central Nervous System (CNS). It tends to develop in young adults, resulting in considerable deficits in sensory, motor, autonomic, and neurocognitive function (Sospedra). MS can be classified as either Relapsing-Remitting MS (RRMS), or Progressive MS. | ||
[[File:MS Phenotypes.png|thumb|Figure 1. Classifications of Progressive MS. Referenced from...]] | |||
The latter could be categorized as Primary or Secondary, and further broken down into active or not active, with or without progression, as listed in the diagram below. Progressive MS affects 10-20% of patients, and several mechanisms have been proposed to explain its occurrence. One explanation is that inflammation causes degeneration of the brain, while other theories state that the inflammation and neurodegeneration occur independently (Lassman). However, the two are not mutually exclusive. In fact, 50% of those diagnosed with RRMS will transition to Progressive MS within 10 years, and 90% will transition within 25 years (CITE PLS). Progression is measured through clinical evaluation of the patient’s status and outcome measures, at least once a year. This can be done using the Nine Hole Peg Test (NHPT), Timed 25-Foot Walk (T25FW), and Paced Auditory Serial Addition (PASAT) which give a picture of physical and cognitive function. | |||
This case studies tracks the progress of Geraldine Smith, a 35-year-old woman diagnosed with Secondary Progressive Multiple Sclerosis (SPMS) in 2011. She initially reported symptoms of blurred vision, general weakness, and difficulty with balance to her family physician. The presence of low-level lesions and plaque formation in the cerebral white matter were noted through MRI imaging, and Evoked Potential testing was conducted to confirm the diagnosis as MS. The disease has been classified as active without progression for 10 years. Mrs. Smith was diagnosed with depression five years ago and hypertension 4 years ago. During her last visit to the neurologist, she noticed her symptoms were worsening. The MRI imaging confirmed her diagnosis had changed to SPMS active with progression. Her neurologist suggested she visit the Physical Therapy Clinic at Queen’s University to manage her symptoms and help her achieve some of her goals. She is easily fatigued during her job as a sales rep even when working from home, where she lives with her husband and daughter. | This case studies tracks the progress of Geraldine Smith, a 35-year-old woman diagnosed with Secondary Progressive Multiple Sclerosis (SPMS) in 2011. She initially reported symptoms of blurred vision, general weakness, and difficulty with balance to her family physician. The presence of low-level lesions and plaque formation in the cerebral white matter were noted through MRI imaging, and Evoked Potential testing was conducted to confirm the diagnosis as MS. The disease has been classified as active without progression for 10 years. Mrs. Smith was diagnosed with depression five years ago and hypertension 4 years ago. During her last visit to the neurologist, she noticed her symptoms were worsening. The MRI imaging confirmed her diagnosis had changed to SPMS active with progression. Her neurologist suggested she visit the Physical Therapy Clinic at Queen’s University to manage her symptoms and help her achieve some of her goals. She is easily fatigued during her job as a sales rep even when working from home, where she lives with her husband and daughter. | ||
| Line 13: | Line 19: | ||
Studies have researched the benefits of physical therapy management in patients with MS. Kalron et al. (2016) found that standardized physical therapy brings about a significant increase in gait speed and step length in patients at the end of an intervention program. A similar approach could be taken with Mrs. Smith to improve her mobility functions and assist her in reaching her personal goals. The incorporation of a balance rehabilitation program proves to reduce the fall rate and improve balance skills in subjects with MS, with a statistically significant difference on the Berg Balance Scale (Cattaneo, 2007). This form of physical therapy would tackle one of Mrs. Smith’s greatest concerns by reducing her risk of falls. | Studies have researched the benefits of physical therapy management in patients with MS. Kalron et al. (2016) found that standardized physical therapy brings about a significant increase in gait speed and step length in patients at the end of an intervention program. A similar approach could be taken with Mrs. Smith to improve her mobility functions and assist her in reaching her personal goals. The incorporation of a balance rehabilitation program proves to reduce the fall rate and improve balance skills in subjects with MS, with a statistically significant difference on the Berg Balance Scale (Cattaneo, 2007). This form of physical therapy would tackle one of Mrs. Smith’s greatest concerns by reducing her risk of falls. | ||
The purpose of this fictional case study is to present evidence-based research on the effects of physiotherapy management as part of an interprofessional healthcare team on a patient with SPMS. Comparisons are drawn from the patient’s case to existing literature to describe the history of illness, findings from the examination, interventions, and the resultant outcomes. | The purpose of this fictional case study is to present evidence-based research on the effects of physiotherapy management as part of an interprofessional healthcare team on a patient with SPMS. Comparisons are drawn from the patient’s case to existing literature to describe the history of illness, findings from the examination, interventions, and the resultant outcomes. | ||
== '''Client Characteristics''' == | == '''Client Characteristics''' == | ||
'''<br />''' | Geraldine Smith is a 35-year-old female (DOB: 12/31/1985) who was diagnosed with SPMS active without progression 10 years ago (2011) but her diagnosis has now developed to SPMS active with progression. Mrs. Smith currently lives with her husband and daughter in Kingston, Ontario and works from home as an online sales representative. Mrs. Smith was diagnosed with depression 5 years ago and hypertension 1 year later. Her neurologist recommended she attend physiotherapy due to her recent change in diagnosis to active with progression and her increasing difficulty with activities of daily living. Mrs. Smith is concerned about her current level of function with this recent decline and hopes that physiotherapy can help prevent further progression of her symptoms and improve her independent function. '''<br />''' | ||
== ''' '''Examination Findings == | == ''' '''Examination Findings == | ||
'''< | |||
=== '''Subjective Assessment''' === | |||
===== Chief Complaint ===== | |||
Mrs. Smith is concerned with her current level of fitness because she wants to be “fit enough” to walk around at her daughter’s grade 8 graduation in one year. | |||
===== History of Present Illness ===== | |||
''Medical Diagnosis:'' SPMS active with progression | |||
* Diagnosis confirmed by: | |||
** MRI to identify areas of lesion in CNS | |||
** Evoked Potentials (measures the speed of nerve impulse conduction), sensorimotor EP | |||
** Expanded Disability Status Scale (EDSS) = 6 | |||
** Established by neurologist | |||
''Treatment to date:'' no previous history of physiotherapy treatment | |||
''Current symptoms''''':''' increased weakness and fatigue in lower extremities, reduced endurance, difficulty with normal gait and impaired balance, difficulty controlling bladder | |||
===== Past Medical History ===== | |||
* Diagnosed with SPMS-Active without Progression in 2011 (10 years ago) | |||
* ''Comorbidities:'' | |||
** Diagnosed with depression 5 years ago | |||
*** Recently started seeing a psychiatrist | |||
**** Prescribed medications | |||
**** Her weekly visits involving cognitive behaviour therapy (CBT) which has been helping her depression symptoms | |||
*** Diagnosed with hypertension 4 years ago | |||
* REF: <nowiki>https://www.ajmc.com/view/comorbidities-management-and-lifestyle-modification-in-patients-with-multiple-sclerosis</nowiki> | |||
===== Medications ===== | |||
* Baclofen – 10mg 3/day to help muscle spasms | |||
* Dalfampridine – 10mg every 12hrs to help with gait | |||
* Amantadine – 100mg 3/day to help with fatigue | |||
* Fluoxetine – 30mg/day to help with depression symptoms | |||
* Captopril – 25mg every 12hrs to control hypertension | |||
===== Social History ===== | |||
* ''Home'': Lives in a bungalow with 4 steps to reach the front entrance to the home | |||
* ''Social Support:'' Lives with her husband Jerry and their 12-year-old daughter | |||
* ''Occupation'': online sales representative | |||
** Currently working from home | |||
** Noticing the need to take more frequent breaks due to fatigue and reduced focus | |||
* ''Hobbies'': | |||
** Baking with her daughter | |||
** Walking outside in the sunny weather with her husband | |||
===== Family History ===== | |||
No previous family members with MS. | |||
===== Functional History ===== | |||
* Previously able to walk with single-point cane for at least 30 minutes without experiencing pain or fatigue. | |||
* Previously able to walk up the 4 front steps with quad cane and no railing without any difficulties. | |||
* Gradually decreased driving after her initial diagnosis and has not driven in over 2 years. | |||
===== Current Functional Status ===== | |||
* Able to walk for 5 minutes with a single point cane before stopping for a break, due to fatigue in the lower extremities. | |||
* Reports difficulties when going from sitting to standing in chairs without arms. | |||
** Experiencing difficulty getting on and off the toilet | |||
** Waiting for an Occupational Therapist consult for how to adjust home environment | |||
* Currently having difficulty ascending the 4 front steps with quad cane and use of railing. | |||
* Difficulty walking on the uneven grass to get to her driveway because it feels like her legs will collapse and she will fall. | |||
* Increased dependency on her husband for errands and household chores. | |||
* Feels unsteady when standing and baking due to lack of focus and other arm movements. | |||
* Had 1 fall 2 weeks ago and has had multiple near-falls since. | |||
===== Patient Goals ===== | |||
* Limit further progression of symptoms as much as possible. | |||
* Build up endurance to be able to walk with daughter at Grade 8 graduation. | |||
* Improve balance to be able to stand to bake and be able to walk on uneven surfaces. | |||
* Be able to walk up front steps without having to take a break. | |||
=== '''Objective Assessment''' === | |||
{| class="wikitable" | |||
|+Bilateral LE ROM (noting UE were WNL) | |||
Just trying out what a table looks like | |||
!Joint | |||
!Movement | |||
!Range | |||
|- | |||
|Hip | |||
|Flexion | |||
|110 | |||
|- | |||
|Hip | |||
|Extension | |||
|2 | |||
|- | |||
|Hip | |||
|Abduction | |||
|35 | |||
|- | |||
|Hip | |||
|Adduction | |||
|30 | |||
|- | |||
|Hip | |||
|IR | |||
|30 | |||
|- | |||
|Hip | |||
|ER | |||
|40 | |||
|- | |||
|Knee | |||
|Flexion | |||
|125 | |||
|- | |||
|Knee | |||
|Extension | |||
| -5 (missing) | |||
|- | |||
|Ankle | |||
|Plantar flexion | |||
|50 | |||
|- | |||
|Ankle | |||
|Dorsiflexion | |||
|0 | |||
|- | |||
|Ankle | |||
|Inversion | |||
|30 | |||
|- | |||
|Ankle | |||
|Eversion | |||
|10 | |||
|} | |||
* Spasticity - Modified Ashworth scale | |||
** UE – WNL (0) | |||
** LE (both sides) | |||
*** Hip flexors – 1+ | |||
*** Hip extensors – 1 | |||
*** Hip Abductors – 0 | |||
*** Hip Adductors – 0 | |||
*** Knee flexors – 1+ | |||
*** Knee extensors – 1 | |||
*** Ankle Plantar flexors – 2 | |||
*** Ankle Dorsiflexors - 1 | |||
* Strength - MMT | |||
** LE (bilateral) | |||
*** Hip | |||
**** Flexors: 4/5 | |||
**** Extensors: 3+/5 | |||
**** Abductors: 4/5 | |||
**** Adductors: 4/5 | |||
**** IR: 4/5 | |||
**** ER: 4/5 | |||
*** Knee | |||
**** Flexors: 4/5 | |||
**** Extensors: 4-/5 | |||
*** Ankle | |||
**** PFs: 3+/5 | |||
**** DFs: 3+/5 | |||
**** Inverters: 4/5 | |||
**** Everters: 4-/5 | |||
* | |||
Neurological | |||
* Dermatomes - WNL | |||
* Myotomes - WNL | |||
* Reflexes | |||
** UMN | |||
*** Clonus - positive | |||
*** Babinski - positive | |||
** LMN | |||
*** Patellar Tendon (L3-L4) Increased– 3/4 | |||
*** Achilles tendon (S1-S2) Increased - 3/4 | |||
* Sensation testing - WNL | |||
Gait | |||
* REF <nowiki>https://academic.oup.com/ptj/article/96/11/1744/2870036</nowiki> | |||
* Decreased ankle dorsiflexion at initial contact, insufficient heel strike | |||
* Decreased hip extension in terminal stance | |||
* Loss of dorsiflexion/heel raise in terminal stance | |||
* Reduced push off in pre-swing to initial swing | |||
* Incomplete foot clearance in initial swing | |||
* Lack of full knee extension in terminal swing | |||
* Reduced gait speed, step and stride length | |||
** Gait speed 0.5m/s with single point cane | |||
* Difficulty performing dual-tasks | |||
* Reliant on single point cane gait aid | |||
Balance | |||
* Administered Berg Balance Scale: 32/56 | |||
* Activities-Specific Balance Scale (ABC) Self Report Outcome Measure = 40 | |||
Fatigue | |||
* Fatigue severity scale (FSS) - 52/63 | |||
* INSERT IMAGE | |||
Walking Ability | |||
* Disease Steps = 4 late cane | |||
* Patient Determined Disease Steps =5 late cane | |||
* Timed up and go (TUG) (with single point cane) - 17 seconds | |||
** Increased risk of falls | |||
** Requires gait aid | |||
* 12-item MS Walking Scale (MSWS-12) - self report | |||
** Score: 42/60 or 62.5% | |||
* INSERT IMAGE | |||
* Endurance | |||
* Six-Minute Walk Test (6MWT) - 140m | |||
* With single point cane | |||
* Borg Rating of Perceived Exertion (RPE) = 16 | |||
Quality of Life and Physical Function | |||
* Multiple Sclerosis Impact Scale (MSIS-29) | |||
** Physical – 57 -> 46.25 | |||
** Psychological – 28 -> 52.78 | |||
* INSERT IMAGE | |||
== ''' '''Clinical Impression == | == ''' '''Clinical Impression == | ||
Revision as of 15:58, 13 May 2021
Abstract[edit | edit source]
Purpose: The purpose of this fictional case study is to present and examine the presentation of a patient with Secondary Progressive Multiple Sclerosis (SPMS) and present the research on the effects of treatment by an interdisciplinary health care team with the focus on physiotherapy management. This case spans from initial assessment to follow up and discharge.
Case Presentation: This fictional case study focuses on Geraldine Smith, a 35-year-old woman whose diagnosis recently changed from SPMS active without progression to SPMS active with progression. This progression brought an increase in symptoms mainly effecting her mobility, work, activities of daily living and participation in fun events with her family.
Intervention: Mrs. Smith is prescribed an intervention program focusing on balance, strengthening, stretching and gait to help improve or limit her symptoms. Geraldine is currently seeking other treatment from her neurologist, occupational therapist and psychiatrist, while also looking into massage therapy and pelvic floor physiotherapy.
Outcomes: Geraldine’s follow-up showed notable improvements in her fatigue level, balance and gait. Changing her gait aid improved her confidence, balance and gait overall. Her additional treatments from the rest of her interdisciplinary health care team have also contributed to her improved quality of life and functional ability. Geraldine’s success with her home exercise program and her improvements indicate that she is on track to meet her goals and can be discharged at this time.
Introduction[edit | edit source]
Multiple Sclerosis (MS) is an autoimmune inflammatory disease that causes the demyelination of neurons in the Central Nervous System (CNS). It tends to develop in young adults, resulting in considerable deficits in sensory, motor, autonomic, and neurocognitive function (Sospedra). MS can be classified as either Relapsing-Remitting MS (RRMS), or Progressive MS.
The latter could be categorized as Primary or Secondary, and further broken down into active or not active, with or without progression, as listed in the diagram below. Progressive MS affects 10-20% of patients, and several mechanisms have been proposed to explain its occurrence. One explanation is that inflammation causes degeneration of the brain, while other theories state that the inflammation and neurodegeneration occur independently (Lassman). However, the two are not mutually exclusive. In fact, 50% of those diagnosed with RRMS will transition to Progressive MS within 10 years, and 90% will transition within 25 years (CITE PLS). Progression is measured through clinical evaluation of the patient’s status and outcome measures, at least once a year. This can be done using the Nine Hole Peg Test (NHPT), Timed 25-Foot Walk (T25FW), and Paced Auditory Serial Addition (PASAT) which give a picture of physical and cognitive function.
This case studies tracks the progress of Geraldine Smith, a 35-year-old woman diagnosed with Secondary Progressive Multiple Sclerosis (SPMS) in 2011. She initially reported symptoms of blurred vision, general weakness, and difficulty with balance to her family physician. The presence of low-level lesions and plaque formation in the cerebral white matter were noted through MRI imaging, and Evoked Potential testing was conducted to confirm the diagnosis as MS. The disease has been classified as active without progression for 10 years. Mrs. Smith was diagnosed with depression five years ago and hypertension 4 years ago. During her last visit to the neurologist, she noticed her symptoms were worsening. The MRI imaging confirmed her diagnosis had changed to SPMS active with progression. Her neurologist suggested she visit the Physical Therapy Clinic at Queen’s University to manage her symptoms and help her achieve some of her goals. She is easily fatigued during her job as a sales rep even when working from home, where she lives with her husband and daughter.
Studies have researched the benefits of physical therapy management in patients with MS. Kalron et al. (2016) found that standardized physical therapy brings about a significant increase in gait speed and step length in patients at the end of an intervention program. A similar approach could be taken with Mrs. Smith to improve her mobility functions and assist her in reaching her personal goals. The incorporation of a balance rehabilitation program proves to reduce the fall rate and improve balance skills in subjects with MS, with a statistically significant difference on the Berg Balance Scale (Cattaneo, 2007). This form of physical therapy would tackle one of Mrs. Smith’s greatest concerns by reducing her risk of falls.
The purpose of this fictional case study is to present evidence-based research on the effects of physiotherapy management as part of an interprofessional healthcare team on a patient with SPMS. Comparisons are drawn from the patient’s case to existing literature to describe the history of illness, findings from the examination, interventions, and the resultant outcomes.
Client Characteristics[edit | edit source]
Geraldine Smith is a 35-year-old female (DOB: 12/31/1985) who was diagnosed with SPMS active without progression 10 years ago (2011) but her diagnosis has now developed to SPMS active with progression. Mrs. Smith currently lives with her husband and daughter in Kingston, Ontario and works from home as an online sales representative. Mrs. Smith was diagnosed with depression 5 years ago and hypertension 1 year later. Her neurologist recommended she attend physiotherapy due to her recent change in diagnosis to active with progression and her increasing difficulty with activities of daily living. Mrs. Smith is concerned about her current level of function with this recent decline and hopes that physiotherapy can help prevent further progression of her symptoms and improve her independent function.
Examination Findings[edit | edit source]
Subjective Assessment[edit | edit source]
Chief Complaint[edit | edit source]
Mrs. Smith is concerned with her current level of fitness because she wants to be “fit enough” to walk around at her daughter’s grade 8 graduation in one year.
History of Present Illness[edit | edit source]
Medical Diagnosis: SPMS active with progression
- Diagnosis confirmed by:
- MRI to identify areas of lesion in CNS
- Evoked Potentials (measures the speed of nerve impulse conduction), sensorimotor EP
- Expanded Disability Status Scale (EDSS) = 6
- Established by neurologist
Treatment to date: no previous history of physiotherapy treatment
Current symptoms: increased weakness and fatigue in lower extremities, reduced endurance, difficulty with normal gait and impaired balance, difficulty controlling bladder
Past Medical History[edit | edit source]
- Diagnosed with SPMS-Active without Progression in 2011 (10 years ago)
- Comorbidities:
- Diagnosed with depression 5 years ago
- Recently started seeing a psychiatrist
- Prescribed medications
- Her weekly visits involving cognitive behaviour therapy (CBT) which has been helping her depression symptoms
- Diagnosed with hypertension 4 years ago
- Recently started seeing a psychiatrist
- Diagnosed with depression 5 years ago
- REF: https://www.ajmc.com/view/comorbidities-management-and-lifestyle-modification-in-patients-with-multiple-sclerosis
Medications[edit | edit source]
- Baclofen – 10mg 3/day to help muscle spasms
- Dalfampridine – 10mg every 12hrs to help with gait
- Amantadine – 100mg 3/day to help with fatigue
- Fluoxetine – 30mg/day to help with depression symptoms
- Captopril – 25mg every 12hrs to control hypertension
Social History[edit | edit source]
- Home: Lives in a bungalow with 4 steps to reach the front entrance to the home
- Social Support: Lives with her husband Jerry and their 12-year-old daughter
- Occupation: online sales representative
- Currently working from home
- Noticing the need to take more frequent breaks due to fatigue and reduced focus
- Hobbies:
- Baking with her daughter
- Walking outside in the sunny weather with her husband
Family History[edit | edit source]
No previous family members with MS.
Functional History[edit | edit source]
- Previously able to walk with single-point cane for at least 30 minutes without experiencing pain or fatigue.
- Previously able to walk up the 4 front steps with quad cane and no railing without any difficulties.
- Gradually decreased driving after her initial diagnosis and has not driven in over 2 years.
Current Functional Status[edit | edit source]
- Able to walk for 5 minutes with a single point cane before stopping for a break, due to fatigue in the lower extremities.
- Reports difficulties when going from sitting to standing in chairs without arms.
- Experiencing difficulty getting on and off the toilet
- Waiting for an Occupational Therapist consult for how to adjust home environment
- Currently having difficulty ascending the 4 front steps with quad cane and use of railing.
- Difficulty walking on the uneven grass to get to her driveway because it feels like her legs will collapse and she will fall.
- Increased dependency on her husband for errands and household chores.
- Feels unsteady when standing and baking due to lack of focus and other arm movements.
- Had 1 fall 2 weeks ago and has had multiple near-falls since.
Patient Goals[edit | edit source]
- Limit further progression of symptoms as much as possible.
- Build up endurance to be able to walk with daughter at Grade 8 graduation.
- Improve balance to be able to stand to bake and be able to walk on uneven surfaces.
- Be able to walk up front steps without having to take a break.
Objective Assessment[edit | edit source]
| Joint | Movement | Range |
|---|---|---|
| Hip | Flexion | 110 |
| Hip | Extension | 2 |
| Hip | Abduction | 35 |
| Hip | Adduction | 30 |
| Hip | IR | 30 |
| Hip | ER | 40 |
| Knee | Flexion | 125 |
| Knee | Extension | -5 (missing) |
| Ankle | Plantar flexion | 50 |
| Ankle | Dorsiflexion | 0 |
| Ankle | Inversion | 30 |
| Ankle | Eversion | 10 |
- Spasticity - Modified Ashworth scale
- UE – WNL (0)
- LE (both sides)
- Hip flexors – 1+
- Hip extensors – 1
- Hip Abductors – 0
- Hip Adductors – 0
- Knee flexors – 1+
- Knee extensors – 1
- Ankle Plantar flexors – 2
- Ankle Dorsiflexors - 1
- Strength - MMT
- LE (bilateral)
- Hip
- Flexors: 4/5
- Extensors: 3+/5
- Abductors: 4/5
- Adductors: 4/5
- IR: 4/5
- ER: 4/5
- Knee
- Flexors: 4/5
- Extensors: 4-/5
- Ankle
- PFs: 3+/5
- DFs: 3+/5
- Inverters: 4/5
- Everters: 4-/5
- Hip
- LE (bilateral)
Neurological
- Dermatomes - WNL
- Myotomes - WNL
- Reflexes
- UMN
- Clonus - positive
- Babinski - positive
- LMN
- Patellar Tendon (L3-L4) Increased– 3/4
- Achilles tendon (S1-S2) Increased - 3/4
- UMN
- Sensation testing - WNL
Gait
- REF https://academic.oup.com/ptj/article/96/11/1744/2870036
- Decreased ankle dorsiflexion at initial contact, insufficient heel strike
- Decreased hip extension in terminal stance
- Loss of dorsiflexion/heel raise in terminal stance
- Reduced push off in pre-swing to initial swing
- Incomplete foot clearance in initial swing
- Lack of full knee extension in terminal swing
- Reduced gait speed, step and stride length
- Gait speed 0.5m/s with single point cane
- Difficulty performing dual-tasks
- Reliant on single point cane gait aid
Balance
- Administered Berg Balance Scale: 32/56
- Activities-Specific Balance Scale (ABC) Self Report Outcome Measure = 40
Fatigue
- Fatigue severity scale (FSS) - 52/63
- INSERT IMAGE
Walking Ability
- Disease Steps = 4 late cane
- Patient Determined Disease Steps =5 late cane
- Timed up and go (TUG) (with single point cane) - 17 seconds
- Increased risk of falls
- Requires gait aid
- 12-item MS Walking Scale (MSWS-12) - self report
- Score: 42/60 or 62.5%
- INSERT IMAGE
- Endurance
- Six-Minute Walk Test (6MWT) - 140m
- With single point cane
- Borg Rating of Perceived Exertion (RPE) = 16
Quality of Life and Physical Function
- Multiple Sclerosis Impact Scale (MSIS-29)
- Physical – 57 -> 46.25
- Psychological – 28 -> 52.78
- INSERT IMAGE
Clinical Impression[edit | edit source]
Interventions[edit | edit source]
Outcome[edit | edit source]
Discussion[edit | edit source]
Self-study Questions[edit | edit source]
References[edit | edit source]
'''''