Physiotherapy Management for Sexual Dysfunction in Men
Introduction[edit | edit source]
Sexual dysfunction is defined as a complication occurring in any phase of the sexual response cycle. The phases of the sexual response cycle include; desire, arousal, orgasm, and resolution[1]. Sexual dysfunction is extremely common among women and men, and effective treatment is available. However, few individuals seek help as many, even healthcare professionals, are embarrassed and hesitant to discuss the topic.
Sexual dysfunction, although less common in men, still affects 31% of men and has a large impact on the quality of life as well as interpersonal relationships[2].
Sexual desire/interest, arousal, orgasm, and sexual pain are the four main categories of sexual dysfunction. Sexual dysfunction may include; Sexual desire dysfunctions (Sexual aversion disorder), Sexual arousal dysfunctions, Erectile dysfunction, Premature ejaculation, Anejaculation (inability to ejaculate), Orgasmic dysfunction, Priapism (persistent and painful erection of the penis), and Peyronie’s disease (a bent, rather than straight, erect penis due to scar tissue)[3].
Erectile dysfunction ( 5–20% of men) and premature ejaculation (20–30% of men) are the most common male sexual dysfunctions[4].
Risk factors[edit | edit source]
- Psychological complications (eg. depression)
- Biological complications (hormonal, neurologic, and/or vascular)
- Increase with age
- Prostate cancer
- Chronic prostatitis/chronic pelvic pain syndrome[5]
Anatomy & Physiology[edit | edit source]
Bony structures[edit | edit source]
Pelvic cavity;
- Sacrum & coccyx
- Left and Right innominate bones (ilium, ischium & pubis)
- Pectineal line
- Pubic crest[5]
Musculature[5][edit | edit source]
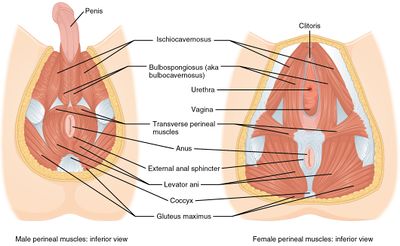
The pelvic floor consists of 3 layers;
Most superficial layer
- bulbospongiosus m.
- ischiocavernosus m.
- superficial transverse perineal m.
- external anal sphincter
The second layer (the urogenital diaphragm)
- deep transverse perineal,
- sphincter urethrae,
- compressor urethrae
Assist with urethral closure during raised intra-abdominal pressure & plays a role in stabilising the pelvis and lumbar joints.
The third layer (the pelvic diaphragm)
- Levator ani (Pubococcygeus & Ischiococcygeus)
- Iliococcygeus,
Contraction of the Levator ani muscles maintain anal continence when contracted and allow the evacuation of bowel when relaxed. It also supports the pelvic organs.
The obturator internus muscle does not form part of the pelvic floor muscles but still has an effect on the elevation of pelvic organs.
The pelvic floor muscles form a dome-shaped structure that enclose the pelvic cavity.
The functions of the pelvic floor muscles include;
- Stabilising pelvic joints
- Support internal pelvic organs
- Voluntary contraction of urethral and anal sphincters
- Regulate erection, emission and ejaculation
- Controls continence (urinary & fecal)
Innervation[5][edit | edit source]
The innervation of pelvic floor muscles is from sympathetic, parasympathetic, and somatic nerve fibres.
Nerves responsible for pelvic floor functioning;
- Hypogastric nerve
- Pudendal nerve
- Levator ani nerve
Physiotherapy Management[edit | edit source]
Treatment[edit | edit source]
Studies indicate that pelvic floor muscle training is effective in treating erectile dysfunction, ejaculation complications and chronic pelvic pain.
Common complications and relevance to Physiotherapy[5][edit | edit source]
Erectile Dysfunction
Literature has indicated that between 9-40% of men struggle with erectile dysfunction by age 40 and raises 10% each decade after 40. Erectile dysfunction is defined as the inability to either obtain and/or maintain a rigid erection sufficient for penetration.
The muscles responsible for erection are; the bulbospongiosus and ischiocavernosus muscles. Strengthening voluntary contraction of the ischiocavernosus muscle relaxation techniques in cases of high pelvic floor muscle tone (spasms or increased tone may prevent adequate blood flow necessary for erection) have been proven to be an effective treatment.
Ejaculatory Dysfunction
During ejaculation there occurs contraction of the smooth muscles of the prostate gland and the bladder neck, as well as relaxation of the urethral sphincter.
The muscle responsible for ejaculation is the bulbospongiosus muscle. As premature ejaculation is among the most common sexual dysfunction cases in men, pelvic floor therapy are proven to improve control and latency times. Behavioural changes are also beneficial and include; pre-intercourse masturbation, frequent sexual activity or stopping intercourse intermittently with sustained contraction/ internal squeeze.
Chronic Prostatitis/ Chronic Pelvic Pain Syndrome
Chronic Prostatitis/ Chronic Pelvic Pain Syndrome is defined as pelvic -, abdomen - and genital pain without symptoms of urinary tract infection. This most commonly occurs during or after ejaculation.
Motor control exercises emphasising on the relaxation of levator ani muscles (if increased tone is present) and coordinated activation-deactivation exercises with biofeedback methods are an extremely beneficial treatment for men with Chronic Prostatitis/ Chronic Pelvic Pain Syndrome.
Soft tissue mobs, myofascial release and manipulation are also beneficial if the physiotherapist has undergone adequate and specialised training.
.
References[edit | edit source]
- ↑ deGROAT WC, BOOTH AM. Physiology of male sexual function. Annals of internal medicine. 1980 Feb 1;92(2_Part_2):329-31.
- ↑ Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Current psychiatry reports. 2000 Jun 1;2(3):189-95.
- ↑ Hatzimouratidis K, Hatzichristou D. Sexual dysfunctions: classifications and definitions. The journal of sexual medicine. 2007 Jan;4(1):241-50.
- ↑ Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, Vardi Y, Wespes E. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. European urology. 2010 May 1;57(5):804-14.
- ↑ 5.0 5.1 5.2 5.3 5.4 Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.