Post Concussion Syndrome Case Study: Following a Fall: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
<blockquote>'''Subjective'''</blockquote>'''''History of Present Illness''' -'' | <blockquote>'''Subjective'''</blockquote>'''''History of Present Illness''' -'' | ||
'''''Past Medical History''' - Healthy prior to injury; no previous trauma, surgeries, or other serious health conditions/comorbidities noted | '''''Past Medical History''''' - Healthy prior to injury; no previous trauma, surgeries, or other serious health conditions/comorbidities noted | ||
'''''Major Symptoms''''' | '''''Major Symptoms''''' | ||
| Line 14: | Line 14: | ||
# Dizziness - occurs when moving head side to side or up and down | # Dizziness - occurs when moving head side to side or up and down | ||
'''''Medications''' - No medications; occasionally takes Tylenol 2-3 days per week if headaches become unbearable (i.e., 8/10 pain) | '''''Medications''' -'' No medications; occasionally takes Tylenol 2-3 days per week if headaches become unbearable (i.e., 8/10 pain) | ||
'''''Health Habits''' - Non-smoker; consumption of wine (2-3 glasses/week) prior to the injury - has ceased drinking any alcohol post-injury | '''''Health Habits''' -'' Non-smoker; consumption of wine (2-3 glasses/week) prior to the injury - has ceased drinking any alcohol post-injury | ||
'''''Social History''' -'' Registered Nurse (RN) for 11 years; yoga practitioner for 10 years and yoga teacher for 5 years; currently living in a two-storey townhouse with fiancé. | '''''Social History''' -'' Registered Nurse (RN) for 11 years; yoga practitioner for 10 years and yoga teacher for 5 years; currently living in a two-storey townhouse with fiancé. | ||
'''''Current Level of Function''' - | '''''Current Level of Function''' -'' Able to ambulate normally at home and perform simple chores independently, sleep quality has decreased markedly since the injury: has trouble falling asleep and wakes up 2-3 times on average at night; able to drive during day time, but has difficulty at night time due to light sensitivity (i.e., bright lights from car); decreased concentration and memory has been noted; more likely to become emotional over relatively trivial issues (i.e., spilling milk); tolerance for moderately challenging activities (such as work) has decreased drastically due to headaches, decreased cognitive capacity, moodiness, etc. Although the major complaint is of headache, the patient also reports slight dizziness when looking around frequently (i.e., such as looking for a product during grocery shopping).<blockquote>'''Objective'''</blockquote>'''''Blood Pressure''''' - 108mmHg/66mmHg (within normal limits) | ||
'''''Heart Rate''' - 66bpm (within normal limits) | '''''Heart Rate''''' - 66bpm (within normal limits) | ||
'''''General Observation''' - no significant postural abnormalities | '''''General Observation''''' - no significant postural abnormalities | ||
'''''Gait''' - normal | '''''Gait''''' - normal | ||
'''''Speech''' - normal speech comprehension and fluency | '''''Speech''''' - normal speech comprehension and fluency | ||
'''''Upper Limb scan exam''' - normal | '''''Upper Limb scan exam''''' - normal | ||
'''''Upper Limb Neurological exam''''' - dermatomes, myotomes & reflexes all normal | '''''Upper Limb Neurological exam''''' - dermatomes, myotomes & reflexes all normal | ||
'''''Cranial Nerve Testing''' - normal | '''''Cranial Nerve Testing''''' - normal | ||
'''''Cervical Active ROM''' - all ranges within normal limits | '''''Cervical Active ROM''' -'' all ranges within normal limits | ||
'''''Superficial and Deep Neck Flexors''''' - activation and strength both normal | '''''Superficial and Deep Neck Flexors''''' - activation and strength both normal | ||
'''''Palpation''' - increased tightness bilaterally in upper fibre trapezius and levator scapulae | '''''Palpation''' -'' increased tightness bilaterally in upper fibre trapezius and levator scapulae<blockquote>'''Outcome Measures'''</blockquote>'''''Static Balance''''' | ||
* | * | ||
''[[Functional Gait Assessment| | ''[[Functional Gait Assessment|'''Functional Gait Assessment''']]'' | ||
* <u>Score</u>: 24/30, moderate impairment | * <u>Score</u>: 24/30, moderate impairment | ||
* Difficulty with gait with horizontal and vertical head turns category | * Difficulty with gait with horizontal and vertical head turns category | ||
* Experienced increased dizziness | * Experienced increased dizziness | ||
'' | '''''The Headache Impact Test''''' | ||
* <u>Score</u>: 59, substantial impact on health related quality of life | * <u>Score</u>: 59, substantial impact on health related quality of life | ||
* Score range: 36-78 | * Score range: 36-78 | ||
'' | '''''Dizziness Handicap Inventory''''' | ||
* <u>Score</u>: 45/96, moderate handicap | * <u>Score</u>: 45/96, moderate handicap | ||
* Physical, Emotional, Functional subscales | * Physical, Emotional, Functional subscales | ||
''[https://physio-pedia.com/Vestibular/Oculomotor_Motor_Screening_(VOMS)_Assessment | ''[https://physio-pedia.com/Vestibular/Oculomotor_Motor_Screening_(VOMS)_Assessment '''Vestibular-Ocular Screening (VOMS) Test''']'' | ||
* | * | ||
== '''Clinical Impression''' == | == '''Clinical Impression''' == | ||
| Line 73: | Line 73: | ||
== '''Intervention''' == | == '''Intervention''' == | ||
<blockquote>'''Goals'''</blockquote><blockquote>'''Education'''</blockquote><blockquote>'''Manual Therapy'''</blockquote><blockquote>'''Exercise'''</blockquote>''Balance'' | <blockquote>'''Goals'''</blockquote> | ||
# Reduce headache severity at rest from a 2/10 to 0/10 by the end of the 3rd week of treatment | |||
# Be able to maintain static single leg stance balance bilaterally with eyes closed for 30 seconds by the end of the 4th week of treatment | |||
# Be able to turn head while walking without causing nausea or dizziness by the end of the 6th week of treatment | |||
<blockquote>'''Education'''</blockquote><blockquote>'''Manual Therapy'''</blockquote>'''Soft Tissue Release Technique''' | |||
* Upper fibers trapezius (bilateral) | |||
* Levator Scapulae (bilateral) | |||
<u>Parameters:</u> Passive approach with gliding pressure along muscle fibres in multiple planes, 10 reps total each side | |||
<u>Progression</u>: Can progress to performing active-assisted and then active STR | |||
'''Trigger Point Release Technique''' | |||
* Upper fibers Trapezius (bilateral) | |||
* Levator Scapulae (bilateral) | |||
<u>Parameters:</u> Apply pressure on trigger points for 30 seconds, 2 reps, each side<blockquote>'''Exercise'''</blockquote>''Balance'' | |||
''Stretching'' | ''Stretching'' | ||
| Line 79: | Line 94: | ||
''Vestibular-ocular Reflex Specific Exercise'' | ''Vestibular-ocular Reflex Specific Exercise'' | ||
== '''Outcome''' == | == '''Outcome''' == | ||
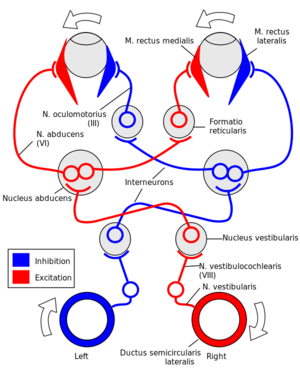
<blockquote>'''Status Change Post Intervention'''</blockquote><blockquote>'''Outcome Measures'''</blockquote><blockquote>'''Discharge Plan'''</blockquote>[[File:Vestibular-Ocular Reflex.png|thumb|When the head moves to the right, the right semicircular canals detect this movement, sending an excitatory signal to the ipsilateral vestibular nucleus, subsequently to the left abducens nucleus which causes excitation of left lateral rectus and right medial rectus - keeping eye gaze in the same direction as the head moves to the right.]] | |||
[[File:Vestibular-Ocular Reflex.png|thumb|When the head moves to the right, the right semicircular canals detect this movement, sending an excitatory signal to the ipsilateral vestibular nucleus, subsequently to the left abducens nucleus which causes excitation of left lateral rectus and right medial rectus - keeping eye gaze in the same direction as the head moves to the right.]] | |||
== '''Discussion''' == | == '''Discussion''' == | ||
| Line 94: | Line 103: | ||
# Emotional | # Emotional | ||
# All of the above | # All of the above | ||
Post concussion symptoms typically resolve in _________ days | Post concussion symptoms typically resolve in _________ days among adults. | ||
# 4-6 | # 4-6 | ||
# 7-10 | # 7-10 | ||
Revision as of 04:45, 12 May 2020
Abstract[edit | edit source]
Introduction[edit | edit source]
Client Characteristics[edit | edit source]
Examination Findings[edit | edit source]
Subjective
History of Present Illness -
Past Medical History - Healthy prior to injury; no previous trauma, surgeries, or other serious health conditions/comorbidities noted
Major Symptoms
- Headache - constant, dull, diffuse headache 2/10 at rest ***
- Dizziness - occurs when moving head side to side or up and down
Medications - No medications; occasionally takes Tylenol 2-3 days per week if headaches become unbearable (i.e., 8/10 pain)
Health Habits - Non-smoker; consumption of wine (2-3 glasses/week) prior to the injury - has ceased drinking any alcohol post-injury
Social History - Registered Nurse (RN) for 11 years; yoga practitioner for 10 years and yoga teacher for 5 years; currently living in a two-storey townhouse with fiancé.
Current Level of Function - Able to ambulate normally at home and perform simple chores independently, sleep quality has decreased markedly since the injury: has trouble falling asleep and wakes up 2-3 times on average at night; able to drive during day time, but has difficulty at night time due to light sensitivity (i.e., bright lights from car); decreased concentration and memory has been noted; more likely to become emotional over relatively trivial issues (i.e., spilling milk); tolerance for moderately challenging activities (such as work) has decreased drastically due to headaches, decreased cognitive capacity, moodiness, etc. Although the major complaint is of headache, the patient also reports slight dizziness when looking around frequently (i.e., such as looking for a product during grocery shopping).
Objective
Blood Pressure - 108mmHg/66mmHg (within normal limits)
Heart Rate - 66bpm (within normal limits)
General Observation - no significant postural abnormalities
Gait - normal
Speech - normal speech comprehension and fluency
Upper Limb scan exam - normal
Upper Limb Neurological exam - dermatomes, myotomes & reflexes all normal
Cranial Nerve Testing - normal
Cervical Active ROM - all ranges within normal limits
Superficial and Deep Neck Flexors - activation and strength both normal
Palpation - increased tightness bilaterally in upper fibre trapezius and levator scapulae
Outcome Measures
Static Balance
- Score: 24/30, moderate impairment
- Difficulty with gait with horizontal and vertical head turns category
- Experienced increased dizziness
The Headache Impact Test
- Score: 59, substantial impact on health related quality of life
- Score range: 36-78
Dizziness Handicap Inventory
- Score: 45/96, moderate handicap
- Physical, Emotional, Functional subscales
Vestibular-Ocular Screening (VOMS) Test
Clinical Impression[edit | edit source]
Diagnosis
36 year-old female presenting with post concussion syndrome two weeks after diagnosis of concussion from fall while ice skating on Jan 2, 2020. Patient has bilateral tightness in upper trapezius and levator scapulae, impaired bilateral single leg stance with eyes closed, and gait impacted by vertical and horizontal head turns. Symptoms are interfering with return to work, driving at night, getting a restful sleep, and grocery shopping. Patient is an excellent candidate for physiotherapy.[edit | edit source]
Problem List
- Disturbance in quality of sleep (unable to sleep straight through the night)
- Inability to drive at night due to light sensitivity
- Experiencing dizziness with dual tasks when walking and impacting performance in ADLs
- Unable to return to work due to symptoms from post concussion syndrome
- Tightness bilaterally in upper fibre traps and levator scapula
- Impaired single leg stance with eyes closed
- Gait impacted with vertical and horizontal head turns
- Headaches impacting health related quality of life
- Headache with all tasks on the VOMS
- Vestibular ocular reflex horizontal and vertical elicits dizziness and nausea along with headache
- Mild dizziness during visual motion sensitivity test
- Increase in pain when performing activities with head movements
Intervention[edit | edit source]
Goals
- Reduce headache severity at rest from a 2/10 to 0/10 by the end of the 3rd week of treatment
- Be able to maintain static single leg stance balance bilaterally with eyes closed for 30 seconds by the end of the 4th week of treatment
- Be able to turn head while walking without causing nausea or dizziness by the end of the 6th week of treatment
Education
Manual Therapy
Soft Tissue Release Technique
- Upper fibers trapezius (bilateral)
- Levator Scapulae (bilateral)
Parameters: Passive approach with gliding pressure along muscle fibres in multiple planes, 10 reps total each side
Progression: Can progress to performing active-assisted and then active STR
Trigger Point Release Technique
- Upper fibers Trapezius (bilateral)
- Levator Scapulae (bilateral)
Parameters: Apply pressure on trigger points for 30 seconds, 2 reps, each side
Exercise
Balance
Stretching
Vestibular-ocular Reflex Specific Exercise
Outcome[edit | edit source]
Status Change Post Intervention
Outcome Measures
Discharge Plan
Discussion[edit | edit source]
Self Study Questions[edit | edit source]
The consequences of concussions can include which of the following?
- Physical
- Cognitive
- Emotional
- All of the above
Post concussion symptoms typically resolve in _________ days among adults.
- 4-6
- 7-10
- 15-20
- 10-12
The vestibular oculomotor screening test (VOMS) test the following?
- Convergence
- Smooth pursuits
- Visual motion sensitivity
- a and b
- a and c
- a, b, and c






