Quadrilateral Space Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 20: | Line 20: | ||
** humerus (lateral)<br> | ** humerus (lateral)<br> | ||
{{#ev:youtube|uiP626A5MBE}}<ref>Peter Zatezalo. Quadrilateral Space Anatomy. Available from: https://www.youtube.com/watch?v=uiP626A5MBE [last accessed 11/17/2021] </ref> | {{#ev:youtube|uiP626A5MBE}}<ref>Peter Zatezalo. Quadrilateral Space Anatomy. Available from: https://www.youtube.com/watch?v=uiP626A5MBE [last accessed 11/17/2021] </ref> | ||
Revision as of 06:49, 18 November 2021
Clinically Relevant Anatomy
[edit | edit source]
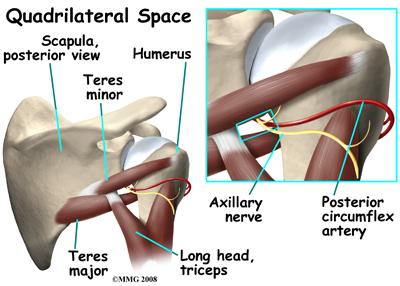
Quadrilateral space syndrome (QSS) refers to a rare condition in which neural and vascular structures are entrapped in the quadrilateral space. This space is created by the lateral head of the triceps, teres minor, teres major, and medial border of the humerus. Through this space passes the axillary nerve and the posterior circumflex humeral artery. Fibrous bands in this space are commonly though to be the cause of compression. One study showed that 14 of 16 cadavers had fibrous bands present, usually between the long head of the triceps and the teres major.[1]
- Contents of the Quadrilateral Space
- Axillary Nerve (C5 nerve root)
- innervates deltoid, teres minor, provides sensation to lateral shoulder
- Posterior Circumflex Humeral Artery
- supplies the teres minor, triceps brachii, teres major
- Axillary Nerve (C5 nerve root)
- Structures that frame the quadrilateral space
- teres minor (superior)
- teres major (inferior)
- long head of the triceps brachii (medial)
- humerus (lateral)
Mechanism of Injury / Pathological Process
[edit | edit source]
The exact mechanism and cause of the injury is still unclear at this time. However, it is often associated with overhead athletes such as pitchers, swimmers, or volleyball players who regularly put their arm in the position of abduction and external rotation. This position causes the greatest amount of compression to the QS. Because of this, the dominant shoulder is most often affected, and the syndrome is reported to be most common in active people age 20-40.[3] QSS can be caused by anything that decreases the area of the quadrilateral space. This could be caused by anatomic variations, a glenoid cyst, muscle hypertrophy, or paralabral cyst from a labrum injury. [4]
- Possible causes of QSS:
- fibrous bands
- trauma (scapular fracture)
- paralabral cysts (inferior labral tear)
- muscle hypertrophy
- benign or malignant mass
Clinical Presentation[edit | edit source]
Patients generally present with an insidious onset of diffuse shoulder pain, posterior shoulder pain, weakness, and sensation loss in the distribution of the axillary nerve. Weakness is most notable in abduction and external rotation. It's possible to have atrophy in the external rotators or more noticeably in the deltoid if the case in chronic. Patients are almost always point tender at the QS itself. [3]
Diagnostic Procedures[edit | edit source]
Selective atrophy of the teres minor muscle can be identified by MRI, which is a positive indicator of the syndrome.[5] However, MRI studies have shows that teres minor atrophy is a common finding in rotator cuff pathology, prior surgical intervention, and traction injuries with glenohumeral instability. It's also been suggested that a lidocaine block in the area of the QS and axillary nerve can be a positive diagnostic criteria if the pain is abolished. [3]
Outcome Measures[edit | edit source]
There is currently no specific outcome measure for QSS that is supported by evidence. Any shoulder outcome measure that takes into account functional use and overhead activities should be able to measure progress with QSS effectively.
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
- Thoracic Outlet Syndrome
- Cervical Radiculopathy
- Rotator Cuff Pathology
- Internal/Posterior Shoulder Impingement
- Glenohumeral Instability
- Suprascapular Nerve Injury
- Brachial Plexus Injury
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ McClelland D, Paxinos A. The anatomy of the quadrilateral space with reference to quadrilateral space syndrome [Internet]. Journal of Shoulder and Elbow Surgery. Mosby; 2007 [cited 2021Nov16]. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1058274607005009
- ↑ Peter Zatezalo. Quadrilateral Space Anatomy. Available from: https://www.youtube.com/watch?v=uiP626A5MBE [last accessed 11/17/2021]
- ↑ 3.0 3.1 3.2 Lindsay F. Quadrilateral space syndrome: a review. Journal of Shoulder and Elbow Surgery [Internet]. 2018 [cited 2021Nov16]; Available from: http://bonefix.co.nz/portals/160/images/Flynn%20Quadrangular%20space%20syndrome.pdf
- ↑ Hoskins WT. Case report quadrilateral space syndrome: A case study and ... [Internet]. British Journal of Sports Medicine . 2005 [cited 2021Nov17]. Available from: https://bjsm.bmj.com/content/bjsports/39/2/e9.full.pdf
- ↑ Linker CS, Roy EA, Eliahou R, Linda DD, Gaskin CM, Rutten MJCM, et al. Quadrilateral space syndrome: Findings at Mr Imaging. [Internet]. Radiology. 1993 [cited 2021Nov16]. Available from: https://pubs.rsna.org/doi/abs/10.1148/radiology.188.3.8351331