Proliferative Myositis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
== Definition/Description [[Image:SCM2.jpg|thumb|right]] == | == Definition/Description [[Image:SCM2.jpg|thumb|right]] == | ||
Proliferative myositis (PM) is a benign tumor which grows in skeletal muscle<ref name="Fauser et. al">Fauser C, Nahrig J, Niedermeyer H, Arnold W. Proliferative myositis: a rare pseudomalignant tumor of the head and neck. Archives of Otolaryngology - Head &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Neck Surgery [serial on the Internet]. (2008, Apr), [cited March 16, 2011]; 134(4): 437-440. Available from: CINAHL with Full Text.</ref>. It is usually 3-4 cm in diameter<ref name="Stanford" />, and is often mistaken for sarcomas (especially rhabdomyosarcoma)<ref name="Meis et. al">Meis J, Enzinger F. Proliferative fasciitis and myositis of childhood. The American Journal Of Surgical Pathology [serial on the Internet]. (1992, Apr), [cited March 16, 2011]; 16(4): 364-372. Available from: MEDLINE.</ref>. The tumor is formed by ganglion-like cells, fibroblasts, and myofibroblasts which increase the spaces between muscle fibers<ref name="Stanford" />. While etiology is unknown, it may result from injury to the muscle, fascia, or vasculature (resulting in ischemia) of the associated area<ref name="Dent et. al">Dent C, DeBoom G, Hamlin M. Proliferative myositis of the head and neck. Report of a case and review of the literature. Oral Surgery, Oral Medicine, And Oral Pathology [serial on the Internet]. (1994, Sep), [cited March 16, 2011]; 78(3): 354-358. Available from: MEDLINE.</ref>. PM generally presents in the upper extremity or trunk regions<ref name="Stanford" />. Median age of onset is 50 years<ref name="Mulier et. al" />, with rare cases reported in children<ref name="Stanford">Stanford University. Proliferative Myositis. Available at http://surgpathcriteria.stanford.edu/softfib/proliferative_myositis/printable.html. Accessed April 4, 2011</ref>. '' [Photo: PM of the SCM muscle<ref name="Fauser et. al" />]'' | Proliferative myositis (PM) is a benign tumor which grows in skeletal muscle<ref name="Fauser et. al">Fauser C, Nahrig J, Niedermeyer H, Arnold W. Proliferative myositis: a rare pseudomalignant tumor of the head and neck. Archives of Otolaryngology - Head &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Neck Surgery [serial on the Internet]. (2008, Apr), [cited March 16, 2011]; 134(4): 437-440. Available from: CINAHL with Full Text.</ref>. It is usually 3-4 cm in diameter<ref name="Stanford" />, and is often mistaken for sarcomas (especially rhabdomyosarcoma)<ref name="Meis et. al">Meis J, Enzinger F. Proliferative fasciitis and myositis of childhood. The American Journal Of Surgical Pathology [serial on the Internet]. (1992, Apr), [cited March 16, 2011]; 16(4): 364-372. Available from: MEDLINE.</ref>. The tumor is formed by ganglion-like cells, fibroblasts, and myofibroblasts which increase the spaces between muscle fibers<ref name="Stanford" />. While etiology is unknown, it may result from injury to the muscle, fascia, or vasculature (resulting in ischemia) of the associated area<ref name="Dent et. al">Dent C, DeBoom G, Hamlin M. Proliferative myositis of the head and neck. Report of a case and review of the literature. Oral Surgery, Oral Medicine, And Oral Pathology [serial on the Internet]. (1994, Sep), [cited March 16, 2011]; 78(3): 354-358. Available from: MEDLINE.</ref>. PM generally presents in the upper extremity or trunk regions<ref name="Stanford" />. Median age of onset is 50 years<ref name="Mulier et. al" />, with rare cases reported in children<ref name="Stanford">Stanford University. Proliferative Myositis. Available at http://surgpathcriteria.stanford.edu/softfib/proliferative_myositis/printable.html. Accessed April 4, 2011</ref>. '' [Photo: PM of the SCM muscle<ref name="Fauser et. al" />]'' | ||
== Prevalence<br> == | == Prevalence<br> == | ||
According to an article written by Fauser ''et. al'' in 2008, approximately 100 cases of PM had been published in the literature<ref name="Fauser et. al" />. According to Jassar and Kumar (2005), approximately 1000 cases have been reported<ref name="Kumar">Jassar A, Kumar V. Proliferative myositis--a case report. Indian Journal Of Pathology &amp; Microbiology [serial online]. January 2005;48(1):33-35. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2011.</ref>.<br> | According to an article written by Fauser ''et. al'' in 2008, approximately 100 cases of PM had been published in the literature<ref name="Fauser et. al" />. According to Jassar and Kumar (2005), approximately 1000 cases have been reported<ref name="Kumar">Jassar A, Kumar V. Proliferative myositis--a case report. Indian Journal Of Pathology &amp;amp; Microbiology [serial online]. January 2005;48(1):33-35. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2011.</ref>.<br> | ||
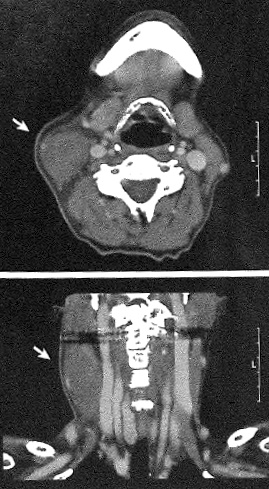
== Characteristics/Clinical Presentation<ref name="Fauser et. al" /><ref name="Kumar" /><ref name="Sharma">Sharma S and Banerjee AK. Proliferative Myositis: Report of Two Cases. Indian Journal of Pathology &amp;amp; Microbiology; an Official Organ of Indian Association of Pathologists and Microbiologists [serial online]. 1985;28(3):273-276.</ref><ref name="Turner">Turner R, Robson A, Motley R. Proliferative myositis: an unusual cause of multiple subcutaneous nodules. Clinical and Experimental Dermatology 1997;22:101-103</ref> [[Image:Neck CT.jpg|thumb]] == | == Characteristics/Clinical Presentation<ref name="Fauser et. al" /><ref name="Kumar" /><ref name="Sharma">Sharma S and Banerjee AK. Proliferative Myositis: Report of Two Cases. Indian Journal of Pathology &amp;amp;amp; Microbiology; an Official Organ of Indian Association of Pathologists and Microbiologists [serial online]. 1985;28(3):273-276.</ref><ref name="Turner">Turner R, Robson A, Motley R. Proliferative myositis: an unusual cause of multiple subcutaneous nodules. Clinical and Experimental Dermatology 1997;22:101-103</ref> [[Image:Neck CT.jpg|thumb]] == | ||
*Solid tumor within skeletal muscle | *Solid tumor within skeletal muscle | ||
| Line 42: | Line 42: | ||
== Systemic Involvement == | == Systemic Involvement == | ||
Mulier et. al reported a case in which one patient had a mild fever (37.5 degrees C or 100 degrees F)<ref name="Mulier et. al" />. No other cases of systemic symptoms have been reported. | Mulier et. al reported a case in which one patient had a mild fever (37.5 degrees C or 100 degrees F)<ref name="Mulier et. al" />. No other cases of systemic symptoms have been reported. | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Revision as of 14:12, 6 April 2011
Original Editors - Billie Rehberg from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description [edit | edit source]
Proliferative myositis (PM) is a benign tumor which grows in skeletal muscle[1]. It is usually 3-4 cm in diameter[2], and is often mistaken for sarcomas (especially rhabdomyosarcoma)[3]. The tumor is formed by ganglion-like cells, fibroblasts, and myofibroblasts which increase the spaces between muscle fibers[2]. While etiology is unknown, it may result from injury to the muscle, fascia, or vasculature (resulting in ischemia) of the associated area[4]. PM generally presents in the upper extremity or trunk regions[2]. Median age of onset is 50 years[5], with rare cases reported in children[2]. [Photo: PM of the SCM muscle[1]]
Prevalence
[edit | edit source]
According to an article written by Fauser et. al in 2008, approximately 100 cases of PM had been published in the literature[1]. According to Jassar and Kumar (2005), approximately 1000 cases have been reported[6].
Characteristics/Clinical Presentation[1][6][7][8] [edit | edit source]
- Solid tumor within skeletal muscle
- Rapidly enlarging (often noticeably larger within several days time)
- Localized inflammation
- No lymph node enlargement
- No significant laboratory results
- Possible localized pain
[Photo: Computerized Tomography of PM of the SCM muscle[1]]
Associated Co-morbidities[edit | edit source]
No associated co-morbidities have been reported.
Medications[edit | edit source]
Ibuprofen and other NSAIDs may be beneficial in decreasing pain and inflammation.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
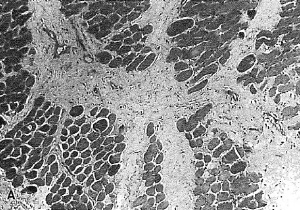
Proliferative Myositis is diagnosed based on biopsy[1]. The following list, taken directly from the Stanford University School of Medicine page on PM, are histologic and immunologic characteristics of PM which are used in its diagnosis:
o Relatively normal muscle fibers separated by expanded myxoid connective tissue
o Produces distinctive checkerboard pattern
o No evidence of muscle damage
o No sarcolemmal proliferation
o No multinucleation
o No nuclear enlargement
o No necrosis
o Connective tissue space between fibers contains reactive cells resembling those seen in nodular fasciitis and proliferative fasciitis
o Spindled and stellate fibroblasts and myofibroblasts
o Vesicular nuclei
o No cytologic atypia
o Actin positive
o CD68 variable [Image: "checkerboard" arrangement
o S100, desmin negative of cells often seen in PM biopsies[5]]
o Ganglion-like cells
o Characteristic feature of this process
o Large round regular nuclei
o Occasional binucleate and trinucleate cells may be seen
o Prominent nucleoli
o Dispersed chromatin
o Basophilic to amphophilic cytoplasm
o May be clustered and may mold each other
o Factor XIIIa positive
o Actin, CD68 negative to focal/weak
o Desmin, keratin, S100, neuron specific enolase negative
o Mitotic figures frequent
o No atypical mitotic figures [2]
Etiology/Causes[edit | edit source]
While etiology is unknown, PM may result from injury to the muscle, fascia, or vasculature (resulting in ischemia) of the associated area[4].
Systemic Involvement[edit | edit source]
Mulier et. al reported a case in which one patient had a mild fever (37.5 degrees C or 100 degrees F)[5]. No other cases of systemic symptoms have been reported.
Medical Management (current best evidence)[edit | edit source]
Proliferative Myositis is a self-limiting pathology, meaning that the growth of the tumor will eventually stop. While spontaneous resolution of the tumor has been reported[1][8][5], surgical excision is the only treatment and recurrence following excision is rare[2].
Physical Therapy Management (current best evidence)[edit | edit source]
It has been theorized that PM is a precursor to heterotopic ossification or myositis ossificans[6]. Thus, aggressive range of motion and strengthening exercises should be avoided to prevent possible aggravation of the condition while the tumor is still enlarging. ROM and strengthening exercises and modalities to regain normal muscular function and decrease pain following surgery may be indicated.
Alternative/Holistic Management (current best evidence)[edit | edit source]
No formal report of alternative/holistic management of PM exists. In verified cases of PM, the "wait and see" approach carries no risk, as PM is a self-limiting process and spontaneous regression has been reported[1][8][5].
Differential Diagnosis[5][3][2][edit | edit source]
- Myositis Ossificans
- Neoplasms (especially rhabdomyosarcomas)
- Proliferative fasciitis
- Nodular fasciitis
- Fibromatosis
- Ganglioneuroblastoma or ganglioneuroma
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Fauser C, Nahrig J, Niedermeyer H, Arnold W. Proliferative myositis: a rare pseudomalignant tumor of the head and neck. Archives of Otolaryngology - Head &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Neck Surgery [serial on the Internet]. (2008, Apr), [cited March 16, 2011]; 134(4): 437-440. Available from: CINAHL with Full Text.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Stanford University. Proliferative Myositis. Available at http://surgpathcriteria.stanford.edu/softfib/proliferative_myositis/printable.html. Accessed April 4, 2011
- ↑ 3.0 3.1 Meis J, Enzinger F. Proliferative fasciitis and myositis of childhood. The American Journal Of Surgical Pathology [serial on the Internet]. (1992, Apr), [cited March 16, 2011]; 16(4): 364-372. Available from: MEDLINE.
- ↑ 4.0 4.1 Dent C, DeBoom G, Hamlin M. Proliferative myositis of the head and neck. Report of a case and review of the literature. Oral Surgery, Oral Medicine, And Oral Pathology [serial on the Internet]. (1994, Sep), [cited March 16, 2011]; 78(3): 354-358. Available from: MEDLINE.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Mulier S, Stas M, Delabie J, Lateur L, Gysen M, De Wever I, et al. Proliferative myositis in a child. Skeletal Radiology [serial on the Internet]. (1999, Dec), [cited March 16, 2011]; 28(12): 703-709. Available from: MEDLINE.
- ↑ 6.0 6.1 6.2 Jassar A, Kumar V. Proliferative myositis--a case report. Indian Journal Of Pathology &amp; Microbiology [serial online]. January 2005;48(1):33-35. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2011.
- ↑ Sharma S and Banerjee AK. Proliferative Myositis: Report of Two Cases. Indian Journal of Pathology &amp;amp; Microbiology; an Official Organ of Indian Association of Pathologists and Microbiologists [serial online]. 1985;28(3):273-276.
- ↑ 8.0 8.1 8.2 Turner R, Robson A, Motley R. Proliferative myositis: an unusual cause of multiple subcutaneous nodules. Clinical and Experimental Dermatology 1997;22:101-103