Sacral Insufficiency Fractures: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
= Definition/Description = | = Definition/Description = | ||
Sacral insufficiency fractures (SIFs) are a cause of low back pain.<ref name="Meeusen">Meeusen, R. Praktijkgids rug- en nekletsels. Deel 1. Dienst uitgaven Vrije Universiteit Brussel. 218 blz.</ref><sup> | Sacral insufficiency fractures (SIFs) are a cause of low back pain.<ref name="Meeusen">Meeusen, R. Praktijkgids rug- en nekletsels. Deel 1. Dienst uitgaven Vrije Universiteit Brussel. 218 blz.</ref><sup> </sup><br>These kind of fractures are a subtype of stress fractures. They result from normal stress applied to a bone with reduced elasticity.<ref name="Lyders">Lyders E.M., Whitlow C.T., Baker M.D., Morris P.P., Imaging and treatment of sacral insufficiency fractures (review), Am. J. Neuroradiology 31:201-10, February 2010.fckLR(Levels of evidence: C)</ref> <ref name="Wild">Wild A., Jaeger M., Haak H., Mehdian S.H., Sacral insufficiency fracture, an unsuspected cause of low-back pain in elderly women. Arch. Orthop. Trauma. Surg (2002) 122:58-60fckLR(Levels of evidence: C)</ref> | ||
(Levels of evidence: C)</ref> <ref name="Wild">Wild A., Jaeger M., Haak H., Mehdian S.H., Sacral insufficiency fracture, an unsuspected cause of low-back pain in elderly women. Arch. Orthop. Trauma. Surg (2002) 122:58- | |||
(Levels of evidence: C)</ref | |||
An underlying condition like [[Osteoporosis|osteoporosis]] or other metabolic bone diseases are often a cause of SIFs. This is why SIFs are more common with elder women.<ref name="Lyders" /> <ref name="Wild" / | An underlying condition like [[Osteoporosis|osteoporosis]] or other metabolic bone diseases are often a cause of SIFs. This is why SIFs are more common with elder women.<ref name="Lyders" /> <ref name="Wild" /><ref name="Yong">Yong-Lee J., Bong-Jin H., Kim J.T., Chung D.S., Sacral insufficiency fracture, most overlooked cause of lumbosacral pain. J. Kor. Neurosurg. Soc. September 2008, 44 (3): 166-169fckLR(Levels of evidence: C)</ref> <sup> </sup><br>Bone insufficiency fractures are described first by Lourie in 1982.<ref name="Wild" /><sup> </sup><ref name="Yong" /> <sup> </sup> | ||
(Levels of evidence: C)</ref> | |||
= Clinically Relevant Anatomy = | = Clinically Relevant Anatomy = | ||
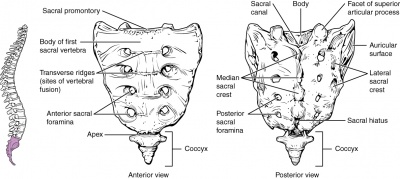
The sacrum is a triangular bone formed by 5 vertebral segments. It articulates superiorly with the fifth lumbar vertebra and inferiorly with the coccyx. The lateral surface of the upper part of the lateral masses (auricular surface) articulates with the ilium.<ref name="Tsiridis" /> | The sacrum is a triangular bone formed by 5 vertebral segments. It articulates superiorly with the fifth lumbar vertebra and inferiorly with the coccyx. The lateral surface of the upper part of the lateral masses (auricular surface) articulates with the ilium.<ref name="Tsiridis" /> | ||
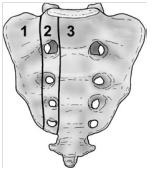
Denis et al classified traumatic sacral fractures by dividing the sacrum into 3 zones (Fig.1). These traumatic fractures are not directly related to SIFs, but the classification system of Denis is very useful for the description of the fractures.<ref name="Tsiridis">Tsiridis E., Upadhyay N., Giannoudis P.V., Sacral insufficiency fractures: current concepts of management. Osteoporos. Int. (2006) 17: 1716- | Denis et al classified traumatic sacral fractures by dividing the sacrum into 3 zones (Fig.1). These traumatic fractures are not directly related to SIFs, but the classification system of Denis is very useful for the description of the fractures.<ref name="Tsiridis">Tsiridis E., Upadhyay N., Giannoudis P.V., Sacral insufficiency fractures: current concepts of management. Osteoporos. Int. (2006) 17: 1716-1725fckLR(Levels of evidence: C)</ref> | ||
(Levels of evidence: C)</ref> | |||
Zone 1: involves the sacral ala (lateral to the sacral foramina). This is the most common site of SIFs.<br>Zone 2: involves the sacral (neural) foramina (but the fracture does not enter the central sacral canal). The fractures in this site are associated with unilateral lumbosacral radiculopathies.<br>Zone 3: involves the sacral bodies and the transverse central canal.<ref name="Lyders" /> <ref name="Tsidiris" /> <sup> | Zone 1: involves the sacral ala (lateral to the sacral foramina). This is the most common site of SIFs.<br>Zone 2: involves the sacral (neural) foramina (but the fracture does not enter the central sacral canal). The fractures in this site are associated with unilateral lumbosacral radiculopathies.<br>Zone 3: involves the sacral bodies and the transverse central canal.<ref name="Lyders" /> <ref name="Tsidiris" /> <sup><br></sup> | ||
<br> | <br> | ||
| Line 47: | Line 43: | ||
= Epidemiology /Etiology = | = Epidemiology /Etiology = | ||
The most important cause of SIF is [[Osteoporosis|osteoporosis.]]<ref name="Lyders" /> <ref name="Wild" /> <ref name="Dasgupta">Dasgupta B., Shah N., Brown H., Gordon T.E., Tanqueray A.B., Mellor J.A., Sacral insufficiency fractures: an unsuspected cause of low back pain. British Journal of Rheumatology 1998; 37: 789- | The most important cause of SIF is [[Osteoporosis|osteoporosis.]]<ref name="Lyders" /> <ref name="Wild" /> <ref name="Dasgupta">Dasgupta B., Shah N., Brown H., Gordon T.E., Tanqueray A.B., Mellor J.A., Sacral insufficiency fractures: an unsuspected cause of low back pain. British Journal of Rheumatology 1998; 37: 789-793fckLR(Levels of evidence: B)</ref> <ref name="Yong" /> Other risk factors are: | ||
(Levels of evidence: B)</ref> <ref name="Yong" /> | |||
*Pelvic radiation | *Pelvic radiation | ||
*Steroid-induced osteopenia <ref name="Yong" /> | *Steroid-induced osteopenia <ref name="Yong" /> | ||
*[[Rheumatoid Arthritis|Rheumatoid arthritis]] <ref name="Dasgupta" /> | *[[Rheumatoid Arthritis|Rheumatoid arthritis]] <ref name="Dasgupta" /> <br> | ||
*Multiple myeloma | *Multiple myeloma | ||
*[[Paget's Disease|Paget disease]] <ref name="Yong" /> | *[[Paget's Disease|Paget disease]] <ref name="Yong" /> | ||
*Renal osteodystrophy | *Renal osteodystrophy | ||
*Hyperparathyroidism <ref name="Lyders" /> <ref name="Karatas">KARATAS M., BASARAN C., OZGUL E., TARHAN E., AGILDERE A.M., Postpartum sacral stress fracture, An unusual case of low-back and buttock pain. Am. J. Phys. Med. Rehabil. Vol 87, No. 5. | *Hyperparathyroidism <ref name="Lyders" /> <ref name="Karatas">KARATAS M., BASARAN C., OZGUL E., TARHAN E., AGILDERE A.M., Postpartum sacral stress fracture, An unusual case of low-back and buttock pain. Am. J. Phys. Med. Rehabil. Vol 87, No. 5. 2008fckLR(Levels of evidence: C)</ref> <ref name="Wild" /> <ref name="Yong" /> | ||
(Levels of evidence: C)</ref> <ref name="Wild" /> <ref name="Yong" /> | *Corticosteroid medication <ref name="Lyders" /> <ref name="Wild" /> | ||
*Corticosteroid medication <ref name="Lyders" /> <ref name="Wild" /> | *Metastatic disease <ref name="Lyders" /> <ref name="Wild" /> | ||
*Metastatic disease <ref name="Lyders" /> <ref name="Wild" /> | *Marrow replacement processes <ref name="Lyders" /> <ref name="Wild" /> | ||
*Marrow replacement processes <ref name="Lyders" /> <ref name="Wild" /> | *Fibrous dysplasia <ref name="Karatas" /> | ||
*Fibrous dysplasia <ref name="Karatas" /> | *Osteogenesis imperfect<sup> <ref name="Karatas" /> </sup> | ||
*Osteogenesis imperfect<sup> <ref name="Karatas" /> | *Osteopetrosis <ref name="Karatas" /> | ||
*Osteopetrosis <ref name="Karatas" /> | *Osteomalacia <ref name="Karatas" /> | ||
*Osteomalacia <ref name="Karatas" /> | |||
Patients with SIFs are mostly time older than 55 years old. The mean age is between 70 and 75 years old.<br>The precise incidence of SIFs is unknown but some studies reported a prevalence of 1% - 5% in at-risk patient populations.<br>Two-third of patients were a-traumatic. <ref name="Lyders" /> | Patients with SIFs are mostly time older than 55 years old. The mean age is between 70 and 75 years old.<br>The precise incidence of SIFs is unknown but some studies reported a prevalence of 1% - 5% in at-risk patient populations.<br>Two-third of patients were a-traumatic. <ref name="Lyders" /> | ||
SFI can occur in a younger population. For example: pregnant women. This can be related to pregnancy-associated osteoporosis. <ref name="Karatas" /><sup>. | SFI can occur in a younger population. For example: pregnant women. This can be related to pregnancy-associated osteoporosis. <ref name="Karatas" /><sup>.</sup> | ||
= Characteristics/Clinical Presentation = | = Characteristics/Clinical Presentation = | ||
| Line 74: | Line 68: | ||
Patients with SIFs may have: | Patients with SIFs may have: | ||
*Tenderness of palpation (lower back and sacral region) <ref name="Lyders" /> <ref name="Kos">KOS C.B., TACONIS W.K., VAN DER EIJKEN J.W., Insufficiëntiefracturen van het sacrum, Ned. Tijdschr. Geneeskd 1999, 13 februari; 143(7) | *Tenderness of palpation (lower back and sacral region) <ref name="Lyders" /> <ref name="Kos">KOS C.B., TACONIS W.K., VAN DER EIJKEN J.W., Insufficiëntiefracturen van het sacrum, Ned. Tijdschr. Geneeskd 1999, 13 februari; 143(7)fckLR(Levels of evidence: C)</ref> <ref name="Wild" /> <ref name="Dasgupta" /> | ||
(Levels of evidence: C)</ref> <ref name="Wild" /> <ref name="Dasgupta" /> | *Pain (at the buttock, back, hip, pelvic or groin) <ref name="Thein">THEIN R., BURSTEIN G., SHABSHIN N., Labor-related sacral stress fracture presenting as lower limb radicular pain. Orthopedics June 2009; 32(6):447fckLR(Levels of evidence: B)</ref> | ||
*Pain (at the buttock, back, hip, pelvic or groin) <ref name="Thein">THEIN R., BURSTEIN G., SHABSHIN N., Labor-related sacral stress fracture presenting as lower limb radicular pain. Orthopedics June 2009; 32(6): | |||
(Levels of evidence: B)</ref> | |||
*Problems with walking (slowly and painfull) | *Problems with walking (slowly and painfull) | ||
*Nerve damage (unusual) <ref name="Lyders" /> <ref name="Wild" /> | *Nerve damage (unusual) <ref name="Lyders" /> <ref name="Wild" /> | ||
<br> | <br> | ||
| Line 87: | Line 79: | ||
Sacral insufficiency fractures are difficult to diagnose because the signs and symptoms are vague and non-specific. <br>SIFs can be confused with: | Sacral insufficiency fractures are difficult to diagnose because the signs and symptoms are vague and non-specific. <br>SIFs can be confused with: | ||
*Metastatic disease <ref name="Wild" /> | *Metastatic disease <ref name="Wild" /> | ||
*Radiculopathy <ref name="Lyders" /> | *Radiculopathy <ref name="Lyders" /> | ||
*Disc disease | *Disc disease | ||
*[[Spinal Stenosis|Spinal stenosis]] | *[[Spinal Stenosis|Spinal stenosis]] | ||
| Line 97: | Line 89: | ||
= Diagnostic Procedures = | = Diagnostic Procedures = | ||
SIF can be diagnosed with radiology. Bone scintigraphy is the most sensitive study to detect SIFs. Other radiographic procedures that can help to diagnose SIFs are magnetic resonance imaging (MRI) and computed tomography (CT) scans. <ref name="Lyders" /> <ref name="Wild" /> <ref name="Gotis-Graham">GOTIS-GRAHAM I., McGUIGAN L., DIAMOND T., PORTEK I., QUINN R., STURGESS A., TULLOCH R., Sacral insufficiency fractures in the elderly. J. Bone Joint Surg. 1994; 76-B: 882- | SIF can be diagnosed with radiology. Bone scintigraphy is the most sensitive study to detect SIFs. Other radiographic procedures that can help to diagnose SIFs are magnetic resonance imaging (MRI) and computed tomography (CT) scans. <ref name="Lyders" /> <ref name="Wild" /> <ref name="Gotis-Graham">GOTIS-GRAHAM I., McGUIGAN L., DIAMOND T., PORTEK I., QUINN R., STURGESS A., TULLOCH R., Sacral insufficiency fractures in the elderly. J. Bone Joint Surg. 1994; 76-B: 882-6fckLR(Levels of evidence: B)</ref> | ||
(Levels of evidence: B)</ref> | |||
<br> | <br> | ||
| Line 104: | Line 95: | ||
= Examination = | = Examination = | ||
The physical examination shows: <ref name="Tsiridis" /> | The physical examination shows: <ref name="Tsiridis" /> | ||
*Sacral tenderness (on lateral compression) | *Sacral tenderness (on lateral compression) | ||
| Line 116: | Line 107: | ||
= Physical Therapy Management = | = Physical Therapy Management = | ||
Early rehabilitation and moderate weight-bearing exercises, within the boundaries of pain tolerance, have been suggested. Earlier rehabilitation will stimulate the bone formation by the osteoblasts and improve muscle tension. <br>Mobilization is recommended because long periods of immobilization can result in complications (deep vein thrombosis, pulmonary embolus, loss of muscle strength, etc.). In the earlier stages of fracture healing, mobilization can be assisted by the use of external devices (e.g. walking frames) or hydrotherapy as these are typically tolerated better by many patients. <ref name="Tsiridis" /> | Early rehabilitation and moderate weight-bearing exercises, within the boundaries of pain tolerance, have been suggested. Earlier rehabilitation will stimulate the bone formation by the osteoblasts and improve muscle tension. <br>Mobilization is recommended because long periods of immobilization can result in complications (deep vein thrombosis, pulmonary embolus, loss of muscle strength, etc.). In the earlier stages of fracture healing, mobilization can be assisted by the use of external devices (e.g. walking frames) or hydrotherapy as these are typically tolerated better by many patients. <ref name="Tsiridis" /> | ||
<br> | <br> | ||
Revision as of 00:22, 20 April 2014
Search Strategy[edit | edit source]
Keywords:
- Sacral insufficiency fractures
- SIF
- Physical therapy OR Physiotherapy OR Exercise OR Treatment
- Mobilization
- Hydrotherapy OR Aquatherapy
Databases:
- Pubmed
- Web of Knowledge
- PEDro
- Google scholar
Definition/Description[edit | edit source]
Sacral insufficiency fractures (SIFs) are a cause of low back pain.[1]
These kind of fractures are a subtype of stress fractures. They result from normal stress applied to a bone with reduced elasticity.[2] [3]
An underlying condition like osteoporosis or other metabolic bone diseases are often a cause of SIFs. This is why SIFs are more common with elder women.[2] [3][4]
Bone insufficiency fractures are described first by Lourie in 1982.[3] [4]
Clinically Relevant Anatomy[edit | edit source]
The sacrum is a triangular bone formed by 5 vertebral segments. It articulates superiorly with the fifth lumbar vertebra and inferiorly with the coccyx. The lateral surface of the upper part of the lateral masses (auricular surface) articulates with the ilium.[5]
Denis et al classified traumatic sacral fractures by dividing the sacrum into 3 zones (Fig.1). These traumatic fractures are not directly related to SIFs, but the classification system of Denis is very useful for the description of the fractures.[5]
Zone 1: involves the sacral ala (lateral to the sacral foramina). This is the most common site of SIFs.
Zone 2: involves the sacral (neural) foramina (but the fracture does not enter the central sacral canal). The fractures in this site are associated with unilateral lumbosacral radiculopathies.
Zone 3: involves the sacral bodies and the transverse central canal.[2] [6]
Epidemiology /Etiology[edit | edit source]
The most important cause of SIF is osteoporosis.[2] [3] [7] [4] Other risk factors are:
- Pelvic radiation
- Steroid-induced osteopenia [4]
- Rheumatoid arthritis [7]
- Multiple myeloma
- Paget disease [4]
- Renal osteodystrophy
- Hyperparathyroidism [2] [8] [3] [4]
- Corticosteroid medication [2] [3]
- Metastatic disease [2] [3]
- Marrow replacement processes [2] [3]
- Fibrous dysplasia [8]
- Osteogenesis imperfect [8]
- Osteopetrosis [8]
- Osteomalacia [8]
Patients with SIFs are mostly time older than 55 years old. The mean age is between 70 and 75 years old.
The precise incidence of SIFs is unknown but some studies reported a prevalence of 1% - 5% in at-risk patient populations.
Two-third of patients were a-traumatic. [2]
SFI can occur in a younger population. For example: pregnant women. This can be related to pregnancy-associated osteoporosis. [8].
Characteristics/Clinical Presentation[edit | edit source]
Patients with SIFs may have:
- Tenderness of palpation (lower back and sacral region) [2] [9] [3] [7]
- Pain (at the buttock, back, hip, pelvic or groin) [10]
- Problems with walking (slowly and painfull)
- Nerve damage (unusual) [2] [3]
Differential Diagnosis[edit | edit source]
Sacral insufficiency fractures are difficult to diagnose because the signs and symptoms are vague and non-specific.
SIFs can be confused with:
- Metastatic disease [3]
- Radiculopathy [2]
- Disc disease
- Spinal stenosis
- Cauda equina syndrome
Diagnostic Procedures[edit | edit source]
SIF can be diagnosed with radiology. Bone scintigraphy is the most sensitive study to detect SIFs. Other radiographic procedures that can help to diagnose SIFs are magnetic resonance imaging (MRI) and computed tomography (CT) scans. [2] [3] [11]
Examination[edit | edit source]
The physical examination shows: [5]
- Sacral tenderness (on lateral compression)
- SI-joint tests are often positive (this test is not specific for SFI)
- Gait is slow and antalgic
- Trendelenburg test is normal
- Sciatic nerve tension tests (Lasegue and Straight Leg Raise (SLR)) are normal
Physical Therapy Management[edit | edit source]
Early rehabilitation and moderate weight-bearing exercises, within the boundaries of pain tolerance, have been suggested. Earlier rehabilitation will stimulate the bone formation by the osteoblasts and improve muscle tension.
Mobilization is recommended because long periods of immobilization can result in complications (deep vein thrombosis, pulmonary embolus, loss of muscle strength, etc.). In the earlier stages of fracture healing, mobilization can be assisted by the use of external devices (e.g. walking frames) or hydrotherapy as these are typically tolerated better by many patients. [5]
Resources[edit | edit source]
http://www.artrose-blog.nl/rugaandoeningen/insufficientiefracturen-van-het-sacrum
References[edit | edit source]
1. LYDERS E.M., WHITLOW C.T., BAKER M.D., MORRIS P.P., Imaging and treatment of sacral insufficiency fractures (review), Am. J. Neuroradiology 31:201-10, Februari 2010.
(Levels of evidence: C)
2. KOS C.B., TACONIS W.K., VAN DER EIJKEN J.W., Insufficiëntiefracturen van het sacrum, Ned. Tijdschr. Geneeskd 1999, 13 februari; 143(7)
(Levels of evidence: C)
3. THEIN R., BURSTEIN G., SHABSHIN N., Labor-related sacral stress fracture presenting as lower limb radicular pain. Orthopedics June 2009; 32(6):447
(Levels of evidence: B)
4. KARATAS M., BASARAN C., OZGUL E., TARHAN E., AGILDERE A.M., Postpartum sacral stress fracture, An unusual case of low-back and buttock pain. Am. J. Phys. Med. Rehabil. Vol 87, No. 5. 2008
(Levels of evidence: C)
5. WILD A., JAEGER M., HAAK H., MEHDIAN S.H., Sacral insufficiency fracture, an unsuspected cause of low-back pain in elderly women. Arch. Orthop. Trauma. Surg (2002) 122:58-60
(Levels of evidence: C)
6. DASGUPTA B., SHAH N., BROWN H., GORDON T.E., TANQUERAY A.B., MELLOR J.A., Sacral insufficiency fractures: an unsuspected cause of low back pain. British Journal of Rheumatology 1998; 37: 789-793
(Levels of evidence: B)
7. TSIRIDIS E., UPADHYAY N., GIANNOUDIS P.V., Sacral insufficiency fractures: current concepts of management. Osteoporos. Int. (2006) 17: 1716-1725
(Levels of evidence: C)
8. GOTIS-GRAHAM I., McGUIGAN L., DIAMOND T., PORTEK I., QUINN R., STURGESS A., TULLOCH R., Sacral insufficiency fractures in the elderly. J. Bone Joint Surg. 1994; 76-B: 882-6
(Levels of evidence: B)
9. YONG-LEE J., BONG-JIN H., KIM J.T., CHUNG D.S., Sacral insufficiency fracture, most overlooked cause of lumbosacral pain. J. Kor. Neurosurg. Soc. September 2008, 44 (3): 166-169
(Levels of evidence: C)
10. MEEUSEN, R. Praktijkgids rug- en nekletsels. Deel 1. Dienst uitgaven Vrije Universiteit Brussel. 218 blz.
- ↑ Meeusen, R. Praktijkgids rug- en nekletsels. Deel 1. Dienst uitgaven Vrije Universiteit Brussel. 218 blz.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Lyders E.M., Whitlow C.T., Baker M.D., Morris P.P., Imaging and treatment of sacral insufficiency fractures (review), Am. J. Neuroradiology 31:201-10, February 2010.fckLR(Levels of evidence: C)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Wild A., Jaeger M., Haak H., Mehdian S.H., Sacral insufficiency fracture, an unsuspected cause of low-back pain in elderly women. Arch. Orthop. Trauma. Surg (2002) 122:58-60fckLR(Levels of evidence: C)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Yong-Lee J., Bong-Jin H., Kim J.T., Chung D.S., Sacral insufficiency fracture, most overlooked cause of lumbosacral pain. J. Kor. Neurosurg. Soc. September 2008, 44 (3): 166-169fckLR(Levels of evidence: C)
- ↑ 5.0 5.1 5.2 5.3 Tsiridis E., Upadhyay N., Giannoudis P.V., Sacral insufficiency fractures: current concepts of management. Osteoporos. Int. (2006) 17: 1716-1725fckLR(Levels of evidence: C)
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedTsidiris - ↑ 7.0 7.1 7.2 Dasgupta B., Shah N., Brown H., Gordon T.E., Tanqueray A.B., Mellor J.A., Sacral insufficiency fractures: an unsuspected cause of low back pain. British Journal of Rheumatology 1998; 37: 789-793fckLR(Levels of evidence: B)
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 KARATAS M., BASARAN C., OZGUL E., TARHAN E., AGILDERE A.M., Postpartum sacral stress fracture, An unusual case of low-back and buttock pain. Am. J. Phys. Med. Rehabil. Vol 87, No. 5. 2008fckLR(Levels of evidence: C)
- ↑ KOS C.B., TACONIS W.K., VAN DER EIJKEN J.W., Insufficiëntiefracturen van het sacrum, Ned. Tijdschr. Geneeskd 1999, 13 februari; 143(7)fckLR(Levels of evidence: C)
- ↑ THEIN R., BURSTEIN G., SHABSHIN N., Labor-related sacral stress fracture presenting as lower limb radicular pain. Orthopedics June 2009; 32(6):447fckLR(Levels of evidence: B)
- ↑ GOTIS-GRAHAM I., McGUIGAN L., DIAMOND T., PORTEK I., QUINN R., STURGESS A., TULLOCH R., Sacral insufficiency fractures in the elderly. J. Bone Joint Surg. 1994; 76-B: 882-6fckLR(Levels of evidence: B)