Physiotherapy management strategies in people with schizophrenia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 159: | Line 159: | ||
It is interesting to see that perspectives of those living with schizophrenia are very similar to those providing care to people with schizophrenia. It would appear that the symptoms of schizophrenia, including both positive (hearing voices) and negative (lack of motivation), play a significant part in stopping individuals engaging in physical activity. Along with this, side effects of medication were identified as a major barrier by 27% of the physiotherapists as well as by the patients themselves (e.g.weight gainand increased appetite). | It is interesting to see that perspectives of those living with schizophrenia are very similar to those providing care to people with schizophrenia. It would appear that the symptoms of schizophrenia, including both positive (hearing voices) and negative (lack of motivation), play a significant part in stopping individuals engaging in physical activity. Along with this, side effects of medication were identified as a major barrier by 27% of the physiotherapists as well as by the patients themselves (e.g.weight gainand increased appetite). | ||
<u>'''Psychosocial Barriers'''</u><br>Psychosocial barriers have psychological components and social components. The participants living with schizophrenia had pre-conceived misconceptions regarding physical activity and believed that they had to work at their maximum otherwise it was completely pointless and there was no benefit (Rastad et al. 2014). This was also the opinion of 11% of the physiotherapists who felt a lack of understanding of the benefits of physical activity was a major barrier. Lack of confidence, fear of failure and difficulties interpreting new information and feelings from the body, e.g. increased heart rate as a result of exercise, were other psychosocial barriers identified by individuals living with schizophrenia. Participants admitted that they were afraid to attempt physical activity in case they could not manage or achieve the results they hoped for. One participant said: '''“If I go on with it without any results, then I’m only going to make myself unhappy because I’m not succeeding…” '''Similarly low self-esteem and low confidence were identified as barriers by 11% of the physiotherapists in the study. | <u>'''Psychosocial Barriers'''</u><br>Psychosocial barriers have psychological components and social components. The participants living with schizophrenia had pre-conceived misconceptions regarding physical activity and believed that they had to work at their maximum otherwise it was completely pointless and there was no benefit (Rastad et al. 2014). This was also the opinion of 11% of the physiotherapists who felt a lack of understanding of the benefits of physical activity was a major barrier. Lack of confidence, fear of failure and difficulties interpreting new information and feelings from the body, e.g. increased heart rate as a result of exercise, were other psychosocial barriers identified by individuals living with schizophrenia. Participants admitted that they were afraid to attempt physical activity in case they could not manage or achieve the results they hoped for. One participant said: '''“If I go on with it without any results, then I’m only going to make myself unhappy because I’m not succeeding…” '''Similarly low self-esteem and low confidence were identified as barriers by 11% of the physiotherapists in the study. | ||
Personal/environmental Barriers<br>The finally category of barriers address personal factors and environmental factors. It was reported by a number of participants that they found getting to the exercise sessions or gyms difficult due to transport difficulty arranging or being able to afford transport (Rastad et al. 2014). Linked into this, a number reported having financial difficulties as a result of gambling and as such were unable to afford a gym membership. 10% of the physiotherapists who responded also agreed with this and recognised financial problems as another barrier to engaging in physical activity.<br>Hopefully this section of the wiki has given you an insight into personal views and experiences of people living with schizophrenia but also the physiotherapists who treat them. There are limitations of these studies: The study by Rastad et al. (2014) was conducted in an outpatient setting with a relatively small number of participants (20) recruited from 3 cities in Sweden. As it was conducted in an outpatient setting only, the results are unlikely to be representative of individuals in in-patient settings. Also, the availability of medical and psychological treatments for patients with schizophrenia varies among countries and as such, the participant’s experiences will not be the same worldwide. The study by Soundy et al. (2014) also had limitations. The analysis assumed that patients were compliant with their medications – non adherence to medication would significantly impact the main barriers that were identified. Also a physiotherapist’s personal habits in regard to PA could influence his/her enthusiasm/effort to promote PA to patients and could have influenced their responses in the survey. <br>Despite the limitations, a number of clear themes have been identified. Although the results may not be truly generalizable, the barriers identified are vital to consider when trying to promote and develop physical activity programmes or interventions with patients. Both of these studies also addressed potential strategies that could help facilitate engagement in physical activity and they will be discussed briefly in the next section. <br><br><br><br> | Personal/environmental Barriers<br>The finally category of barriers address personal factors and environmental factors. It was reported by a number of participants that they found getting to the exercise sessions or gyms difficult due to transport difficulty arranging or being able to afford transport (Rastad et al. 2014). Linked into this, a number reported having financial difficulties as a result of gambling and as such were unable to afford a gym membership. 10% of the physiotherapists who responded also agreed with this and recognised financial problems as another barrier to engaging in physical activity.<br>Hopefully this section of the wiki has given you an insight into personal views and experiences of people living with schizophrenia but also the physiotherapists who treat them. There are limitations of these studies: The study by Rastad et al. (2014) was conducted in an outpatient setting with a relatively small number of participants (20) recruited from 3 cities in Sweden. As it was conducted in an outpatient setting only, the results are unlikely to be representative of individuals in in-patient settings. Also, the availability of medical and psychological treatments for patients with schizophrenia varies among countries and as such, the participant’s experiences will not be the same worldwide. The study by Soundy et al. (2014) also had limitations. The analysis assumed that patients were compliant with their medications – non adherence to medication would significantly impact the main barriers that were identified. Also a physiotherapist’s personal habits in regard to PA could influence his/her enthusiasm/effort to promote PA to patients and could have influenced their responses in the survey. <br>Despite the limitations, a number of clear themes have been identified. Although the results may not be truly generalizable, the barriers identified are vital to consider when trying to promote and develop physical activity programmes or interventions with patients. Both of these studies also addressed potential strategies that could help facilitate engagement in physical activity and they will be discussed briefly in the next section. <br><br><br><br> | ||
| Line 165: | Line 165: | ||
<br> | <br> | ||
<br> | <br> | ||
== Communication strategies == | == Communication strategies == | ||
Revision as of 22:17, 5 January 2016
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Amber McNeill, Amy Westley, Emma Moisey, Fiona Bartholomew, Sally Phimister, Rucha Gadgil, Kim Jackson, Jane Hislop, 127.0.0.1, Admin, WikiSysop, Claire Knott and Amanda Ager
Introduction[edit | edit source]
Aims and Learning Outcomes[edit | edit source]
Aims:
1. To provide final year physiotherapy students and newly qualified physiotherapy graduates with an online learning resources which will develop their knowledge and understanding of schizophrenia and its impact on the individual.
2. To enable final year students and newly qualified physiotherapy graduates to develop their knowledge and awareness of physiotherapy management strategies for people/adults with schizophrenia.
Learning outcomes:
By the end of this online learning resource you should be able to:
1. Identify and evaluate the biopsychosocial impact of schizophrenia on the individual.
2. Explain the effects of the common medications used in the management of schizophrenia and how these effects can impact physiotherapy management.
3. Critically appraise the evidence underpinning some of the key physiotherapy management approaches for schizophrenia and reflect on how the could be used in practice.
4. Select evidence informed communication strategies to be able to interact effectively with individuals with schizophrenia.
What is Mental Health?[edit | edit source]
Why is There a Need for This Physiopedia Page?[edit | edit source]
An Overview of Schizophrenia[edit | edit source]
Medications[edit | edit source]
Introduction to Schizophrenia medication[edit | edit source]
Patients with mental health conditions may need medication to help with any symptoms that they are experiencing to live life normally. In the UK 2.75 million people go to the GP for a mental health condition every year which accounts for one in four GP consultations (Lee and Lyon 2009). Common conditions that require medication are depression, anxiety, schizophrenia, and bipolar disorder. Schizophrenia can require 1.5-3% of a health budget spending (Nasrallah et al 2015). There are five main sub branches of psychotropic medications for managing the effects of mental health conditions. They are: antipsychotics, antidepressants, tranquillisers/sleeping pills, mood stabilisers and beta blockers (MIND 2015). Each patient is different and may react differently to different medications. Mind.org.uk has an extensive A-Z on drugs used in mental health. Physiotherapists need to be able to understand the effects these drugs will have on the patients and how it may limit their interaction with physical management. During an assessment or treatment session a Physiotherapist also needs to be aware of how all these medications will affect cognition, proprioception and the patients’ body image.
First Line of Treatment[edit | edit source]
Patients with Schizophrenia are more susceptible to the side effects of medication like weight gain, movement disorder and metabolic effects.
Before medication is offered bio-psychosocial interventions must be tried. Medication has an antagonistic effect on dopamine receptors in the mesolimbic system. Dopamine is associated with positive side effects of Schizophrenia (hallucinations, delusions, thought disorder). Antipsychotics don’t get rid of the disorder but make the symptoms more manageable. The drugs are not specific and do also antagonise acetycholine, histamine and noradrenaline and serotonin receptors. This can have positive and negative results, for some the over sedation can be difficult and for others it can help with sleep disorders (histamine)
Antipsychotic medication: haloperidol and chlorpromazine hydrochloride are typical first generation drugs (FGA).
Second generation drugs (SGA): olanzapine, quetapine, risperidone
New drug aripiprazole, agonist of dopamine receptor (third generation TGA)
Most common FGA side effects are extrapyramidal (involuntary). Some experience akathisia and dystonia which are sometimes misdiagnosed as aggression (Pringle 2013).
Types of Medication[edit | edit source]
Antipsychotics
The basic aims of antipsychotics are to help the patient feel better or happier without feeling drowsy, alleviate hallucinations and delusions, help patients think clearly, help with extreme mood swings (Manic depressive disorder) and help with severe depression. Most antipsychotics affect neurotransmitter levels like dopamine in the brain. Overproduction of dopamine has been linked to hallucinations, delusions and thought disorder. (Royal Collage of Psychiatrist 2015). Patients taking antipsychotics will need extra physical prompting when undertaking exercises. Problems with proprioception will need to be addressed with verbal queues and physical prompts.
Antidepressants
Antidepressents help patients alleviate depression and its symptoms. Even though it is not fully understood It is known that two chemicals involved in depression are Serotonin and Noradrenaline. Anti depressants are used in moderate to severe depression, anxiety and panic attacks, OCD, Chronic pain, eating disorders and PTSD. Common antidepressants are: amitriptyline, clomipramine, citalopram, fluoxetine, phenelzine and venlafaxine. (RCPSYCH 2015).
Tranquilisers/ sleeping pills
Tranquilisers are used for patients to improve sleep patterns and for anxiety disorders (anxiolytics). They have a sedative effect due to an increase in GABA (gamma amino butyric acid) a neurotransmitter. This causes areas of the brain responsible for rational thought, memory, emotions and breathing to slow down. These medications shouldn’t be used long term as patients can become addicted, CBT may be more effective for long term management (MIND 2015). Common tranquilisers are benzodiazepines: nitrazepam, flurazepam, loprazolam, lormetazepam and temazepam. Diazepam is commonly used to treat anxiety and insomnia (BNF 2014). Accommodating for patients who are taking tranquillisers may include clear and concise instructions as concentration levels may be low. Timing treatments around taking medication is always important but finding the right time for a patient is necessary. Finding out patient preferences to time of day for treatment is also important as some may find exercises in the morning more difficult compared to the evening or vice versa.
Mood stabilisers
Mood stabilisers allow patients who experience very high and low moods to experience a more balanced life. They are used for patients as a long term treatment option with conditions such as manic depressive disorder, Drugs like lithium, valproate and carbamazepine are examples of mood stabilisers. The side effects of these drugs can make patients very thirsty. Some patients report that the drugs limit their creativity and flatten their personality. This might combat the mood swings but changes their self perspective and this can be very difficult for patients to deal with (MIND 2015). Lithium is a very effective mood stabiliser and is prescribed as a prophylactic as it has unique anti-suicidal properties. Patients need to have good kidney function as it is an element that cannot be metabolised by the body. Patients also experienced weight gain which will effect their self esteem and body image (Bschor 2014). Unfortunately lithium can be toxic in the long term and cause liver failure from fatty liver disease (LIVESTRONG 2015).
Beta blockers
Beta Blockers are beta-adrenoreceptor blocking agents used for decreasing heart rate by blocking adrenaline receptors (NHS 2015). In mental health they are used for patients with anxiety. They can control rapid heartbeat, shaking, trembling, blushing and sweating. Propranalol is an example of a beta blocker commonly used for anxiety (anxieties.com 2015). Some users may feel light headed so therapies that involve moving from lying to sitting/standing will need to be carefully administered for patients using beta blockers.
Pause here and jot down any medications you have come across on placements or in your studies. Are they similar to any here? Why do you think understanding the different medication groups is important?
Physiological Effects of Schizophrenic Medication on the Patient[edit | edit source]
Common reported side effects of psychotropic medications are: weight gain, impotence, insomnia, chronic sedation and lack of ability to concentrate in activities of daily living. This has lead to 90% of patients not adhering to medication strategies. Patients can use self reported questionnaires, such as the Glasgow antipsychotic side effect scale, to let health professionals know how the medication is affecting their daily life. These questionnaires can improve effective communication between the patient and their health care provider (Ashoorian et al 2014). Poor physical health and low socio-economic position are associated with poor mental health. Physical activity has been linked to a reduced use of psychotropic medications in middle aged men and women (Lahti et al 2013). Personally tailored exercise regimes are important because all patients will have different side effects from medication (Richardson et al 2005). Some patients with schizophrenia find it difficult to recognise their bodies and some have proprioception issues. It can sometimes be related to the medication but as schizophrenia is a neurological disorder patients have a physiological reason for proprioception issues (Everett et al 1995)
For patients with schizophrenia cognitive impairment can make functional rehabilitation much more difficult as this type of impairment is not affected by antipsychotics. In a study by Michalopoulou et al (2013) they looked at combining antipsycotics and cognitive remediation. Patients find having meaningful relationships, keeping employment and living independently difficult due to their impaired cognition. It is believed that the cortical neural circuits required for cognition are impaired. Minocycline, modafinil and galantamine have shown positive outcomes on cognition. It in not clear though if the effects of the drugs are maintained after the course has been completed. This means that there might not be a translation to functional ability. Activity was having an effect on the plasticity of neural tissue in some studies. The activity had an effect on seratonin release. This paper recommends CBT and medication as the best way to manage cognitive impairment. The implications for physiotherapy would be understanding each patients level of impairment and understanding that they might struggle with directions or remembering exercise sets. As well as understanding what methods a patient is using to manage their symptoms can aid functional rehab.
After reading this think about what you have seen on placements or read about whilst studying, have you seen any of these effects? How would you manage the side effects?
Write down a possible treatment plan for a patient with some of the side effects stated above. Consider your environment, equipment and how long you would have to treat the patient. If you have not experienced this or have not read about these side effects at all, pause here and take time to research some of them.
Challenges to Physiotherapy Management[edit | edit source]
Many patients don't adhere to their medication programmes which can make symptoms worse leading to functional problems. Participants in a study by Boardman et al (2014) found they were missing 7.8 doses on average at their base line. Taking part in a peer support group to encourage each other to take their medication patients found by week 8 of the study their adherence had improved significantly to only 1.3 missed doses. This proved that peer support improved adherence greatly. Maybe a Physiotherapists role may not be physical when it comes to medication adherence. Just by using verbal encourgement the patients might get benefit out of a Physiotherapy session. Some may argue it is not a Physiotherapists place to tell patients to take medication. Others may argue that as health professionals we have a role of health promotion and it may be no different to encourging patients to stop smoking.
A lot of this wiki focuses on adult patients with mental health conditions. As Band 5 it may be possible to be involved in paedrtic mental health services. Using NICE Guidelines 2013 for Psychosis and schizophrenia in children and young people: recognition and management, it can be understood that 6 weeks of quetiapine can improve symptoms of psychosis from first onset which is similar to the adult population. Patients can be limited by weight gain, lipid disturbance and raised blood pressure. Long term use of olanzipine in children aged 12-18 years old has the same metabolic effect in adults. Weight gain did seem to be more of a problem for children. there is also an increased risk of getting Diabetes (DMT1). There is a high prevalence of smokers in 12-18 year olds who are taking antipsychotics compared to the general population. From this the challenges may be very similar to the adult population. Health promotion and exercise regiemes may be the best treatment for this patient group. As weight gain is an issue which could lead to body image issues exercise for cardiovasuclar benefit as well as weight management may be recommended.
The Role of the Physiotherapist in Health Promotion[edit | edit source]
The Problem of Poor Health in Schizophrenia[edit | edit source]
It is well documented in the literature that people with schizophrenia have much poorer physical health than the general population and despite having more contact with health services they have a much poorer life expectancy, dying on average 15-20 years earlier. One of the key factors that contributes to the poor physical health in this population is very high rate of physical inactivity and the tendency to adopt a far more sedentary lifestyle than the general population (Lindamer et al. 2008, Janney et al. 2013, Stubbs et al. 2014).
In general, physical inactivity is associated with an array of health risks and is said to be one of the leading causes of long term and secondary conditions such as coronary heart disease, diabetes, obesity and different types of cancers (Booth et al.2012 and Lee et al. 2012). It is important to remember that the same health risks apply to people with schizophrenia but due to the nature of their condition and other influencing factors the risk is much greater (Gorczynski and Faulkner 2010). Along with physical inactivity and sedentary behaviour there are a whole range of other factors that could influence the physical health of people with schizophrenia. These include; antipsychotic medications (as discussed earlier), poor diet, high alcohol intake, high rates of smoking and high rates of substance misuse (Phelan et al. 2001, McCreadie 2003 and Vancampfort et al. 2012). ).Together these factors put people with schizophrenia at much higher risk of developing long term conditions and as such they are 1.5-2 times more likely to be overweight, have a two-fold increased risk of developing diabetes and hypertension and an increased risk of cancer of which they are 50% less likely to survive than the general population (NICE 2014, Vancampfort et al.2012).
The evidence shows that there is great disparity between the physical health of those with schizophrenia and the general population and this ‘problem’ is now becoming widely recognised. We feel it is important to explore the role of the physiotherapist in terms of addressing these modifiable factors that are contributing to poor health whilst also paying special attention to the fact that these people have a mental health condition and recognising that it could be influencing their ability to engage in a healthy lifestyle.
Physiotherapists Perspectives of their Role[edit | edit source]
The role of the physiotherapist and even physiotherapy is often misunderstood within the general population with many people assuming that massages are the only thing we are good for. Just think how many times a family member or friend has said ‘oh I’m a bit sore, do you think you could give me a massage?’ In reality the role of the physiotherapist is much more significant, particularly in relation to mental health.
In general, the key role of physiotherapists and principle of physiotherapy is to ‘help restore movement and function when someone is affected by injury, illness or disability’ (NHS 2014). Physiotherapy is based on science and it requires physiotherapists to take a holistic approach to health and wellbeing – including the patients’ general way of life and it looks to involve the individual as much as possible (CSP 2013).
Looking at the Role in Mental Health
Physiotherapists’ are involved in a variety of different health care specialities but it is only within the last 10-15 years that their role within mental health has become increasingly recognised, not only by the health care system in general, but by the physiotherapists themselves.
Until recently physical care and mental care have been regarded as two separate entities (MHF 2015). However, it is now being acknowledged and accepted that there are links between the two and this is resulting in changes to the way that health care is being delivered. According to the Royal college of Psychiatrists (2013, p.9) “poor mental health is associated with a greater risk of physical health problems and poor physical health is associated with a greater risk of mental health problems.” By acknowledging the connection between physical care and mental care the focus within the NHS is now on how the gaps that currently exist between physical care, social care and mental care can be closed. The Chartered Society of Physiotherapy (CSP) has recognised that physiotherapist’s are perfectly positioned and have the necessary skills to bridge the gap between physical and mental health. ‘Commissioning Mental Health Services’ (2008) is a document that was published by the CSP that looked to provide an overview of the contribution of physiotherapy in the delivery of high quality evidence based mental health and well-being services. This document states that “the physiotherapist as a member of the multidisciplinary team can demonstrate the advantages of harnessing the links between mind and body” (CSP 2008, p.5).
There is a growing body of literature looking at the role of the physiotherapist in mental health however it is limited in regards to looking specifically at schizophrenia. A recent article by Stubbs et al. 2014 is the first to get an international understanding of the role of mental health physiotherapists, from their point of view, with regards to the treatment of people with schizophrenia. This qualitative study involved a secure online survey (which contained open and closed questions) and included 3 sections: demographic information, training and education and the role of the physiotherapist in schizophrenia. 151 physiotherapists from 31 countries, who had on average 10 years of experience in mental health, completed the study but only 115 (76.1%) provided a valid response. From the study emerged two main themes: Physiotherapists felt their role was to be the physical health expert within the MDT and physiotherapists felt they played a crucial role in health promotion for patients with schizophrenia (Stubbs et al. 2014).
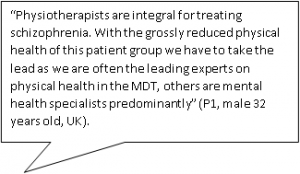
The idea of bringing physical and mental health together was recognised highly amongst physiotherapists. This study found that 41.7% of respondents felt they had a key role in bridging the gap between mental and physical health in this patient population. Due to the qualitative nature of this study it allowed for physiotherapists to give their own view. One respondent said:
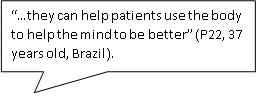
This fits in very well with the patient-centred, holistic approach that physiotherapists are required to take when providing any form of care. Holistic care involves viewing the patient as a whole and considering not only their physical needs but their mental, emotional, social and economic needs (REF). This was another important role established by the physiotherapists in this study – 33.9% felt physiotherapists utilised a “holistic, mind-body approach” when treating patients with schizophrenia. Another participant said:
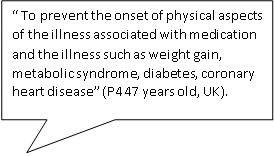
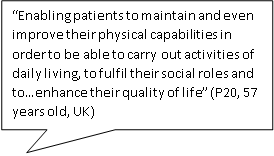
Looking now at the second theme (a vital role in health promotion), 43.5% of participants felt that promoting physical activity and devising individually tailored programmes was a major role. By encouraging more active lifestyles, the physiotherapists recognised that it would help in the management of some of the secondary conditions associated with schizophrenia whilst also having a positive influence on the patient’s mental health and social functioning (Stubbs et al. 2014).
The ‘Commissioning Mental Health Services’ document referred to earlier believes that physiotherapist’s have a key role in “enabling physical activity for health promotion, disease prevention and relapse” and has a major role in providing lifestyle, weight management and well-being programmes (CSP 2008, p.5). It is clear to see that the study conducted by Stubbs et al. (2014) yielded very similar results. This was the first study looking at the international perspectives of the role of physiotherapists in schizophrenia and it concluded that promoting healthy lifestyles and encouraging physical activity as well as bridging the mind-body gap are the key.
A patient centred approach - treatment planning/goal setting[edit | edit source]
A patient centred approach is vital in the management of people with schizophrenia, particularly with regards to treatment planning and goal setting. Autonomy is something that many of us take for granted. In schizophrenia, the combination of positive and negative symptoms as well as side-effects from the medication can result in major changes in a person’s personality and the way they live their life that this independence can often be lost.
The Royal college of Nurses (2015) describes person centred care as care which allows the person to become an equal partner in their care. It encompasses shared decision making and in direct relation to schizophrenia it is about working together to develop treatments and set goals that are meaningful and at a level the person is ready for, willing to and able to achieve (Fogarty and Happell 2005). An article by Stubbs et al. (2014) found that physiotherapists had a role in promoting active lifestyles and designing individually tailored interventions which would enable the patient to stay active in their own environment.
The practice of setting goals is common in mental health rehabilitation and in general case-management (Clarke et al. 2009). The process of goal setting is key to establishing a positive therapeutic relationship and plan (Dopke and Batscha 2014). Working towards achievable and meaningful goals that have been determined collaboratively by both therapist and client can contribute to greater life satisfaction, promote self-management and reduce psychological symptoms. Moreover, attainment of goals improves the emotional and psychological wellbeing of an individual (Clarke et al. 2009).
Clarke et al. (2009) states that the levels of distress due to psychotic symptoms are related to goal progress, with greater symptom distress having a negative impact on the progression of goals. It is likely that this is because whilst symptoms are severe the individuals focus will be on alleviating those distressing symptoms rather than looking towards future goals. This issue highlights the importance of a patient-centered holistic approach where the alleviation of symptoms is targeted whilst also encouraging the attainment of therapeutic goals in order to promote recovery.
Another article by Clarke et al. (2012) discusses the types of goals set by individuals with psychiatric disorders (majority of participants suffered from schizophrenia) depending on the stage of recovery that they were in. This study found that those within early stages of recovery focused more on “avoidance” goals (reducing an undesirable outcome such as hearing voices) whilst those is later stages of recovery showed an increase in setting “approach” goals (moving towards a positive outcome).
Also notable, was that physical health goals were overall reported most frequently. These included adhering to mental health medications, weight loss, increased exercise, improved nutrition and physical fitness. This may be due to these types of goal being practical and clearly defined. It is suggested that when life goals become unachievable, simple daily goals may help keep depression at bay and provide a sense of purpose. There is therefore a higher prevalence of health goals at the early stage of recovery and it is likely that these more concrete initial goals must be at least partially met before the individual feels able to progress to goals associated with relationships, employment and personal development.
Benefits of Physical Activity - The Evidence[edit | edit source]
Barriers to Physical Activity[edit | edit source]
As mentioned earlier, people with schizophrenia spend large periods of their time being sedentary, with the majority failing to meet the physical activity recommendations of 30 minutes per day (REF). As final year physiotherapy students or newly qualified physiotherapists it is important to be aware of any barriers that you may face when trying to promote healthy lifestyles and physical activity in people with schizophrenia.
Before moving onto the next section, take 10-15 minutes and jot down any potential barriers that you can think of. Hint: Consider some of the information that you have already read and think about all of the different factors that could be influencing the patient.
Recent research by Soundy et al. (2014) and Rastad et al. (2014) has looked to establish and explore the factors that could be impacting an individual with schizophrenia’s participation and engagement in physical activity. These two studies take a qualitative approach with one looking at the opinions/experiences of specialist mental health physiotherapists (Soundy et al. 2014) and the other looking at the views and experiences of individuals living with schizophrenia (Rastad et al. 2014)
Analysis of the responses that were collected throughout the two studies generated very similar results. The barriers to physical activity fell, largely, into 3 categories: Physical, psychosocial and environmental.
Physical Barriers
| PATIENT'S PERSPECTIVES(Rastad et al. 2014) | PHYSIOTHERAPIST PERSPECTIVES (Soundy et al. 2014) |
|
Symptoms of Illness and Disease
|
45% - Lack of motivation |
| 27% - Side effects of medication | |
| 21% - Negative Symptoms of Schizophrenia | |
| 19% - Fluctuations in mental and physical health |
It is interesting to see that perspectives of those living with schizophrenia are very similar to those providing care to people with schizophrenia. It would appear that the symptoms of schizophrenia, including both positive (hearing voices) and negative (lack of motivation), play a significant part in stopping individuals engaging in physical activity. Along with this, side effects of medication were identified as a major barrier by 27% of the physiotherapists as well as by the patients themselves (e.g.weight gainand increased appetite).
Psychosocial Barriers
Psychosocial barriers have psychological components and social components. The participants living with schizophrenia had pre-conceived misconceptions regarding physical activity and believed that they had to work at their maximum otherwise it was completely pointless and there was no benefit (Rastad et al. 2014). This was also the opinion of 11% of the physiotherapists who felt a lack of understanding of the benefits of physical activity was a major barrier. Lack of confidence, fear of failure and difficulties interpreting new information and feelings from the body, e.g. increased heart rate as a result of exercise, were other psychosocial barriers identified by individuals living with schizophrenia. Participants admitted that they were afraid to attempt physical activity in case they could not manage or achieve the results they hoped for. One participant said: “If I go on with it without any results, then I’m only going to make myself unhappy because I’m not succeeding…” Similarly low self-esteem and low confidence were identified as barriers by 11% of the physiotherapists in the study.
Personal/environmental Barriers
The finally category of barriers address personal factors and environmental factors. It was reported by a number of participants that they found getting to the exercise sessions or gyms difficult due to transport difficulty arranging or being able to afford transport (Rastad et al. 2014). Linked into this, a number reported having financial difficulties as a result of gambling and as such were unable to afford a gym membership. 10% of the physiotherapists who responded also agreed with this and recognised financial problems as another barrier to engaging in physical activity.
Hopefully this section of the wiki has given you an insight into personal views and experiences of people living with schizophrenia but also the physiotherapists who treat them. There are limitations of these studies: The study by Rastad et al. (2014) was conducted in an outpatient setting with a relatively small number of participants (20) recruited from 3 cities in Sweden. As it was conducted in an outpatient setting only, the results are unlikely to be representative of individuals in in-patient settings. Also, the availability of medical and psychological treatments for patients with schizophrenia varies among countries and as such, the participant’s experiences will not be the same worldwide. The study by Soundy et al. (2014) also had limitations. The analysis assumed that patients were compliant with their medications – non adherence to medication would significantly impact the main barriers that were identified. Also a physiotherapist’s personal habits in regard to PA could influence his/her enthusiasm/effort to promote PA to patients and could have influenced their responses in the survey.
Despite the limitations, a number of clear themes have been identified. Although the results may not be truly generalizable, the barriers identified are vital to consider when trying to promote and develop physical activity programmes or interventions with patients. Both of these studies also addressed potential strategies that could help facilitate engagement in physical activity and they will be discussed briefly in the next section.
Communication strategies[edit | edit source]
Most physiotherapists will, at some point in their career encounter individuals who suffer from a mental health condition (Priestley 2011). It may be that the physiotherapist will be treating another condition, but in order to treat the individual holistically, it is important to understand how this condition may impact the delivery of treatment and require a modified approach (ref?).
A survey conducted by Dandridge et al. (2014) on the views of physiotherapy students towards treating individuals with mental illness, found that one of the key issues was regarding communication. Students raised concerns about how to approach someone with mental illness, discussing a lack of knowledge of how to communicate effectively or adjust their approach to individual needs. The following section will therefore discuss the topic of communication in the context of schizophrenia, including how this condition may impact effective communication and some strategies to help overcome common these barriers.
Barriers to communication[edit | edit source]
Impact of negative symptoms[edit | edit source]
In schizophrenia, while the positive symptoms (hallucinations and delusions) are widely recognised as the hallmarks of the condition, it is the negative symptoms which are harder to treat and are more indicative of the long-term ability of the individual to function in society (Lang et al. 2013). These negative symptoms include poverty of thought and speech, apathy, anhedonia (inability to experience pleasure), lack of motivation and decreased engagement in social interactions (Weinberger and Harrison 2011). These symptoms have a significant impact on how an individual experiences life. They usually exist prior to the emergence of positive symptoms and will often endure long after the psychotic symptoms have disappeared (Staring et al. 2013). Negative symptoms also have implications for physiotherapy treatment as they will affect the client-physiotherapist interactions as well as the ability of the individual to participate actively with their treatment plan.
Deficits in social cognition[edit | edit source]
It has been also identified that individuals may experience deficits in social cognition which can impact their ability to interact socially with others. This can include difficulties with; interpreting facial expressions or tone of voice, recognising the emotions or intentions of others, understanding their own feelings and emotions (Koelkebeck and Wilhelm 2014). Furthermore, a study by Lavelle et al. (2012) on non-verbal communication found that poor social cognition and increased negative symptoms had an adverse impact on social interactions leading participants to perceive poorer rapport when having conversations with individuals suffering from schizophrenia. Interestingly, a higher level of rapport was reported with individuals exhibiting mild positive symptoms, possibly due to these symptoms manifesting as more engagement with the social interaction. As establishing a therapeutic relationship is essential in patient-therapist interactions (Hewitt and Coffey 2005), it is important that these deficits in social cognition are understood and that clinicians engage in strategies to help establish rapport and ensure effective communication is achieved.
Communication skills[edit | edit source]
Approaches to enhance communication: from Pounds 2010[edit | edit source]
A qualitative and descriptive pilot study was carried out to investigate the interaction of an experienced mental health nurse specialist with 3 of her schizophrenic clients. The aim was to describe how she altered her verbal and non-verbal communication in order to enhance effective communication and develop a therapeutic relationship.
Some key approaches that emerged included:
• Exaggeration of facial and vocal cues. As mentioned above, individuals may experience deficits in social cognition, including difficulty reading facial expressions or tone of voice. In this study, the nurse exaggerated her facial expressions (for example, showing concern) or her verbal language (for example, greater inflection in her tone of voice, reflecting a clients’ statement back to them). When applied, these subtle changes in behaviour elicited responses from her clients (such as increased eye contact) and improved their engagement with the interaction.
• Open body language. Displaying open body language, such as leaning forward, smiling and nodding can demonstrate to the client that the clinician is willing to engage with them and can encourage an individual to be involved in the interaction.
• Accepting silence/giving time to answer. Some of the negative symptoms (as mentioned above) that an individual with schizophrenia may face are poverty of thought and speech. This means that when asked a question, a person may require longer to gather their thoughts and give an answer. In her interactions with her clients, there were often periods of silence whilst they were considering a question (lasting between 5-15 seconds).
What can we take from this study?:
The main limitation of this pilot study is that it had an extremely small sample size of three participants and only monitored the behaviour of one clinician, and therefore the results may not be representative of this patient population. However, it does begin to describe what may be some useful but subtle changes to the interactional behaviours of the clinician that could encourage communication and help them connect with their clients (Pound 2010). These strategies, in combination with adequate time to get to know the individual will facilitate the building of trust and help establish a positive therapeutic relationship (Cameron at al. 2005).
Promoting engagement with treatment[edit | edit source]
A-motivation as a key problem[edit | edit source]
Lack of motivation is one of the main negative symptoms experienced by those with schizophrenia (Wienberger and Harrison 2011) and has been identified as having a significant impact on all aspects of behaviour (Choi and Medalia 2010). Motivation is essential for engagement in self-care actions and has an important role in the process of change (Pickens 2012). A qualitative study by Abed (2010) identified lack of motivation to be a major factor that influenced health-related decisions and behaviour. Foussias et al. (2011) conducted a longitudinal study and found that amotivation was responsible for 74% of variance in functional outcomes at baseline and 72% of variance at 6-month follow-up, therefore indicating the motivation has a crucial role in predicting the functional outcomes for individuals with schizophrenia. Addressing motivation is of great importance to promote engagement with change and healthy lifestyle choices within this population (Pickens 2012).
Strategies to enhance motivation[edit | edit source]
Goal setting:
The importance of setting patient centered goals within this population is discussed previously on this physiopedia page. However, it is important to note that working with the client to set personal meaningful goals can help combat amotivation and influence their willingness to be actively involved in their treatment (Dopke and Batscha 2014). Adams and Drake (2006) discuss how individuals with serious mental illnesses are capable of meaningfully participate in decisions about their healthcare and it is therefore important to involve them in the planning of treatment. The setting of patient centered goals is one way in which a sense of control can be returned to the patient and can increase their self-determination (Dopke and Batscha 2014). Progression towards personal goals is also considered to be powerful influencing factor in promoting psychological recovery (Clarke 2009).
Social support:
It has been documented that social interactions can have a positive impact on adherence, enjoyment and motivation to change (Vancampfort et al. 2013), however, individuals with schizophrenia often feel isolated by their condition and have a lack of social support (Soundy et al. 2014). This is due to a number of reasons including paranoia, social skill deficits, social and emotional processing problems, negative symptoms and stigma (Dopke and Batscha 2014). A survey of mental health physiotherapists conducted by Soundy et al. (2014) investigated the common forms of support they utilised to engage people with schizophrenia in physical activity. Forty physiotherapists provided in depth responses and from this four dimensions of social support were identified: Informational, tangible, esteem and emotional support. Examples of each dimension are as follows:
Informational:
• Education on benefits of exercise and exercise prescription.
• Providing information on exercise classes.
• May be verbal or written, other forms include diagrams/drawings (consider signposting to online resources).
• Consider the patients individual needs and how to best communicate with them.
Tangible:
• Providing periods of activity under supervised conditions – staff-run or community-led groups.
• Understand the transition and prepare clients for integration into new environment.
• Incentives to promote attendance – support with costs (e.g. free/reduced admission to fitness facilities, support with transport costs.
• Develop connections with local sports centres so they can support people with schizophrenia.
Esteem support:
• Positive reinforcement – identifying positive changes.
• Praise for even very small achievements.
• Encouragement for every physical activity opportunity.
• Consider psychological theories and models to help provide esteem support – e.g. motivational interviewing, self-efficacy and self-determination.
Emotional support:
• Spend time with and listen to the person.
• Active listening and counselling.
• Develop positive therapeutic relationship.
While the results from this survey may not be representative or generalisable, a number of key themes were seen to emerge. Many of these suggestions may be useful for physiotherapists to consider in order to better support their clients in their recovery (Soundy et al. 2014).
Cognitive Behavioural Therapy[edit | edit source]
Motivational Interviewing[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.