Ruptured Spleen
Original Editors - Nick Hansen & Ren Peterson from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description [edit | edit source]
The spleen is an organ of the lymphatic system located on the left side of your stomach (abdomen) under the rib cage and diaphragm in a region that is referred to as the left upper quadrant. In humans the spleen is about the size of a fist and its primary roles are filtering the body’s blood and helps to fight infection. It also serves a role in storing and releasing certain types of immune cells that mediate tissue inflammation [1]
Rupturing a spleen describes an emergency situation in which your spleen has developed a break in its surface. This is serious condition that can occur during a direct blow or trauma and without emergency treatment a ruptured spleen can cause life threatening internal bleeding. [2]
Prevalence[edit | edit source]
The prevalence of splenic ruptures are poorly documented but one study suggest that traumatic splenic ruptures are more likely to occur in males (2:1 male to female) with ages ranging from 18-34 years.[3]
Infectious Mononucleosis – Annually in the United States there are appropriately 345 – 671 cases per 100,000. Typically involving school age children ages 13-19 years. Approximately 0.1% to 0.2% of the 345 – 671 cases in the United States will suffer from splenic ruptures. “Base on this figure, approximately 100 cases of ruptures may occur yearly in the US, only a few of which are reported.” [4]
Characteristics/Clinical Presentation[edit | edit source]
Signs and symptoms of a ruptured spleen includes: [2]
• Pain (usually severe but not always) in the upper left portion of the stomach (abdomen) or under rib cage
• Tenderness when you touch the upper left portion of the stomach (abdomen)
• Left shoulder pain-Kehr’s Sign
Kehr's sign (Hans Kehr (1862–1913), German surgeon] pain in the left shoulder caused by irritation of the undersurface of the diaphragm by blood leaking from a ruptured spleen. The pain impulses are referred along the phrenic nerve supplying the diaphragm C3-C5 nerve distribution. [5]
Internal bleeding due to a ruptured spleen can cause blood pressure to drop (hypotension). This can cause: [6]
• Blurred vision
• Confusion
• Light-headedness
• Fainting
• Signs of shock (cold clammy skin, pale, weak or rapid pulse)
It is strongly advised to seek immediate medical care if an injury is sustained coupled with pain in the left upper stomach (abdomen) region along with any of the above listed signs and symptoms. If severe injuries are untreated a ruptured spleen can be fatal.
Associated Co-morbidities[edit | edit source]
Common co-morbidities for traumatic splenic ruptures are hypertension, type II diabetes, and asthma. In a study involving 538 subjects, 25% suffered from one or more of the co-morbilities listed above. [7]
Non-traumatic splenic ruptures can be associated with numerous conditions and diseases. Some of the most common include, lymphoma, cirrhosis of the liver, liver disease, pancreatic pathology, bone marrow disorders such as leukaemia, and blood clotting disorders.
Viral diseases that can lead to splenic rupture include mononucleosis, malaria, and in rare cases HIV
Other conditions that can lead to splenic include drug addiction, sickle cell disease, and prolonged use of blood thinners.
Medications[edit | edit source]
No medications are prescribed to heal severe splenic ruptures, there are medications and vaccines recommended post-surgical removal of the spleen (splenectomy) in severe injuries.
The Advisory Committee on Immunization Practices for the Centers for Disease Control and Prevention (CDC) and the Society of Surgery for the Alimentary Tract recommends all patients that undergo splenectomy receive: [8]
• the pneumococcal polysaccharide vaccine
• meningococcal vaccination
• considered for the Hib vaccine
• annual influenza vaccine in addition to the pneumococcal, meningococcal, and Hib vaccines, because secondary bacterial infections can lead to severe disease in this patient population
• boosters for all the bacterial vaccines every 5 years
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Grades of Splenic Injury
| Grades | Extent of Splenic Injury |
| Grade 1 |
Hematoma; subscapular, non expanding, <10% of surface area Laceration: capsular tear, non bleeding, <1 cm of parenchymal depth |
| Grade 2 |
Hematoma, subscapular, non expanding, 10-50% of surace area, intraparenchyma, non expanding, <2 cm in diameter Laceration: capsular tear, active bleeding, 1-3 cm of parenchymal depth that does not involve a trabecular vessel |
| Grade 3 |
Hematoma: subscapular >50% of surface area or expanding, ruptured subscapuar hematoma with active bleeding, intraparenchymal hematoma, >2 cm or expanding Lacertation > 3 cm of parenchymal depth or involving trabecular vessels |
| Grade 4 |
Hematoma: ruptured intraparenchymal hematoma with active bleeding Laceration: laceration involving segmental or hilar vessel producing major devascularization (>25% of spleen) |
| Grade 5 |
Hematoma: completely ruptured spleen Laceration: hilar vascular injury that devacularizes spleen |
Table Reference[9]
The most common test used to diagnosis splenic rupture is computed tomography (CT) which can be supplemented by x-ray.
Spleen, trauma. Chest radiograph shows a peripherally calcified mass in the left upper quadrant under the diaphragm. The mass represents a calcified splenic hematoma.[10]
Spleen, trauma. Contrast-enhanced CT scan shows a localized area of dense contrast collection in the splenic hilum, with a massive amount of surrounding fluid/blood. Findings here are indicative of active extravasation of contrast in a patient with traumatic autosplenectomy. This is a grade V injury.[10]
Grade I - Subcapsular hematoma of less than 10% of surface area. Capsular tear of less than 1 cm in depth.[11]
Grade III - Subcapsular hematoma of greater than 50% of surface area or expanding and ruptured subcapsular or parenchymal hematoma. Intraparenchymal hematoma of greater than 5 cm or expanding. Laceration of greater than 3 cm in depth or involving trabecular vessels. [11]
Grade V - Shattered spleen or hilar vascular injury [11]
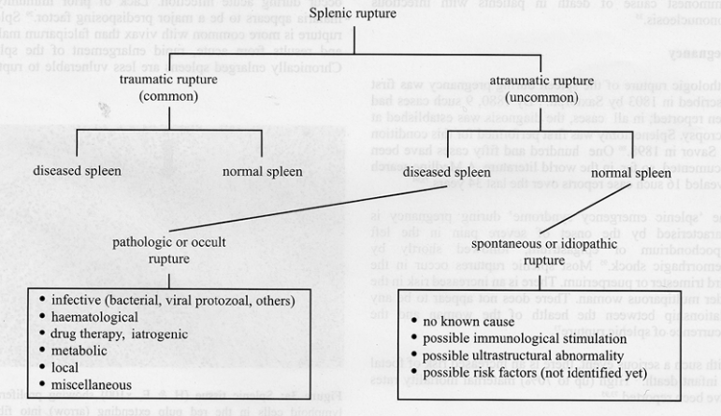
Etiology/Causes[edit | edit source]
Traumatic(common) [2]
• Injury or blow to left side of the body (left upper abdomen or left lower chest)
• Sports related
• Fights/Assaults
• Motor vehicle accidents
• Falls
Atraumatic(uncommon and diagnosis is often missed due to absence of any history of trauma)
http://www.rcsed.ac.uk/journal/vol47_1/47100010.html
http://www.rcsed.ac.uk/journal/vol47_1/47100010.html
Systemic Involvement[edit | edit source]
Rupture of the spleen can lead to life threatening bleeding into the abdominal cavity, which will lead to low blood pressure and decreased oxygen supply to the heart and brain. It is a medical emergency and should be referred to the emergency room immediately.
Medical Management (current best evidence)[edit | edit source]
First case control study on operative vs. non-operative management by Upadhyaya and Simpson in 1968 suggested that isolated splenic injuries could be safely treated without surgery in children. Pediatric surgeons led the way during the following decades, and non-operative management is now reported to be successful in more than 90 percent of children with isolated blunt injuries.[12]
Non-Operative Management (NOM)
• Non-operative management may require: [13]
• Significant blood transfusions
• Repeated CT scans
• Hematocrits (a centrifuge for separating blood cells from plasma)
• Close observation for up to 2 weeks, including an initial period of observation in intensive care.
• Non-Operative treatment is attempted in 60-90% of patients with blunt traumatic splenic injuries with intent to preserve splenic function [12]
• Spleen preserving surgery gained popularity in 1960’s due to the discovery of the spleens role in immune function [12]
• Predictors and other risk factors associated with failure of non-operative management: [12]
• Hemodynamic instability:
o systolic blood pressure less than 100 mm Hg
o heart rate greater than 120 beats per minute
o lack of response to a fluid challenge of 2 L of a crystalloid solution
•Contrast Extravasation:
o A leakage of contrast material into the fatty tissue around a vein. Contrast is a dye that allows your veins and arteries to show up more clearly on the CT/MRI scan [14]
• Arteriovenous Fistula:
o abnormal connection between an artery and a vein [2]
• Pseudoaneurysm:
o false aneurysm
• Large volume of blood in peritoneum cavity
• age over 55 years
• multiple injuries
• Angioembolization is an adjunct to non-operative management and generally reported to increase the success rate of non-operative management approaching 95 percent [12]
File:Angioembolism Pics.docx.png
http://onlinelibrary.wiley.com/doi/10.1002/bjs.7764/abstract [12]
• In angiographic embolization, coils or pledgets are used to reduce splenic hemorrhage, by occlusion either of the proximal splenic artery or of more distal branches (Fig.2a,b). Proximal splenic artery embolization is thought to reduce the perfusion pressure in the spleen, thereby stopping bleeding and the risk of delayed rupture or rebleeding. Peripheral embolization stops bleeding more selectively and occludes pseudoaneurysms or arteriovenous fistulas [12]
Operative Management (OM)
• Splenectomy
• Performed most splenic injuries up to 1950
• Complete removal of spleen
• Most appropriate procedure for unstable patients [12]
• Laproscopic and Open procudures
• Prone to infections
•
• Splenorrhaphy
• Suturing the spleen and non-removal
• Performed approximately 6% of the time (anything new in adult splenic ruptures)
• Grade 3 spleen injury - mesh splenorrhaphy
http://www.trauma.org/index.php/main/images_keyword/laparotomy/
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapist must be able to recognize the signs and symptoms of spleen rupture. In sports, splenic rupture is the most common cause of death due to abdominal trauma trauma, it is vital that clinicians perform a through exam of the patient.
Palpation - The spleen is located in the left upper quadrant and covered by the 9th - 11th ribs. Clinicians should check this area for pain and tenderness. Abdominal palpation should also be performed in the hook-lying position checking for tenderness, distension, guarding, and rebound tenderness. "To palpate the spleen, lift the left flank with your nondominant hand; keeping your other hand flat, depress the palpating digits just below and anteriro to the 11th and 12 ribs and ask the patient to take a deep breath. A normal healthy spleen should not be palpable."
Patient Education - Most splenic ruptures can be rapidly progressing, while others can delay hemmorrhage for hours, days, or even weeks after injury, until a suffient enough force causes rupture. It is vital that we education patients about the signs and symptoms so they can seek medical care immediately.
Post-operation: encourage ROM, ambulation, and coughing techniques (splinted coughing). Most traumatic splenic ruptures will not be seen in physical therapy.
Alternative/Holistic Management (current best evidence)[edit | edit source]
No supporting evidence for alternative/holistic management available during our search although it may exist.
Differential Diagnosis[edit | edit source]
Left kidney trauma/pathology
Rib fracture
Intestinal pathology
Musculoskeletal Involvement
Case Reports/ Case Studies
[edit | edit source]
Third-Degree Spleen Laceration in a Male Varsity Athlete
http://journals.humankinetics.com/att-back-issues/attvolume8issue3may
Splenic Rupture in Infectious Mononucleosis
http://www.annals.org/content/46/6/1184.short
Spontaneous rupture of the spleen – a fatal complication of pregnancy
http://www.ncbi.nlm.nih.gov/pubmed/7572867
Resources
[edit | edit source]
1. Mayo Clinic
http://www.mayoclinic.com/health/ruptured-spleen/DS00872
2. Medscape
http://emedicine.medscape.com/article/432823-treatment
3. Discussion Board Spleen Rupture
http://www.medhelp.org/tags/show/148977/rupture-spleen
http://www.healthboards.com/boards/general-health/698344-rib-cage-injury-ruptured-spleen.html
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1tYbWOIP0tI0rcUJrEZlcEvYw6v8cNAf2PUUAlTae95SAWDgH4|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ Encyclopædia Britannica. Encyclopædia Britannica Online Academic Edition. Encyclopædia Britannica Inc.,. Spleen. Available from: http://www.britannica.com/EBchecked/topic/560613/spleen
- ↑ 2.0 2.1 2.2 2.3 Mayo Foundation for Medical Education and Research (MFMER) 1998-2012. Ruptured Spleen. [Internet] 2012 [updated 2010 Nov 19; cited 2012 Mar 30]. Available from: http://www.mayoclinic.com/health/ruptured-spleen/DS00872
- ↑ 3.0 3.1 3.2 Debnath D, Valerio D. Education- Atraumatic rupture of the spleen in adults. J.R. Coll.Surg.Edinb. 2002;47;437-445. http://www.rcsed.ac.uk/journal/vol47_1/47100010.html (accessed 28 Mar 2012)
- ↑ Foreman B, Mackler L. Can we prevent splenic rupture for patients with infectious mononucleosis? Journal of Family Practice 2005; 54: 547
- ↑ A Dictionary of Nursing. 2008. Kehr’s Sign. 29 Mar. 2012 Available at: http://www.encyclopedia.com/doc/1O62-Kehrssign.html.
- ↑ WebMD. 2005-2012. Ruptured Spleen. [Internet] [reviewed 2009 Aug 19; cited 2012 Mar 30]. Available from: http://www.webmd.com/digestive-disorders/ruptured-spleen
- ↑ Clancy A, Tiruta C, Ashman D, Ball C, Kirkpatrick A. The song remains the same although the instruments are changing: complications following selective non-operative management of blunt spleen trauma: a retrospective review of patients at a level I trauma centre from 1996 to 2007. Journal of Trauma Management & Outcomes 2012; ISSN 1752-2897
- ↑ Webb C, Crowell K. Which vaccinations are indicated after splenectomy? Journal of Family Practice 2006;55:8. http://www.jfponline.com/Pages.asp?AID=4327&amp;amp;amp;issue=August%202006&amp;amp;amp;UID= (accessed 26 Marc 2012)
- ↑ EB Medicine, Splenic Injuries: http://www.ebmedicine.net/topics.php?paction=showTopicSeg&amp;amp;amp;topic_id=132&amp;amp;amp;seg_id=2728
- ↑ 10.0 10.1 Klepac S. Spleen Trauma Imaging. Medscape.http://emedicine.medscape.com/article/373694-overview (accessed 22 March 2012).
- ↑ 11.0 11.1 11.2 Johnson J, Splenic Injury AAST Grading System. UVMRads. UVMRads. http://uvmrads.org/sections/bodyct/87-splenic-injury-aast-grading-system?start=1 (accessed 23 March 2012
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 Skattum J, Naess P, Gaarder C. Non-operative management and immune function after splenic injury. BJS 2011;99:1;59-65. http://onlinelibrary.wiley.com/doi/10.1002/bjs.7764/abstract (accessed 28 Mar 2012)
- ↑ MD Guidlelines, Rupture of Spleen Traumatic. fckLRhttp://www.mdguidelines.com/rupture-of-spleen-traumatic (accessed 20 Mar 2012)
- ↑ University of Washington, Radiology and Imaging Services. http://uwmedicine.washington.edu/Patient-Care/Our-Services/Medical-Services/Radiology-Imaging-Services/Pages/Contrast-Extravasation.aspx (accessed 21 Mar 2012)
- ↑ Trauma.org. Care for the Injured- Massotto H. Grade 3 spleen prevention-mesh splenorrhaphy. Available: http://www.trauma.org/index.php/main/images_keyword/laparotomy (assessed 30 Mar 2012)